1 Distinguishing Systolic versus Diastolic Heart FailureA Practical Approach by Echocardiography
Left Ventricular Dimensions and Thickness
See Appendix for reference values.
Key Points
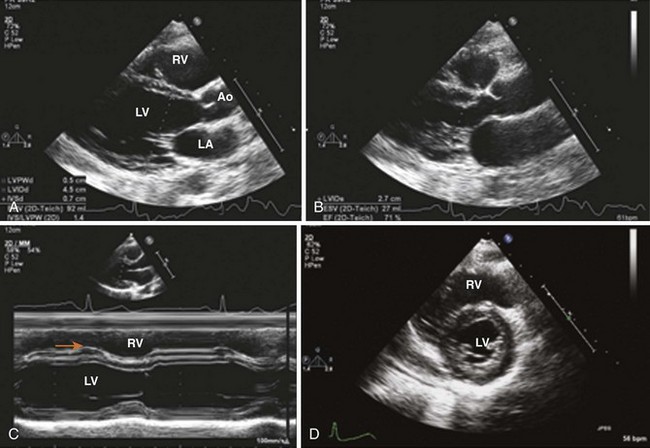
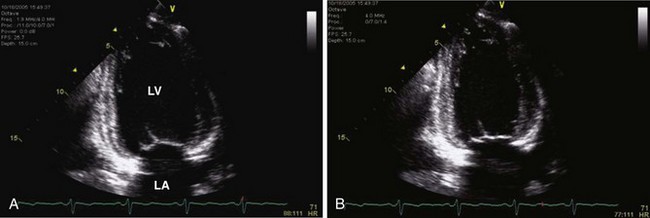
• These values are measured in the parasternal long-axis (PLAX) (Figure 1-1) or parasternal short-axis (PSAX) view using 2D or M-mode.
• Two-dimensional (2D) echocardiographic measurements should be made from trailing edge to leading edge.
• M-mode echocardiographic measurements are always slightly greater than 2D measurements because of these conventions.
• Measurement is made at the level of the LV minor axis, approximately at the mitral valve leaflet tips.
• LV mass is measured by M-mode at PLAX view or by 2D method at the midpapillary muscle level in the short-axis (SAX) view.
• These linear measurements can be made directly from 2D images or using 2D-targeted M-mode echocardiography (Figure 1-2; see also Figure 1-1).
Limitations
• LV posterior chords, anterior aberrant chords, and the tricuspid apparatus may be misinterpreted as the LV posterior wall and inner and outer borders of the anterior interventricular septum (IVS), respectively (see Figure 1-1C, orange arrow).
• End-diastole can be defined at the onset of the QRS complex, but is preferably defined as the frame after mitral valve closure or the frame in the cardiac cycle in which the cardiac dimension is largest.
Left Ventricular Systolic Function
Fractional Area Change
Key Points
• Fractional area change is obtained from the PLAX view by the M-mode or 2D method as (LVEDD − LVESD)/LVEDD × 100, where LVEDD is end-diastolic dimension and LVESD is end-systolic dimension (see Figure 1-1).
• It is easy to perform; however, it has technical limitations in the presence of segmental wall motion abnormalities and an abnormally shaped ventricle. 2D- and M-mode–derived ejection fraction by the Teichholz method are based on minor dimensions: (end-diastolic volume − end-systolic volume)/end-systolic volume where the end-diastolic volume = 7/(2.4 + EDD) × EDD3 and the end-systolic volume = 7/(2.4 + ESD) × ESD3. Because of geometric assumptions, these methods have been superseded by 2D volumetric methods.
Left Ventricular Volumes and Ejection Fraction (Table 1-1)
TABLE 1-1 ECHOCARDIOGRAPHIC ASSESSMENT OF LEFT VENTRICULAR SYSTOLIC FUNCTION
| Method | View | Pitfalls |
|---|---|---|
| Two-Dimensional Imaging | ||
| Fractional shortening | PLAX or PSAX | Geometric Assumptions Based on a single cross section Ignores wall motion in nonmeasured segments |
| Ejection fraction | (LVEDV − LVESV) × 100/LVEDV | Dependent on load and heart rate (HR) |
| Modified Simpson’s rule | 4-chamber and 2-chamber | Foreshortening of apical views Poor visualization of anterior wall |
| Area-length method | 4-chamber (LV area)2 × 0.85/LV end-diastolic length | Not appropriate for non-symmetrical LV Assumes cylindrical LV shape |
| Bullet method | Mid-SAX and apical 4- chamber | LV shape assumption |
| Wall motion score index | PLAX, PSAX, apical 4-, 2-, and 3-chamber Average endocardial thickening score of 16 or 17 segments | Reader and center variability Requires visualization of all segments |
| Exercise ejection fraction | As above | To detect incipient LV systolic dysfunction Usually eyeballed |
| Three-dimensional volumes | Full-volume apical view | Resolution is dependent on 2D image quality |
| Doppler Methods | ||
| LV stroke volume | PLAX 2D and apical 5- or 3-chamber | Circular shape assumption of LV outflow tract (LVOT) Error in LVOT measurement Errors are squared |
| LV dP/dt (mm Hg/s) | MR CW Doppler Σ Δt 1 m/s to 3 m/s, 32/Δt | Load independent Not always feasible |
| MPI | Apical 5-chamber | Somewhat load dependent No geometric assumption |
| Tissue Doppler | Apical views Objective data Less dependent on image quality Less dependent on reader expertise | Somewhat load dependent Requires parallel angle of insonation Affected by translation, tethering, and respiration |
| 2D speckle tracking | Longitudinal Strain Not affected by Doppler angle | Requires high frame rate Requires good 2D image resolution Decreased feasibility versus TDI |
| Radial Strain Not affected by Doppler angle | ||
Key Points
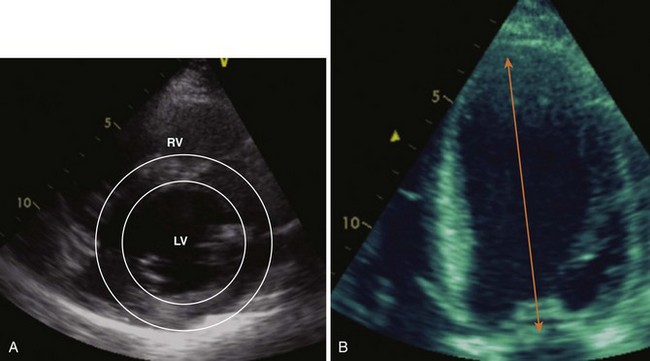
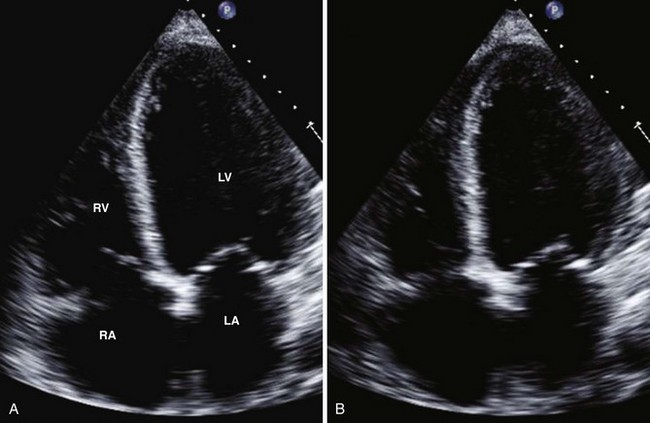
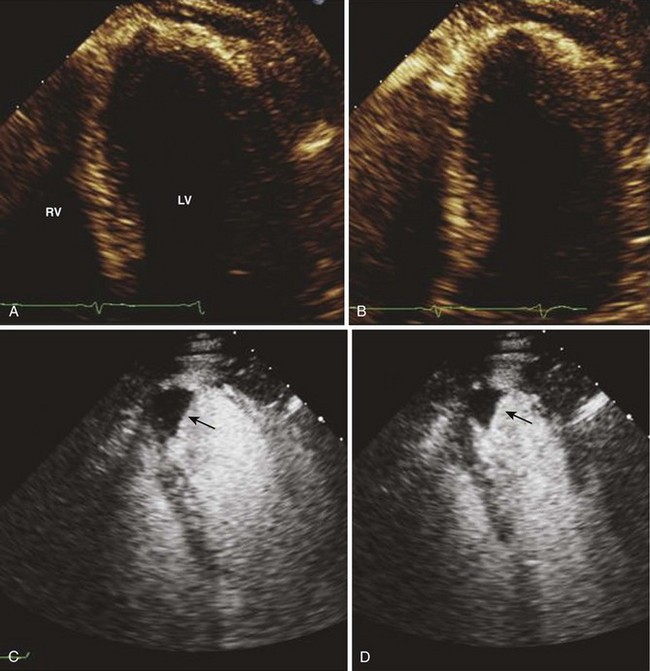
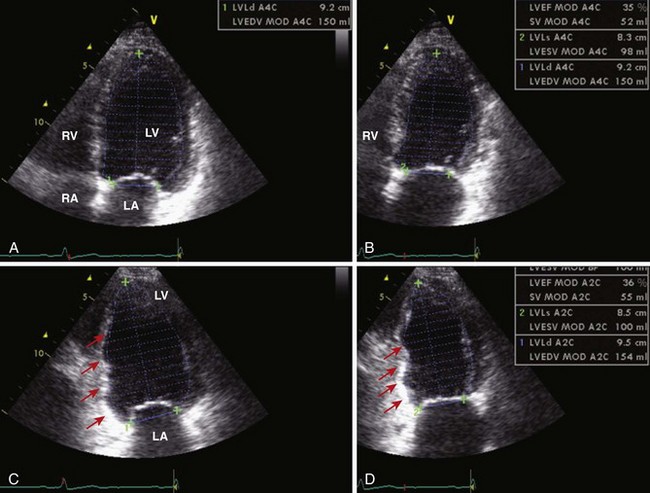
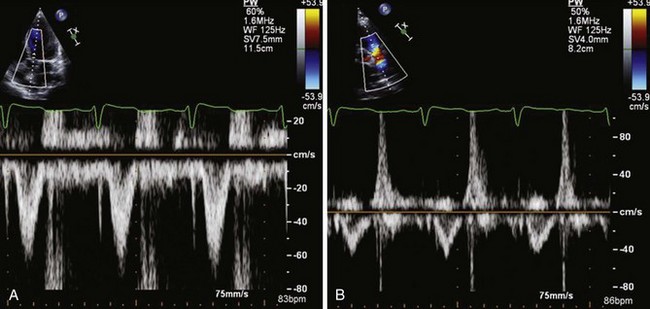
• The most commonly used 2D measurement for volume estimations is the biplane method of disks (modified Simpson’s rule; Figures 1-4 and 1-5). Left-sided contrast agents used for endocardial border delineation are helpful and improve measurement reproducibility for suboptimal studies and correlation with other imaging techniques (Figure 1-6). These agents also help improve diagnosis of left ventricular thrombus (Figure 1-7).
Segmental Wall Motion
Key Points
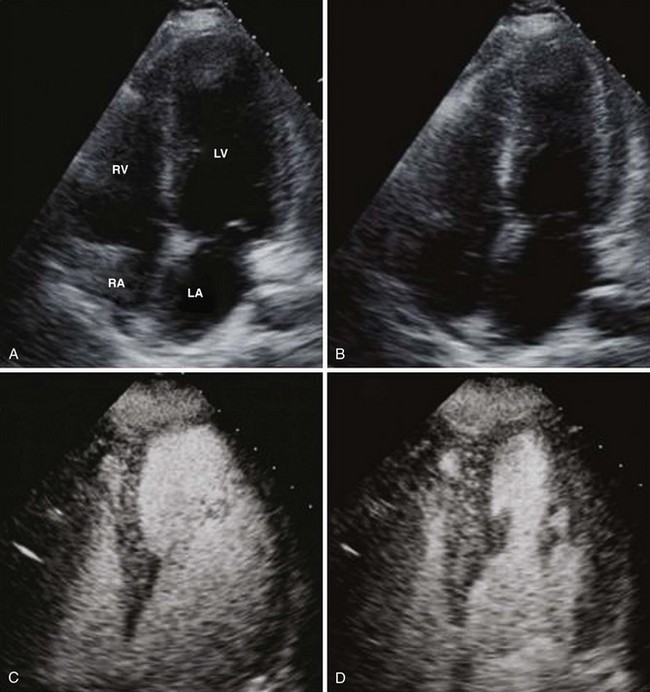
• Dilated ischemic cardiomyopathy (ICM): hypokinetic segments as well as akinetic segments with or without thinning and increased echogenicity suggesting scar formation (Figure 1-8; see also Figures 1-6 and 1-7).
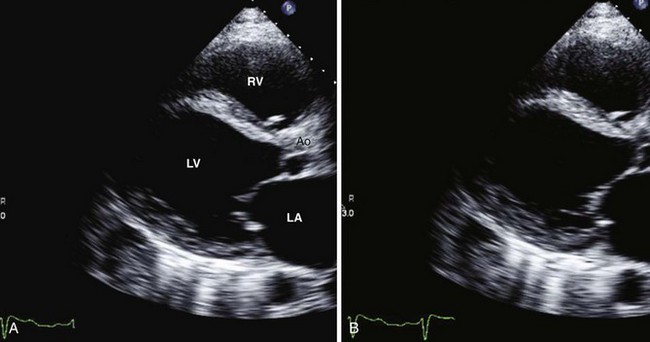
• Dilated non-ischemic cardiomyopathy (NICM): usually global hypokinesis; some segments may be akinetic, dyskinetic, or aneurysmal (see Figures 1-2, 1-4, and 1-5).
• LV thrombus may be present in the apical/distal IVS region or rarely at inferior/lateral aneurysmal segments (see Figure 1-7).
• Reversed IVS motion with or without apical and inferoapical dyskinesis occurs in the presence of left bundle branch block or RV pacing.
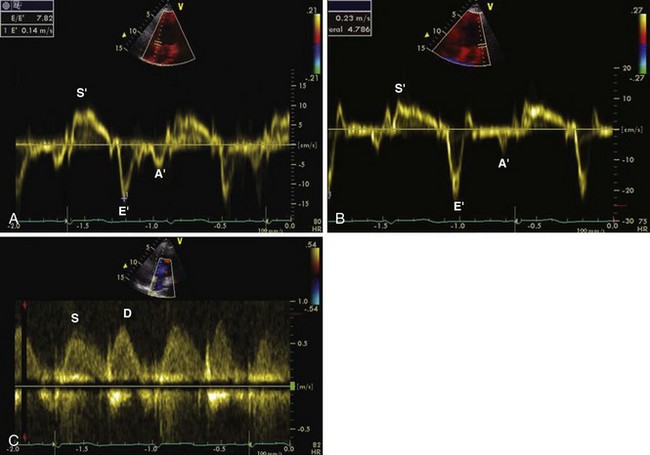
LV Function Assessment by Tissue Doppler Imaging (Figure 1-9)
Key Points
• Tissue Doppler imaging (TDI) provides more objective data and is less dependent on reader expertise.
• TDI systolic and diastolic velocities can be obtained reliably in basal and mid-myocardial segments by color-coded and pulsed wave (PW) Doppler techniques. Velocity of motion, displacement, and deformation can be measured in the longitudinal, radial, and circumferential planes.
LV Function Assessment by 2D Speckle Tracking (Figure 1-10)
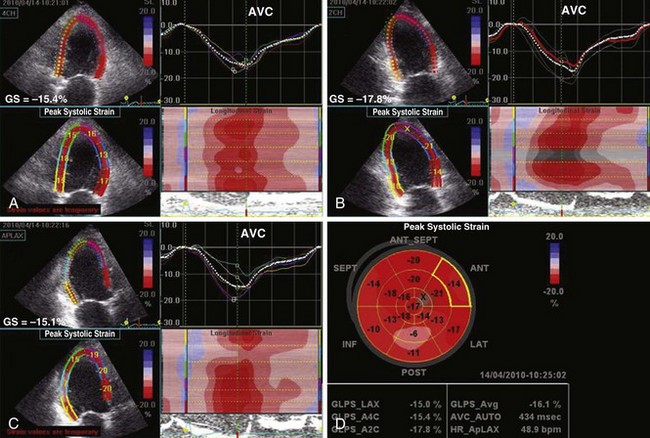
Figure 1-10 Apical 4-chamber (A), 2-chamber (B), and 3-chamber (C) 2D strain maps and segmental strain scores along with bull’s-eye map (D) showing global strain (GS) and segmental strain values in the same patient as in Figure 1-8. Note reduced segmental strain values of −6 to −13% in the basal to midinferior and inferolateral segments consistent with transmural infarction. GS is mildly reduced at −16%. AVC, aortic valve closure.
Key Points
• Twist is normal in diastolic heart failure (DHF) and markedly reduced in systolic heart failure (SHF) (SHF: 5 ± 2.8, DHF: 13 ± 6.8, control: 14 ± 5.8).
• Circumferential strain is normal in DHF (15% ± 5%) and markedly reduced in SHF (7% ± 3%) (control groups: 20% ± 3%).
• In patients with preserved ejection fraction (50%), regional longitudinal strain of ≤13% compared to other segments identified transmural myocardial infarction (MI) with 80% sensitivity and specificity (see Figure 1-10).
Methods Evaluating Combined Systolic and Diastolic Function
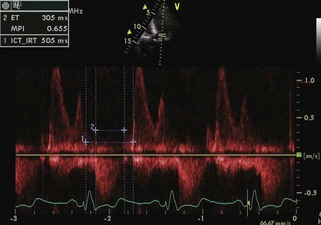
Myocardial Performance Index
Key Points
• The myocardial performance index is defined as the sum of isovolumic contraction time (IVCT) and isovolumic relaxation time (IVRT) divided by ejection time (ET).
• The myocardial performance index has prognostic value in various clinical settings because it seems to be independent of heart rate (Figure 1-12).