11 Ebstein’s Anomaly
I. CASE
A. Fetal echocardiography findings
1. The fetal echo reveals situs solitus of the atria, levocardia, left aortic arch, and heart rate of 112 bpm.
2. There are frequent conducted and nonconducted premature atrial beats (PACs), abnormal cardiac axis (left), and massive cardiomegaly (cardiothoracic ratio = 0.55).
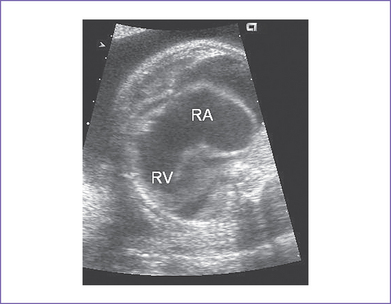
3. The four-chamber view reveals marked dilation of the right atrium (RA) and atrialization of the right ventricle (RV) (Fig. 11-1).
4. The septal and posterior leaflets of the tricuspid valve are displaced into the RV cavity (the essence of Ebstein’s malformation).
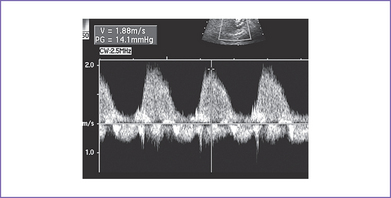
5. There is 4+ tricuspid valve regurgitation with peak velocity of 3.3 m/s and a decreased dP/dt (change in pressure per change in time) of 550 mm Hg per second (Fig. 11-2).
6. The pulmonary valve is atretic and the proximal main pulmonary artery is severely hypoplastic, with reversal of flow in the ductus arteriosus (aorta to pulmonary).
7. The branch pulmonary artery Doppler velocity is decreased, with a negative response to the maternal hyperoxygenation test, suggesting severe pulmonary hypoplasia and pulmonary arteriolar underdevelopment.
8. The left ventricle (LV) is compressed by the dilated atrialized RV.
9. The LV outflow tract is normal, as are the aortic Doppler flow values, pattern, and velocity through it.
10. The aortic arch is leftward and the ductal and aortic arches are of similar size.
11. The flow though the aortic arch is antegrade, and flow through the ductal arch is retrograde, filling the pulmonary arteries.
12. The foramen ovale is large and patent, and the flow is unrestricted and mainly right to left.
13. The pulmonary venous flow pattern is normal.
14. The RV Tei index (myocardial performance index) is elevated (0.6) and the LV Tei index is normal.
D. Fetal management and counseling
The baby has a severe form of congenital heart disease combining Ebstein’s malformation of the tricuspid valve with massive tricuspid regurgitation and pulmonary atresia. There is a 10% to 15% chance for the baby to survive after birth, assuming a term delivery with normal chromosomes and no other abnormalities present. With hydrops and low peak velocity of the tricuspid valve regurgitation, the prognosis is poor (see Fig. 11-2).
1. Amniocentesis could not be offered at this gestation, and it is usually not productive in this lesion.
a. Parents should be aware that the disease can progress to a more severe form.
b. Serial antenatal fetal echocardiography studies are performed at weekly intervals.
c. Consider treatment with digoxin to support the LV function and attempt to prevent catecholamine excess.
E. Delivery
1. If the fetus remains well compensated, normal vaginal delivery can occur at term in a tertiary care center.
2. The true degree of pulmonary stenosis (atresia) after birth and after ductus arteriosus closure may be difficult to predict.
3. In the presence of heart failure or hydrops, delivery should be by cesarean section, which will in effect add the risk of prematurity to that of severe circulatory failure in a fetus already endangered by a major cardiac malformation.
4. Parents should be made aware that if the fetus survives to delivery, the risk of neonatal mortality is high because many of these babies cannot be adequately ventilated.
F. Neonatal management
b. General treatment, especially for anatomical pulmonary atresia.
c. Closure of ductus arteriosus for functional pulmonary atresia.
d. Congestive heart failure (CHF) requires anticongestive measures with digoxin and diuretics.
a. Indications for surgical intervention vary from one institution to the other. Common indications for surgery include:
b. There is controversy concerning the surgical procedure of choice.
c. Palliative and corrective options.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree