Duplex Evaluation of Lower Extremity Arterial Occlusive Disease
Gregory L. Moneta
Molly J. Zaccardi
Arterial duplex scanning provides detailed anatomic and hemodynamic information from the abdominal aorta to the distal tibial vessels that cannot be obtained by indirect physiologic testing. A prospective comparison of arterial duplex scanning with angiography has established standard criteria for normal and diseased arteries.1 The sensitivity of duplex scanning for detecting the presence of a hemodynamically significant lesion (≥50% diameter reduction) ranges from 89% at the iliac artery to 68% at the popliteal artery. Overall sensitivities for predicting interruption of patency are 90% for the anterior and posterior tibial arteries and 82% for the peroneal artery. This method is versatile and does not appear to be significantly influenced by the presence of previous operations or multilevel disease.
INSTRUMENTATION
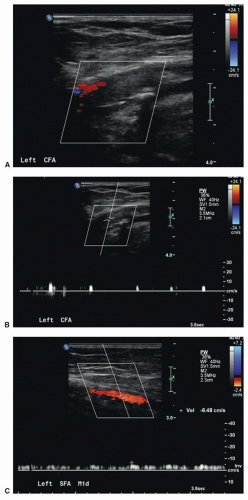
A standard duplex ultrasound system with high-resolution B-mode imaging, pulsed Doppler spectral waveform analysis, and color-flow imaging is adequate for lower extremity arterial scanning. Color-flow imaging facilitates the duplex examination by aiding in the rapid identification of arteries and decreasing the overall time required, particularly in the iliac, popliteal trifurcation, and tibial arteries. Color flow also helps in determining the length of an occlusion and distal sites of reconstitution (Fig. 12.1). However, color flow cannot be used to quantify percent stenosis, and the detailed classification of disease severity is based on analysis of Doppler spectral waveforms.2
A variety of transducers is needed for a complete lower extremity arterial duplex examination. Low-frequency (2- or 3-MHz) transducers are best for evaluating the iliac arteries, whereas a higher frequency (5-MHz) transducer is adequate in most patients for the infrainguinal vessels. In general, the highest frequency transducer that provides adequate depth penetration should be used. As for other applications of arterial duplex scanning, Doppler angle correction is important when examining the peripheral arteries. Although 60 degrees is generally regarded as “ideal,” angles between 30 and 70 degrees are sufficient to provide clinically accurate information.3
EXAMINATION TECHNIQUE
A complete lower extremity arterial duplex examination includes the abdominal aorta; the common and external iliac arteries; the common femoral artery; the profunda femoris artery origin; the proximal, middle, and distal superficial femoral artery; the popliteal artery; and the tibial arteries. Examining patients after a fast of 8 to 12 hours facilitates examination of the intra-abdominal vessels. A complete duplex study in a patient with complicated arterial anatomy may require from 1.0 to 1.5 hours.
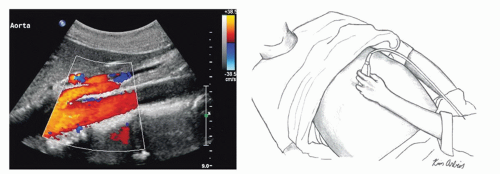
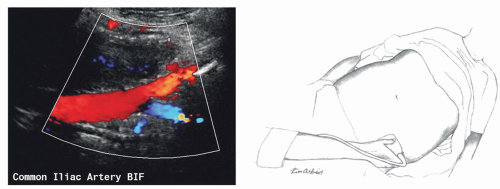
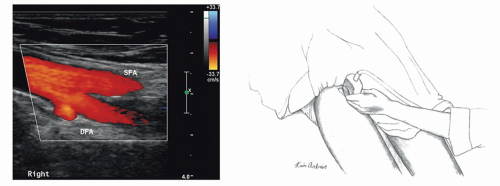
The examination begins with the abdominal aorta. With the patient in the supine position, a low-frequency transducer is placed below the xiphoid process and angled cephalad (Fig. 12.2). The proximal abdominal aorta can be seen in long axis with visualization of the origins of the celiac trunk and superior mesenteric artery. This aortic segment is evaluated by both B-mode imaging and pulsed Doppler. The transducer is then angled caudad and moved inferiorly to evaluate the distal abdominal aorta. The aortic bifurcation is visualized by placing the transducer at the level of the umbilicus and using an oblique approach from the patient’s left side (Fig. 12.3). It is important to sweep the pulsed Doppler sample volume slowly through the distal aorta and proximal common iliac arteries to detect stenotic lesions. The transducer is placed at the level of the iliac crest to evaluate the middle to distal common iliac and proximal external iliac arteries (Fig. 12.4). This usually requires applying considerable probe pressure. In many cases, the internal iliac artery can also be evaluated from this approach. The internal iliac artery is used as a landmark to separate the common iliac from the external iliac artery.
Next, a higher-frequency transducer is placed in the groin and pointed in a cephalad direction to assess the distal external iliac and common femoral arterial segments (Fig. 12.5). The transducer is moved distally down the leg to identify the origins of the profunda femoris and superficial femoral arteries. The profunda femoris artery is normally evaluated for the first 3 or 4 cm, at which point it begins to descend more deeply into the thigh. Attention then turns back to the superficial femoral artery, which is followed down to the level of the knee. When the superficial femoral artery passes through
Hunter’s canal, it assumes a deeper position that may make it difficult to assess with the patient supine. At this point, the patient may need to be placed in the prone position to assess the distal superficial femoral and popliteal arteries. As the popliteal artery is scanned in a longitudinal view, the first branch vessel to be encountered is usually the anterior tibial artery.
Hunter’s canal, it assumes a deeper position that may make it difficult to assess with the patient supine. At this point, the patient may need to be placed in the prone position to assess the distal superficial femoral and popliteal arteries. As the popliteal artery is scanned in a longitudinal view, the first branch vessel to be encountered is usually the anterior tibial artery.
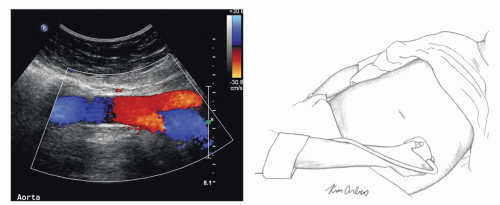 FIGURE 12.3. The transducer is positioned obliquely from the left side at the level of the umbilicus to visualize the distal aorta and proximal common iliac arteries. |
After the origin of the anterior tibial artery has been identified and interrogated, the technologist places the transducer at the level of the ankle, posterior to the medial malleolus, to visualize the posterior tibial artery (Fig. 12.6). It is possible to follow the posterior tibial artery throughout its entire length up to and including the bifurcation of the tibial-peroneal trunk in the proximal calf. The adjacent paired veins help identify the tibial and peroneal arteries. After scanning the length of the posterior tibial artery, the transducer is placed posterior to the lateral malleolus to assess the distal peroneal artery. Sliding the transducer proximally, the entire length of the peroneal artery is evaluated. Finally, with the transducer placed anteriorly on the ankle, it is possible to follow the anterior tibial artery up to the level at which it penetrates the interosseous membrane to reach its origin from the popliteal artery.
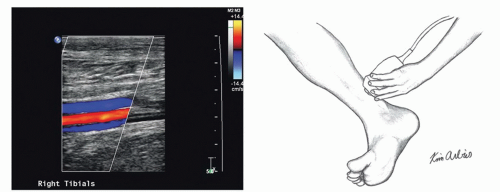 FIGURE 12.6. The transducer is placed at the level of the ankle, posterior to the medial malleolus, to visualize the posterior tibial artery between the adjacent paired veins. |
Velocities should be routinely recorded from specified sites and from any site at which a flow disturbance is identified. Areas of both high velocity (suggestive of a hemodynamically significant stenosis) and low velocity (indicating a more proximal stenosis or occlusion) should be noted. Table 12.1 lists expected blood flow velocities from normal lower extremity arterial segments.
CLASSIFICATION OF STENOSIS
As discussed in Chapter 13, flow waveforms from normal resting lower extremity arteries are triphasic, and end-diastolic flow velocity is near the zero baseline, reflecting the high end-organ resistance associated with the peripheral circulation.
This triphasic waveform pattern is maintained throughout the length of the lower extremity, but peak systolic velocity (PSV) decreases from the iliac to the tibial vessels (see Table 12.1). There are no significant differences in velocity measurements among the three tibial/peroneal arteries in normal subjects.
This triphasic waveform pattern is maintained throughout the length of the lower extremity, but peak systolic velocity (PSV) decreases from the iliac to the tibial vessels (see Table 12.1). There are no significant differences in velocity measurements among the three tibial/peroneal arteries in normal subjects.
TABLE 12.1 BLOOD FLOW VELOCITIES IN NORMAL LOWER EXTREMITY ARTERIAL SEGMENTS AS MEASURED DURING DUPLEX SCANNING | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree