13 Double-Outlet Right Ventricle
I. CASE
A. Fetal echocardiography findinges
1. The fetal echo reveals situs solitus of the atria, levocardia, left aortic arch, heart rate of 132 bpm, normal cardiac axis and position, and mild cardiomegaly (cardiothoracic ratio = 0.38).
2. The four-chamber view is abnormal, with a small posterior left ventricle.
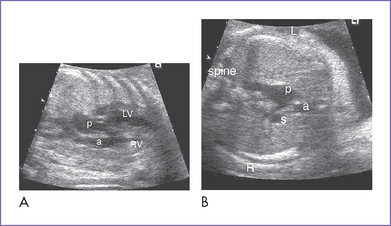
3. The outflow assessment reveals transposition of the great arteries (TGA) (aorta anterior and to the right of the pulmonary artery), mild asymmetry and the aorta slightly smaller than the pulmonary artery (Fig. 13-1).
4. The aortic valve is bicuspid, and the annulus is a normal size for gestation. The valve domes mildly in systole, with moderate flow acceleration through it by Doppler (1.5 m/s).
5. The main pulmonary artery is a good size and has confluent branch pulmonary arteries with normal Doppler velocity through them.
6. The aortic arch is leftward; however, the aortic arch is smaller than the ductal arch. Both arches have antegrade flow.
7. There is a large perimembranous ventricular septal defect (VSD) with outlet extension.
8. There is straddling of the mitral valve.
9. Flow through the foramen ovale is unrestricted, with a bidirectional shunt.
10. The pulmonary venous flow pattern and drainage are normal.
11. The Tei index (myocardial performance index) is normal in both ventricles.
D. Fetal management and counseling
1. Management: Diagnosis of any form of double-outlet right ventricle (DORV) should prompt referral for the following:
a. Thorough anatomic examination by ultrasound.
c. In this case, the abnormal maternal serum screen is an additional reason to ask for amniocentesis.
2. Follow-up includes serial antenatal studies at 4- to 6-week intervals.
a. Pulmonary and aortic outflow obstruction (bilateral outflow tract obstruction) is possible, with progressive hypoplasia of the aortic valve, ascending aorta, and arch and evolving coarctation of the aorta.
b. Check the size of the VSD (might become restrictive).
c. Monitor the direction of ductal flow.
d. Monitor ventricular size and function using the biventricular Tei index.
e. Watch for development of hydrops fetalis. It is unlikely unless there is biventricular dysfunction or significant atrioventricular (AV) valve or semilunar valve regurgitation.
F. Neonatal management
a. If there is progressive arch hypoplasia with or without aortic outflow obstruction, initiation of prostaglandin E1 (PGE1) infusion should be considered to keep the ductus open at least until a postnatal echocardiogram confirms or excludes important outflow tract and arch pathology.
b. In addition, given the potential for transposition physiology and streaming, PGE1 may be necessary until an atrial septostomy is performed to improve atrial and ventricular level mixing.
c. Administration of oxygen can increase oxygen saturation by decreasing pulmonary valve regurgitation and increasing blood flow.
d. At times, volume and inotropic support may be indicated to improve ventricular function and atrial level mixing.
2. Surgical: In this case, given the presence of a straddling mitral valve, single ventricle palliation is most likely in order.
b. Stage 2 is a bidirectional Glenn shunt at 4 to 6 months, following diagnostic cardiac catheterization.
c. Stage 3 is a modified Fontan procedure at 2 to 5 years of age.
II. YOUR HANDY REFERENCE
A. Prevalence
1. DORV accounts for less than 1% of all congenital heart disease.
2. Allan and Sharland (1992) studied a total group of 2136 fetuses with heart diseases diagnosed prenatally. These included 62 (3%) cases of DORV.
b. Survival: 17 babies survived (61% survival rate of continuing pregnancies).
3. In fetal life, DORV in the absence of ventricular hypoplasia is one of the less commonly identified lesions in utero. As in TGA, the four-chamber view may be normal, and most of these lesions go undetected at the time of obstetric ultrasound examination.
C. Associated syndromes and extracardiac anomalies
1. DORV can be associated with chromosomal abnormalities and is present in 12% of cases in one fetal series.
2. The tetralogy of Fallot (TOF) type of DORV may be associated with trisomies 13, 18, and 21 as well as with microdeletion of chromosome 22 (velocardiofacial or DiGeorge’s syndrome).
3. The TGA type of DORV has a lower risk of chromosomal abnormalities.
4. DORV associated with mitral atresia and normally related great arteries can be seen in trisomies 18 and 13.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree