Distal Upper Extremity Revascularization (Brachial to Radial/Ulnar/Hand Bypass)
Philip S. K. Paty
Benjamin B. Chang
Introduction
Arterial reconstruction of occlusive disease in the upper extremity has been reported sparingly in the literature with most reports dealing with anecdotal cases or small series. This is in contradistinction to bypass of lower extremity occlusive disease and most likely reflects the lower incidence of atherosclerosis obliterans and increased incidence of differing associated disease processes involving the upper extremity such as collagen vascular disorders, rheumatoid arthritides, posttraumatic aneurysm, etc. In addition, the major cause of tissue loss in the hand is usually disease below the carpal bones of the hand involving palmar and digital arteries as opposed to larger more proximal arteries which occurs in at most 10% of patients.
Arterial reconstructions of infracarpal or arteries beyond the carpal bones are infrequently pursued in most vascular surgery practices. The techniques and exposures involved are often considered to lie outside of the standard armamentarium. As a result, most vascular surgeons when confronted by upper extremity ischemic pain and tissue loss will resort to wound care, chronic calcium channel blocking agents, dorsal sympathectomy, and referral to plastic or other hand specialty services. Reports of arterial reconstructions to these infracarpal arteries are rare and have seldom involved series of more than 15 patients. In the present chapter, we will outline the technical approach to arterial reconstruction to infracarpal arterial outflow arteries.
Clinical evaluation of the patient presenting with upper extremity arterial occlusive disease is most important in determining the subsequent medical and surgical management. A complete history and physical is paramount in order to identify pertinent personal and family medical issues, a history of repetitive trauma, etc. These patients are more frequently afflicted with medical problems and symptom complexes such as
renal failure, rheumatoid arthritides, collagen vascular diseases, and advanced atherosclerosis. Those patients with antecedent histories of rheumatoid and collagen vascular etiologies are more likely to present at an earlier age. All patients without a defined etiology should be referred and evaluated by a rheumatologist with appropriate serologic markers drawn (complete blood count, erythrocyte sedimentation rate, serum protein immunoelectrophoresis, cryogobulin, anticardiolipin titer, lupus procoagulant, beta-2 glycoprotein antibody, rheumatoid factor, ANA DNA, ENA (anti RNP and SM), CCP IGG, ESR, parvovirus, Hepatitis B serology, parvovirus and ACE level).
renal failure, rheumatoid arthritides, collagen vascular diseases, and advanced atherosclerosis. Those patients with antecedent histories of rheumatoid and collagen vascular etiologies are more likely to present at an earlier age. All patients without a defined etiology should be referred and evaluated by a rheumatologist with appropriate serologic markers drawn (complete blood count, erythrocyte sedimentation rate, serum protein immunoelectrophoresis, cryogobulin, anticardiolipin titer, lupus procoagulant, beta-2 glycoprotein antibody, rheumatoid factor, ANA DNA, ENA (anti RNP and SM), CCP IGG, ESR, parvovirus, Hepatitis B serology, parvovirus and ACE level).
In addition, there is often an increased incidence of hypercoaguable states in these patients and hematologic consultation should be obtained routinely with laboratory testing for antithrombin III, Factor V Leiden, protein C and S, plasma homocysteine levels. Patients with active disease or hypercoaguable states may require preoperative steroids or anticoagulation. Lastly, elderly patients and those in whom atherosclerosis is the primary etiology should have preoperative cardiology risk assessment.
Local wound care of all patients with tissue loss especially digital necrosis should be instituted. This may require intravenous antibiotics and preoperative debridement of necrotic lesions. In some patients with nonatherosclerotic etiologies, especially those with active arteritis, the results of revascularization are often so dismal as to warrant a prolonged trial of medical management. In these selected patients, continued close surveillance with minor digital debridement and amputation may achieve eventual wound healing.
Noninvasive vascular evaluation should be performed in all patients with pulse volume recordings and segmental plethysmography to the level of the digits. If abnormalities in perfusion are found, patients should undergo catheter-directed contrast arteriography to the level of the digital arteries. This examination should be supplemented with intra-arterial priscoline or nitroglycerin to unmask arterial vasospasm. Particular attention should be paid to the presence of severe stenosis or the presence of lesions with embolic potential in proximal brachiocephalic arteries. These lesions may be treated percutaneously at the time of the diagnostic procedure either with covered or noncovered endovascular stents at the discretion of the vascular surgeon. Alternatively, these lesions may be treated with endarterectomy or bypass as described in prior chapters.
Patients are considered reconstructible if a patent superficial or deep palmar arch or common digital artery in line with the ischemic digit in question is present on angiogram. The presence of an incomplete superficial or deep palmar arch does not preclude the option for bypass. Patients with a demonstrable outflow vessel should undergo vein mapping of all extremities with Doppler ultrasound to identify a suitable conduit for bypass.
Patients are brought to the operating suite and in the majority of cases will be intubated and the procedures performed under general anesthesia. Alternatively in the high-risk patient in whom the entire procedure is limited to one extremity, an axillary or supraclavicular plexus block may be utilized. The involved upper extremity as well as those required for the harvest of autogenous venous conduit are prepped and draped accordingly.
Preoperative angiography will dictate the arterial inflow source. As with lower extremity, any inflow may be used in the absence of a hemodynamically significant proximal stenosis. The one caveat to this rule is in patients with diabetes mellitus where radial inflow sources may be prone to significant vasospasm.
Brachial Artery Exposure
The majority of these bypasses are performed with mid to distal brachial artery inflow. The mid or supracondylar brachial artery is exposed through a medial longitudinal
incision overlying the bicipital groove (Fig. 7.1). Sharp dissection with a #15 scalpel blade is preferred. Once the incision is deepened below the dermis, care should be taken to avoid injury to median antebrachial cutaneous, median, and ulnar nerves and the basilic vein. Exposure of the distal brachial artery is performed through part or all of a sigmoid-shaped incision overlying the antecubital fossa. Once this incision is deepened, care is taken to avoid damage to the antecubital basilic and cephalic veins as well as the aforementioned nerves. Once the bicipital aponeurosis and minor crossing veins divided, the brachial artery is readily exposed.
incision overlying the bicipital groove (Fig. 7.1). Sharp dissection with a #15 scalpel blade is preferred. Once the incision is deepened below the dermis, care should be taken to avoid injury to median antebrachial cutaneous, median, and ulnar nerves and the basilic vein. Exposure of the distal brachial artery is performed through part or all of a sigmoid-shaped incision overlying the antecubital fossa. Once this incision is deepened, care is taken to avoid damage to the antecubital basilic and cephalic veins as well as the aforementioned nerves. Once the bicipital aponeurosis and minor crossing veins divided, the brachial artery is readily exposed.
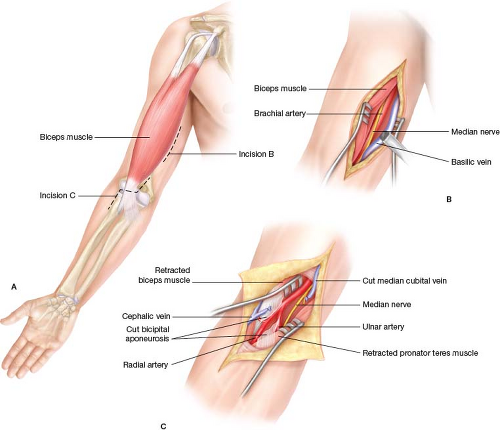 Figure 7.1 A: Exposure of the brachial artery at the mid-upper arm and elbow. B:
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|