Duplex Assessment of Aortic Endografts
Nasim Hedayati
David Del Pizzo
David L. Dawson
Parodi and coworkers1,2 first reported successful exclusion of an abdominal aortic aneurysm (AAA) by an intraluminal graft in 1991. Since that time, the increased use of endovascular aneurysm repair (EVAR) has led to a decrease in traditional open surgical repair, and currently, nearly 75% of all AAAs are being treated via an endovascular approach.3,4,5,6 Advantages of EVAR include shorter operative time and hospital length of stay, as well as lower perioperative morbidity and mortality compared with those of traditional open AAA repair.6,7,8,9 However, late complications such as aneurysm sac enlargement, endoleaks, stent fracture, endograft migration, and stenosis or occlusion of the iliac graft limbs make lifelong endograft surveillance a necessity.10
Surveillance can identify conditions that might represent a risk for aneurysm growth and rupture, such as an endoleak with continued pressurization of the aneurysm sac. Post-EVAR follow-up has traditionally been performed with computed tomography (CT), which has been the “gold standard” for surveillance designed to evaluate aneurysm sac size and detect endoleaks. Follow-up schedules have generally reflected the protocols developed in the clinical trials of EVAR, with postprocedure surveillance CT scans being performed at approximately 1 month, 6 months, 12 months, and annually thereafter.
CT imaging and duplex ultrasonography are the two primary post-EVAR surveillance methods currently being used. Other imaging modalities, such as magnetic resonance angiography (MRA), are rarely used for EVAR surveillance, but the use of duplex ultrasound for the evaluation of abdominal aortic endografts has been gaining wider acceptance. At many institutions, including our own, a duplex ultrasound is performed after the initial post-EVAR CT scan. Subsequent CT imaging is reserved for confirming aneurysm sac enlargement or delineation of an endoleak. An endoleak is defined as blood flow outside the lumen of the endograft or in the aneurysm sac, and it is identified in 15% to 32% of all patients who undergo an EVAR.11,12,13,14,15 An increasing number of studies have compared duplex ultrasound to CT angiography for detecting endoleaks and measuring aneurysm sac diameter. As discussed in this chapter, the efficacy, feasibility, and financial advantages of duplex ultrasonography in comparison with CT angiography for post-EVAR surveillance are well documented.16,17,18,19,20,21,22,23,24,25,26,27,28,29
THE ROLE OF SURVEILLANCE AFTER EVAR
One of the most important features of successful aneurysm treatment by EVAR is the absence of an endoleak. Although approximately 50% of all endoleaks will thrombose or resolve spontaneously without intervention,14 the presence of an endoleak is concerning owing to the possibility of aneurysm sac enlargement and the potential risk for rupture. In addition, endoleak management can greatly increase the overall cost of an EVAR. One estimate of the 5-year postplacement follow-up cost for a patient with an endoleak was $26,739 versus $5706 for a patient without an endoleak.30 This nearly fivefold increase in cost is associated with the secondary interventional procedures and additional imaging studies.
Classification of Endoleaks
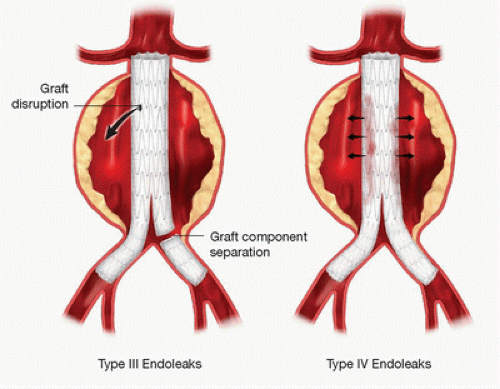
Endoleaks are classified according to the source of the leak, as illustrated in Figures 16.1 and 16.2. A type I endoleak (see Fig. 16.1, Left) represents blood flow into the aneurysm sac from the proximal graft attachment site at the infrarenal neck of the aortic aneurysm (type Ia) or the distal attachment site in the iliac arteries (type Ib). Type I endoleaks have been reported in 4% to 7% of all EVARs.9 If recognized intraoperatively or during postoperative surveillance, type Ia endoleaks can often be treated successfully with balloon angioplasty to better appose the graft to the aortic wall, deploying a proximal aortic cuff, or using a balloon-expandable stent to provide additional proximal fixation and seal. An iliac limb extension can be used to provide a better distal seal for type Ib endoleaks. A persistent type I endoleak not amenable to repair by endovascular techniques may require conversion to open repair.
A type II endoleak results from retrograde flow into the aortic sac from aortic branches such as one or more lumbar arteries, the inferior mesenteric artery, or other collateral vessels (see Fig. 16.1, Right). Type II endoleaks are relatively common and have been observed in 27% to 37% of EVAR cases.11 Some have subcategorized type II endoleaks into type IIa, indicating flow from one branch vessel, and type IIb, representing more than one branch vessel involvement.11 Others have
described a type IIa endoleak as originating from the inferior mesenteric artery and a type IIb as originating from a lumbar artery. To avoid confusion, it may be better to report the presence of a type II endoleak and specifically describe the branch vessel(s) responsible. Most type II endoleaks can be followed without intervention, because many will resolve spontaneously by thrombosis.14 Interventions such as coil embolization or vessel ligation are performed when the type II endoleak is associated with evidence of aneurysm sac enlargement or failure of a large aneurysm sac to shrink over time.
described a type IIa endoleak as originating from the inferior mesenteric artery and a type IIb as originating from a lumbar artery. To avoid confusion, it may be better to report the presence of a type II endoleak and specifically describe the branch vessel(s) responsible. Most type II endoleaks can be followed without intervention, because many will resolve spontaneously by thrombosis.14 Interventions such as coil embolization or vessel ligation are performed when the type II endoleak is associated with evidence of aneurysm sac enlargement or failure of a large aneurysm sac to shrink over time.
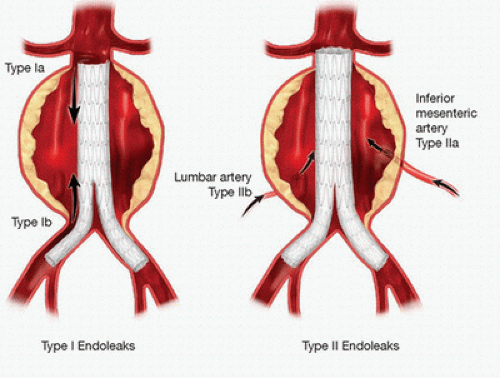 FIGURE 16.1. Left, Type I endoleaks after endovascular aneurysm repair (EVAR). Right, Type II endoleaks. |
A type III endoleak originates from a structural failure of the stent graft, such as a fabric tear or ineffective seal between stent graft components; these occur in less than 3% of cases (see Fig. 16.2, Left).12 Although rare, the presence of a type III endoleak is an indication for intervention by either endovascular revision or open repair because the aneurysm sac is exposed to systemic arterial pressure, and the risk of aneurysm rupture is similar to that with a type I endoleak (or an unrepaired aneurysm). Type III endoleaks can also be subcategorized into type IIIa, indicating device fabric disruption or holes; type IIIb, separation of modular component devices or junctions; and type IIIc, representing suture holes in the fabric of the graft.11
The final endoleak classification is type IV, which is a consequence of graft porosity (see Fig. 16.2, Right). Type IV endoleaks have a reported incidence of about 5%13 but are generally self-limited, resolving quickly as fibrin seals the graft material. Type IV endoleaks are infrequently encountered with the newer generations of endografts that have materials with decreased porosity covering the stents.
The term endotension may also be used in conjunction with a post-EVAR evaluation and has been referred to by some as a type V endoleak.31 Endotension represents pressure in the aneurysm sac or sac enlargement without an identifiable endoleak. Some of these cases are likely associated with endoleaks that are not visualized with the imaging
studies performed. Other less likely causes of endotension include a seroma pressurizing the aneurysm sac, pressure transmission from the thrombus around the stent graft, or graft infection.31
studies performed. Other less likely causes of endotension include a seroma pressurizing the aneurysm sac, pressure transmission from the thrombus around the stent graft, or graft infection.31
Imaging Techniques
Although CT angiography is commonly used for post-EVAR surveillance and detection of endoleaks, this approach has a number of disadvantages, including the use of nephrotoxic contrast agents, patient exposure to ionizing radiation, and cost.17 Furthermore, certain technical factors can limit the accuracy of CT angiography, such as timing of the contrast bolus, the width of image slices, and interobserver variability.19 Pre- and postcontrast studies, typically with multidetector CT, are needed to distinguish between vessel wall calcification and endoleaks, although newer dual-energy CT systems can better differentiate calcium from contrast. It has been estimated that 33% to 65% of post-EVAR cost is secondary to the necessary radiologic studies, which may include lifelong surveillance with CT imaging.30,32
Digital subtraction angiography is usually performed to confirm suspected cases of endoleaks detected by other imaging methods. The feasibility of angiography as a surveillance tool post-EVAR is hindered by its invasiveness, exposure to radiation, and the use of nephrotoxic contrast agents. Furthermore, improper technique or the timing of an angiography contrast injection might result in an endoleak being overlooked.
Duplex Ultrasound
Duplex ultrasound is currently the preferred method for routine diagnosis and surveillance of unrepaired AAAs, as discussed in Chapter 15. In recent years, duplex ultrasonography has also evolved as an effective tool for post-EVAR surveillance. Duplex ultrasound can be used to measure the size of the residual aneurysm sac, detect endoleaks, and evaluate hemodynamic changes or stenosis in the outflow graft limbs and aortic branch vessels. Patency of the renal arteries, which can be compromised by graft fabric impingement, proximal fixation components, or proximal device migration, can be evaluated with duplex ultrasound. With enhanced resolution and better imaging technology, the ability to identify endoleaks with duplex scanning has also improved.23
The routine use of post-EVAR duplex ultrasound for surveillance has numerous advantages. Patients with renal insufficiency benefit from avoidance of repeated exposure to nephrotoxic contrast agents with CT imaging. During long-term follow-up, it has been shown that the risk for a decline in renal function is significantly greater after EVAR than after open aneurysm repair in patients with or without preexisting renal insufficiency.33,34 The ability to eliminate the use of ionizing radiation and its lower cost make abdominal duplex ultrasonography an attractive alternative. A financial analysis of aortic graft surveillance estimated the cost of a CT angiogram at $2779 per study, in comparison to the cost of an abdominal aortic duplex ultrasound at $525 per study.17 Even with the additional cost of routine abdominal radiographs needed to confirm the position of the stent graft, Bendick and colleagues17 estimated an average 3-year saving of more than $16,000 per patient followed up with duplex ultrasound rather than CT imaging after EVAR. Other potential benefits include wider availability and portability and the noninvasive nature of the procedure. However, duplex scanning may not be technically satisfactory in every case. Visualization of the aorta and the iliac vessels can be limited by the presence of overlying bowel gas, body habitus, ascites, and vessel tortuosity. Nevertheless, experience has shown that post-EVAR duplex ultrasound is an effective modality for surveillance and evaluation of aneurysm size and the presence of endoleaks.15,16,17,20,22,23,24,25,35,36
Duplex ultrasound is an accurate measurement tool for aortic aneurysm size. Aneurysm diameter has been shown to correlate within 5 mm between CT and duplex ultrasound in 70% to 92% of the cases.16,20,36 Raman and associates36 performed a retrospective review of 281 patients comparing color-flow duplex ultrasound and CT imaging for post-EVAR surveillance. Routine abdominal radiographs were used to assess the integrity of the stent graft and evaluate for fractures or migration. Minimal variability between the measurements for the minor axis of the aorta was noted between the two diagnostic modalities. Using the abdominal CT scan as the gold standard for post-EVAR evaluation, duplex ultrasonography was demonstrated to have a sensitivity of 42%, a specificity of 96%, a positive predictive value of 54%, and a negative predictive value of 94%. This has been corroborated by Arko and coworkers19 who examined post-EVAR follow-up CT and ultrasound studies in 201 patients. No significant difference was identified on paired analysis of maximal aortic diameter measurements with either imaging technique. Graft patency was documented to be 99% by both CT scan and duplex ultrasound. Furthermore, in comparison with CT imaging, duplex ultrasonography was shown to have a sensitivity of 81%, a specificity of 95%, a positive predictive value of 94%, and a negative predictive value of 90% for diagnosing an endoleak. The few endoleaks missed by duplex ultrasonography but diagnosed by a CT scan involved small lumbar arteries.
In addition to information regarding aneurysm sac size and endoleaks, iliac limb or outflow graft stenosis after EVAR can be easily diagnosed on duplex ultrasound.21 Access vessels such as the external iliac arteries are often atherosclerotic with heavy calcification and may need predilation before advancing large sheaths and placing stent grafts. Hemodynamically significant stenosis may require future treatment with balloon angioplasty or stenting. Access vessel complications during EVAR, including dissection, bleeding, false aneurysm, arterial thrombosis, and arterial embolization, were reported in 13% of the patients in the EUROSTAR registry.37 Subsequent iliac stent graft stenosis has been reported in 5.5% to 9% of cases.31 Therefore, the evaluation of iliac graft limbs and the native iliac arteries is an essential part of post-EVAR duplex ultrasound surveillance.
Migration of the stent graft, defined as greater than 10-mm displacement, has an incidence of 1.4% during the first year post-EVAR.31,38 Rarely, graft material may impinge upon the orifices of the renal arteries owing to either a short aneurysm neck or inaccurate deployment of the graft. A compromised renal artery can often be salvaged with stenting during the initial EVAR procedure or during a subsequent angiographic evaluation. It is important for duplex ultrasonography to evaluate the patency and any degree of stenosis in the renal arteries. Although not specifically validated in patients after EVAR, standard interpretation criteria for native renal arteries are usually applied. The duplex criteria for diagnosis of 60% or greater native renal artery stenosis include peak systolic velocity of 200 cm/s or greater and renal-to-aortic velocity ratio (RAR) of 3.5 or greater.39 There are no standard duplex criteria for stenosis in stented renal arteries, although experience suggests that velocity thresholds for significant stenosis in stented renal arteries are higher than those for native renal arteries (see Chapter 24).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree