Cerebral microemboli are frequently observed during coronary angiography (CA) and percutaneous coronary intervention (PCI), and their numbers have been related to the vascular access site used. Although cerebral microemboli can cause silent cerebral lesions, their clinical impact is debated. To study this, 93 patients referred for CA or PCI underwent serial cognitive testing using the Montreal Cognitive Assessment (MoCA) test to detect postprocedural cognitive impairment. Patients were randomized to radial or femoral access. In a subgroup of 35 patients, the number of cerebral microemboli was monitored with transcranial Doppler technique. We found the median precatheterization result of the MoCA test to be 27, and it did not change significantly 4 and 31 days, respectively, after the procedure. There was no significant correlation between the number of cerebral microemboli and the difference between preprocedural and postprocedural MoCA tests. The test results did not differ between vascular access sites. One-third of the patients had a precatheterization median MoCA test result <26 corresponding to mild cognitive impairment. In conclusion, using the MoCA test, we could not detect any cognitive impairment after CA or PCI, and no significant correlations were found between the results of the MoCA test and cerebral microemboli or vascular access site, respectively. In patients with suspected coronary heart disease, mild cognitive impairment was common.
The aim of the study was first to test the hypothesis that a decrease in cognitive function occurs after coronary angiography (CA) or percutaneous coronary intervention (PCI) as assessed by the Montreal Cognitive Assessment (MoCA) test ; second, to evaluate a possible relation between cerebral microemboli and cognitive impairment; and third, to investigate the potential influence of vascular access site for cognitive impairment, serving as a pilot study for future end point studies.
Methods
Patients with stable angina pectoris without a history of coronary artery bypass graft (CABG) surgery, or advanced kidney disease with an estimated glomerular filtration rate (eGFR) <30 ml/min, referred for CA at the Karolinska University Hospital were eligible. The study was approved by the regional ethics committee and complied with the Declaration of Helsinki. All patients provided written informed consent.
The MoCA test assesses visuospatial abilities, memory, executive functioning, attention, concentration and working memory, language, and orientation. Details regarding normative data and MoCA test administration are available at www.mocatest.org . Permission to use the MoCA test was obtained, and the test was used in 2 Swedish versions. The first MoCA test was performed 1 to 5 days before CA for baseline assessment. Diazepam was given as sedative medication during the procedure. The half-life of diazepam varies substantially and is prolonged at higher age and by β-blocker therapy. Hence, the first follow-up MoCA test was scheduled day 3 after CA or PCI to allow for washout of the drug, and the second version of the MoCA test was applied. For the second follow-up MoCA test, completed 30 days after the procedure, the baseline version of the test was used. Patients were randomized to radial or femoral access sites to investigate their potential influence on cognitive function. CA was performed according to standard procedure with PCI ad hoc when indicated. A subgroup of patients were also examined with transcranial Doppler (TCD) during the catheterization procedure. Both middle cerebral arteries were continuously monitored with a multifrequency Doppler system (Embodop; Compumedics DWL, Singen, Germany). The system automatically identifies cerebral microemboli and differentiates them as gaseous or particulate. Data registration was divided into CA and PCI.
The results of the MoCA test and the number of cerebral microemboli are presented as median and interquartile range (Q1 to Q3). Follow-up MoCA tests were compared with baseline MoCA test using the Wilcoxon signed-rank test. The Spearman rank test was used to test for a correlation between the number of microemboli and the difference between the first follow-up MoCA test and baseline. The difference between baseline and the first follow-up MoCA test result was compared according to access site group with the Mann–Whitney U test. All tests were 2 sided; the level of statistical significance was p <0.05, and all statistical analyses were performed using SPSS Version 22 (IBM Corp., Armonk, New York).
For the prospective calculation of sample size, a difference of 2 points in MoCA test results from baseline was considered clinically relevant. With an assumed SD of 2.5 adjusted for non–normally distributed data using Pitman efficiency, at least 29 patients were needed in each group to detect a statistical significant difference with 80% power and p <0.05. According to a high estimated dropout frequency, we aimed to include at least 49 patients in each group.
Results
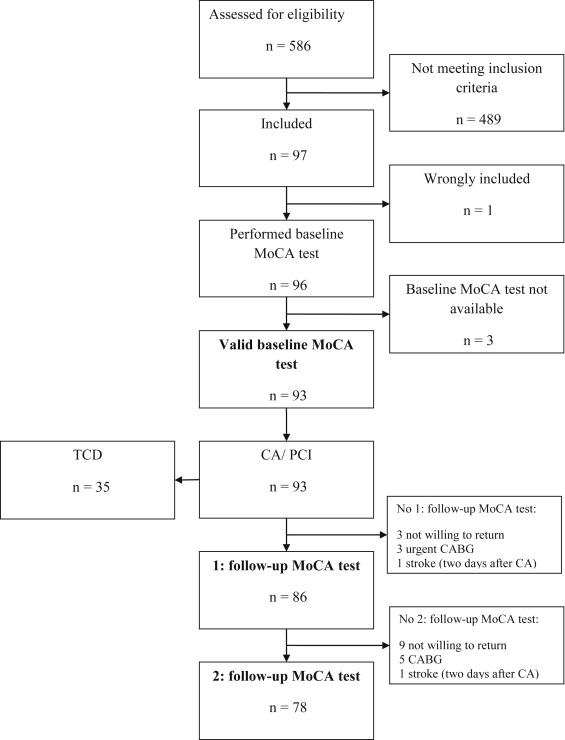
The study was conducted from September 2011 to March 2012 at the Karolinska University Hospital. Of the 586 patients screened for eligibility, 97 patients were included, and the results of 93 patients were finally analyzed ( Figure 1 ). All patients underwent CA, PCI, or CA combined with PCI with evenly distributed vascular access sites. A subgroup of 35 patients was monitored with TCD during the procedure. The first follow-up MoCA test was completed by 86 patients in median 4 days (min to max 2 to 14 days) after the procedure. The second follow-up MoCA test was performed by 78 patients in median 31 days (min to max 20 to 59) after the procedure. Overall, 77 patients completed all 3 MoCA tests.