Early readmissions (ERs) impose a huge cost to the health care system, lower patients’ quality of life, and may be an indicator of quality of initial care. We performed this single-center study to assess the incidence, predictors, and implications of 30-day readmission after percutaneous coronary intervention (PCI) in a tertiary care rural setting. In 4,262 consecutive patients who underwent PCI, we evaluated 30-day readmission rates and assessed demographic, clinical, and angiographic correlates of ER. Using Cox regression analyses, we estimated the multivariable impact of an ER on 1-year all-cause mortality and major adverse events (MACEs; death, myocardial infarction, target vessel revascularization, stent thrombosis). ER occurred in 486 patients (11.4%) including 366 (8.6%) for cardiac reasons and 120 (2.8%) for noncardiac reasons. Multivariable models predicting any readmission, cardiac readmission, and noncardiac readmission had c-statistic values of 0.63, 0.63, and 0.68, respectively. One-year mortality and MACEs were higher in the readmitted versus not readmitted patients (7.9% vs 3.2%, 18 vs 9.7%, p <0.0001 for the 2 comparisons). ER had a significant and independent impact on 1-year mortality (adjusted hazards ratio 2.2, 95% confidence interval 1.4 to 3.4) and MACEs (hazards ratio 2.2, 95% confidence interval 1.8 to 2.8). In conclusion, readmission within 30 days after PCI is common and frequently related to cardiac causes. Patients who require an ER after PCI have higher 1-year mortality and MACEs.
The incidence and factors associated with early readmissions (ERs) after hospitalization for heart failure have been widely studied. The frequency and predictors of readmission after percutaneous coronary intervention (PCI) are less well examined. An estimated 1.27 million PCI procedures were performed in the United States in 2006. Recent studies have reported 30-day readmission rates of 10% to 16% after an index PCI procedure. Much of the existing literature on readmission after PCI is derived from administrative data from Medicare databases. Little current data exist on readmission rates after PCI in a tertiary care rural setting. We performed this analysis to understand the incidence, demographic, clinical, and angiographic correlates and prognostic impact of ERs occurring within 30 days after PCI in a rural tertiary care center.
Methods
The Guthrie Health Off-label Stent (GHOST) Registry is a single-center prospective observational database funded by the Guthrie Health Foundation. We prospectively collect baseline clinical and angiographic characteristics, laboratory values, and in-hospital outcomes (death, myocardial infarction [MI] after PCI, and target vessel revascularization [TVR]) performed in all patients who undergo PCI at the Robert Packer Hospital (Sayre, Pennsylvania). After hospital discharge, we collect information on occurrence of death, MI, and TVR annually for ≥5 years or until the occurrence of a major adverse cardiovascular event (MACE; defined as composite of death, MI, or TVR) by reviewing patient medical records and/or telephone contact with the patient or family. A qualified registered nurse with clinical cardiology experience performs these data collection. Long-term survival follow-up in all patients is also obtained using the Social Security Death Index. This index has previously been shown to be highly accurate. To further ensure accuracy, we compare the mortality data from this index to that obtained from clinical follow-up. Inconsistencies between the Social Security Death Index and clinical follow-up data are resolved by carefully reviewing a patient’s medical records. The institutional review board approved the conduct of this study.
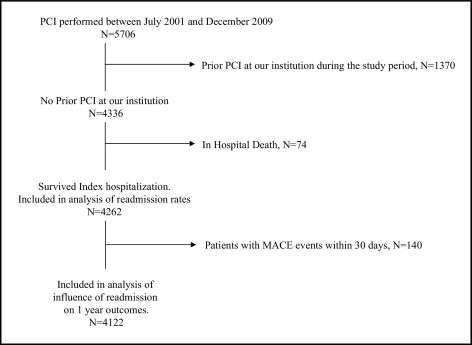
From July 2001 through December 2009, 5,706 patients underwent PCI at our hospital. We excluded 1,370 patients who had previous PCI at our institution during the study period and 74 patients who did not survive their initial hospital stay. Thus, 4,262 PCIs were included in this analysis for assessment of the frequency and correlates of readmission. To evaluate the influence of ER on subsequent 1-year outcomes (31 to 365 days after PCI), we excluded 140 patients who developed any MACE within 30 days after PCI. Inclusion and exclusion criteria are shown in Figure 1 .
We assessed the incidence of ER, defined as readmission for any reason within 30 days after PCI. Patients were classified into an ER group and a no-ER group, respectively, depending on whether they were readmitted or not during the 30 day period after the index PCI. This assessment was based on retrospective review of chart records and telephone calls to patients or next of kin. Whenever an ER to another hospital was reported by the patient or chart review, we obtained medical records from the other hospital to define the cause of ER. We classified ERs as those related to cardiac causes or noncardiac causes based on review of the discharge summary of the readmission. Cardiac ERs were those where the primary discharge diagnosis was unstable angina, MI, repeat revascularization, heart failure, ventricular or atrial arrhythmia, heart block, and/or conduction disturbances. ERs for all other causes were considered noncardiac.
One-year MACE was defined as any MACE occurring 31 to 365 days after PCI. For this part of the analysis, we excluded 140 patients (3.3%) who had a MACE in the first 30 days after PCI (82 of 3,776 patients [2.2%] in the no-ER group and 58 of 486 patients [12%] in the ER group).
Baseline characteristics are described as mean ± 1 SD (median) for continuous variables and percentage for categorical variables. Differences in baseline characteristics between the ER and no-ER groups were compared using contingency tables and chi-square tests (categoric variables) and unpaired t test or Mann–Whitney U test (continuous variables). To estimate the impact of demographic, clinical, and angiographic variables on occurrence of any cause for ER, we performed multiple logistic regression analysis. All variables with a univariable relation (p <0.10) with any cause for ER were included in the initial model. We started with the following variables: gender, age, body surface area, diabetes mellitus, cerebrovascular disease, peripheral vascular disease, hypertension, previous MI, nonelective indication for PCI, left anterior descending coronary artery PCI, American College of Cardiology/American Heart Association lesion type C, postlesion length >28 mm, intra-aortic balloon pump use during PCI, decreased left ventricular ejection fraction (<35%), use of low-dose (<325 mg/day) versus high-dose (325 mg/day) aspirin after PCI, and use of any proton pump inhibitor after PCI. Variables were eliminated using backward stepwise selection until only those variables that had a significant relation to ER remained. Multivariable odds ratios and 95% confidence intervals (CIs) were estimated for each variable in the final model. Similar analyses were then conducted to estimate multivariable correlates of ER for cardiac cause and ER for noncardiac cause.
To estimate the independent effect of any ER on 1-year death, Cox proportional hazards regression analysis was performed. In addition to ER, those variables with a univariable relation to 1-year death (p <0.10) were included in the first step of the model. ER was kept in the final model irrespective of its statistical significance. Adjusted hazards ratios (HRs) and 95% CIs were estimated for each variable in the final model. We conducted similar multivariable analyses to estimate the independent effect of ER on 1-year MACEs.
Results
ERs occurred in 486 patients (11.4%) including 366 (8.6%) for cardiac causes and 120 (2.8%) for noncardiac causes. Clinical and angiographic characteristics of the 2 study groups are listed in Tables 1 and 2 . The ER group had a smaller body surface area, was more likely to be women, have underlying co-morbid conditions, and require PCI on a nonelective basis. In addition, the ER group was less likely to undergo PCI of the left anterior descending coronary artery but more likely to undergo PCI of type C lesions, long lesions (>28-mm length), have low left ventricular ejection fraction, and require intra-aortic balloon pump during PCI. Data on medications prescribed at time of release from the hospital are listed in Table 3 . The number of ERs occurring on each of the 30 days after discharge after the index PCI are shown in Figure 2 .
| Characteristic | ER | p Value | |
|---|---|---|---|
| No | Yes | ||
| (n = 3,776) | (n = 486) | ||
| Women | 1,124 (30%) | 185 (38%) | 0.0002 |
| Age (years) | 65 ± 12 | 65 ± 11 | 0.13 |
| Body surface area (m 2 ) | 2.12 ± 5.03 | 1.99 ± 0.26 | 0.036 |
| Procedure urgency ⁎ | 138 (28%) | 0.0002 | |
| Elective | 1,420 (38%) | 127 (26%) | |
| Emergency | 799 (21%) | 2 (0.4%) | |
| Salvage | 4 (0.1%) | 219 (45%) | |
| Urgent | 1,553 (41%) | ||
| Nonelective procedure | 2,356 (62%) | 348 (72%) | <0.0001 |
| Diabetes mellitus | 1,027 (27%) | 156 (32%) | 0.023 |
| Cerebrovascular disease | 312 (8.3%) | 60 (12%) | 0.003 |
| Peripheral vascular disease | 418 (11%) | 84 (17%) | <0.0001 |
| Current smoker | 1,008 (27%) | 121 (25%) | 0.40 |
| Hypertension † | 2,546 (67%) | 349 (72%) | 0.051 |
| Dyslipidemia ‡ | 2,763 (73%) | 363 (75%) | 0.48 |
| Previous percutaneous coronary intervention | 692 (18%) | 80 (16%) | 0.31 |
| Previous coronary bypass surgery | 613 (16%) | 93 (19%) | 0.11 |
| Previous myocardial infarction | 756 (20%) | 119 (24%) | 0.022 |
| Myocardial infarction at presentation | 1,585 (42%) | 221 (45%) | 0.14 |
| Non–ST-segment elevation myocardial infarction | 822 (22%) | 119 (24%) | 0.17 |
| ST-segment elevation myocardial infarction | 763 (20%) | 102 (21%) | 0.69 |
| Baseline glomerular filtration rate (ml/min) | 103 ± 74 | 114 ± 119 | 0.90 |
⁎ Procedural urgency was defined according to American College of Cardiology/National Cardiovascular Data Registry 2.0b. An urgent procedure is performed on an inpatient basis and before discharge because of significant concerns of risk of ischemia, infarction, and/or death. An emergency procedure is performed as soon as possible because of substantial concerns that ongoing ischemia and/or infarction could lead to death. A salvage procedure is situation in which the patient is undergoing cardiopulmonary resuscitation en route to the cardiac catheter laboratory or before the procedure.
† Hypertension was defined as ≥1 of the following: history of hypertension diagnosed and treated with medication, diet, and/or exercise; systolic blood pressure >140 mm Hg or diastolic blood pressure >90 mm Hg on ≥2 occasions; and/or currently on antihypertensive pharmacologic therapy.
‡ Dyslipidemia was defined as ≥1 of the following: total cholesterol >200 mg/dl, low-density lipoprotein cholesterol ≥130 mg/dl, high-density lipoprotein cholesterol <30 mg/dl, triglycerides >150 mg/dl, and/or ongoing treatment with lipid-lowering medications.
| Angiographic Characteristic ⁎ | ER | p Value | |
|---|---|---|---|
| No | Yes | ||
| (n = 3,776) | (n = 486) | ||
| Lesion in graft | 228 (6.1%) | 38 (7.9%) | 0.12 |
| Lesion in left anterior descending coronary artery | 1,386 (37%) | 146 (30%) | 0.004 |
| Multivessel percutaneous coronary intervention | 467 (12%) | 72 (15%) | 0.13 |
| Lesion risk C | 1,614 (43%) | 235 (48%) | 0.019 |
| Lesion length >28 mm ⁎ | 449/3,613 (12%) | 77/465 (17%) | 0.012 |
| Stenosis before percutaneous coronary intervention (%) † | 90 ± 10 | 90 ± 11 | 0.33 |
| Stenosis after percutaneous coronary intervention (%) † | 7.8 ± 66 | 5.0 ± 19 | 0.24 |
| Thrombolysis In Myocardial Infarction flow before percutaneous coronary intervention ⁎ | 0.90 | ||
| Patients | 3,315 | 424 | |
| 0 | 535 (16%) | 69 (16%) | |
| 1 | 140 (4.2%) | 18 (4.3%) | |
| 2 | 418 (13%) | 48 (11%) | |
| 3 | 2,222 (67%) | 289 (68%) | |
| Thrombolysis In Myocardial Infarction flow after percutaneous coronary intervention ⁎ | 0.042 | ||
| Patients | 3,294 | 424 | |
| 0 | 31 (0.9%) | 7 (1.7%) | |
| 1 | 11 (0.3%) | 2 (0.5%) | |
| 2 | 50 (1.5%) | 1 (0.2%) | |
| 3 | 3,202 (97%) | 414 (98%) | |
| Stent type | 0.26 | ||
| Drug eluting ‡ | 1,981 (53%) | 247 (51%) | |
| Bare metal | 1,544 (41%) | 197 (41%) | |
| No stent | 251 (6.7%) | 42 (8.6%) | |
| Final vessel diameter (mm) ⁎ † | 3.13 ± 0.53 | 3.15 ± 0.58 | 0.79 |
| Patients | 3,635 | 459 | |
| Left ventricular ejection fraction <40% ⁎ | 743 (21%) | 120 (26%) | 0.014 |
| Patients | 3,561 | 464 | |
| Intra-aortic balloon pump used during percutaneous coronary intervention | 235 (6.2%) | 46 (9.5%) | 0.007 |
⁎ Lesion-specific data were not available in all patients.
‡ Includes patients who received drug-eluting stents alone or in conjunction with bare-metal stents.
| Medication Class | ER | p Value | |
|---|---|---|---|
| No | Yes | ||
| (n = 3,776) | (n = 486) | ||
| Aspirin | 3,681 (98%) | 470 (97%) | 0.28 |
| Low-dose aspirin (<325 mg) | 532 (14%) | 89 (18%) | 0.013 |
| Duration of dual antiplatelet therapy (months) ⁎ | 11 (2–21) | 11 (2–19) | 0.62 |
| Patients | 3,571 | 483 | |
| Angiotensin-converting enzyme inhibitor or angiotensin receptor blocker | 2,896 (77%) | 369 (76%) | 0.69 |
| β Blocker | 3,164 (84%) | 414 (85%) | 0.45 |
| Statin | 3,420 (91%) | 431 (89%) | 0.17 |
| Proton pump inhibitor | 1,026 (27%) | 174 (36%) | <0.0001 |
| Warfarin | 339 (9.0%) | 44 (9.1%) | 0.96 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


