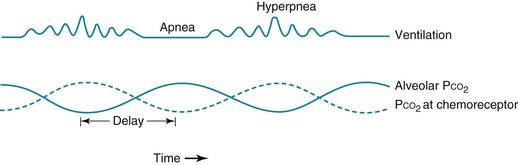
18 The finely tuned system of ventilatory control described in Chapter 17 is altered in a variety of clinical circumstances. In some cases, a primary disorder of the nervous system affects the neurologic network involved in ventilatory control and therefore may either diminish or increase the “drive” to breathe. In other instances the controlling system undergoes a process of adaptation in response to primary lung disease, so any alteration in function is a secondary phenomenon. Patients with these syndromes of hypoventilation are characterized by depressed ventilatory responses to the chemical stimuli of hypercapnia and hypoxia. Measurement of arterial blood gases generally reveals an elevation in arterial PCO2 accompanied by a decrease in PO2, the latter primarily attributable to hypoventilation. As in other disorders associated with these blood gas abnormalities, cor pulmonale may result and be the presenting problem in these syndromes. The term congenital central hypoventilation syndrome or Ondine’s curse (see Chapter 17) has been applied to a rare subset of patients with congenital alveolar hypoventilation. However, an element of decreased ventilatory response to hypercapnia and hypoxia is much more commonly seen in clinical practice and probably represents a spectrum of abnormalities in ventilatory response. In the past, treatment of alveolar hypoventilation generally centered around two modalities: drugs (most commonly the hormone progesterone) and electrical stimulation of the phrenic nerve. Progesterone is well known to be a respiratory stimulant and in some cases may improve respiratory drive and decrease CO2 retention. In the second approach, the diaphragm can be induced to contract by repetitive electrical stimulation of the phrenic nerve, which can be achieved by intermittent current applied via an implanted electrode. Although both of these modalities are still used, the most common current therapy for patients with clinically significant hypoventilation is noninvasive positive-pressure (i.e., assisted) ventilation, usually applied nocturnally. This topic is discussed in Chapter 29. Cheyne-Stokes breathing is a cyclic pattern in which periods of gradually increasing ventilation alternate with periods of gradually decreasing ventilation (even to the point of apnea). This type of ventilation is shown schematically in Figure 18-1. It has been known for many years that two main types of disorders are associated with this type of breathing: heart failure and some forms of CNS disease. Cheyne-Stokes breathing can also be seen under certain physiologic situations even in the absence of underlying disease. Examples include the onset of sleep and exposure to high altitude. Prolongation in circulation time, which is one mechanism postulated to play a role in heart failure, results in an abnormal delay between events in the lung and sensing of PCO2 changes by the central chemoreceptors. Hence, medullary respiratory output is out of phase with gas exchange at the lungs, and oscillations in ventilation occur as the central chemoreceptor and the medullary respiratory center make belated attempts to maintain a stable PCO2 (see Fig. 18-1). A similar type of instability of ventilatory control occurs when hypoxia is driving the feedback system, as is seen on exposure to high altitude. The ventilatory response to hypoxia is nonlinear. For the same drop in PO2, the increment in ventilation is larger at a lower absolute PO2 (see Fig. 17-3). This means that at a relatively high initial PO2, the system is less likely to respond to small changes in PO2 but then is apt to overshoot as PO2 falls further. This instability of the respiratory control system results in a widely oscillating output from the respiratory center and thus a cyclic pattern of ventilation.
Disorders of Ventilatory Control
Primary Neurologic Disease
Presentation with Hypoventilation
Cheyne-Stokes Breathing
Thoracic Key
Fastest Thoracic Insight Engine