Recently, stress myocardial computed tomographic perfusion (CTP) was shown to detect myocardial ischemia. Our main objective was to evaluate the feasibility of dipyridamole stress CTP and compare it to single-photon emission computed tomography (SPECT) to detect significant coronary stenosis using invasive conventional coronary angiography (CCA; stenosis >70%) as the reference method. Thirty-six patients (62 ± 8 years old, 20 men) with previous positive results with SPECT (<2 months) as the primary inclusion criterion and suspected coronary artery disease underwent a customized multidetector-row CT protocol with myocardial perfusion evaluation at rest and during stress and coronary CT angiography (CTA). Multidetector-row computed tomography was performed in a 64-slice scanner with dipyridamole stress perfusion acquisition before a second perfusion/CT angiographic acquisition at rest. Independent blinded observers performed analysis of images from CTP, CTA, and CCA. All 36 patients completed the CT protocol with no adverse events (mean radiation dose 14.7 ± 3.0 mSv) and with interpretable scans. CTP results were positive in 27 of 36 patients (75%). From the 9 (25%) disagreements, 6 patients had normal coronary arteries and 2 had no significant stenosis (8 false-positive results with SPECT, 22%). The remaining patient had an occluded artery with collateral flow confirmed by conventional coronary angiogram. Good agreement was demonstrated between CTP and SPECT on a per-patient analysis (kappa 0.53). In 26 patients using CCA as reference, sensitivity, specificity, and positive and negative predictive values were 88.0%, 79.3%, 66.7%, and 93.3% for CTP and 68.8, 76.1%, 66.7%, and 77.8%, for SPECT, respectively (p = NS). In conclusion, dipyridamole CT myocardial perfusion at rest and during stress is feasible and results are similar to single-photon emission CT scintigraphy. The anatomical-perfusion information provided by this combined CT protocol may allow identification of false-positive results by SPECT.
In the previous few years, multidetector computed tomography has emerged as a powerful tool to evaluate patients with suspect coronary artery disease. Sixty-four–slice multidetector computed tomography has demonstrated high accuracy to detect significant coronary stenosis. A diagnostic tool that can provide detailed information on myocardial perfusion and coronary angiography at the same time will not only help in the prognostic assessment of the patient but also be valuable in choosing appropriate therapeutic strategies. The purpose of this study was to evaluate the feasibility of dipyridamole stress computed tomographic perfusion (CTP) and compare the diagnostic accuracy of dipyridamole stress myocardial CTP and single-photon emission CT perfusion defects to detect significant coronary stenosis (>70%) using CT angiography (CTA) and conventional coronary angiography (CCA) as the reference standards.
Methods
This is a prospective cohort study of consecutive patients with a positive single-photon emission CT/Myocardial perfusion image (MPI) examination who met eligibility criteria and agreed to sign informed consent to participate in this CT research stress perfusion study.
Patient selection for the study included 523 consecutive patients in our institution who underwent scintigraphic stress testing in the previous 2 months for suspected coronary artery disease and had a positive stress test result with a high probability clinically indicating invasive angiography ( Figure 1 ). The decision to undergo cardiac catheterization was made on clinical basis and single-photon emission CT results. Results of coronary CTA and CTP were blinded to the attending physician.

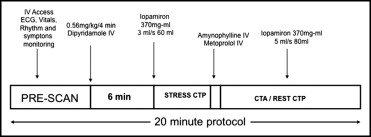
Thirty-six patients with suspected coronary artery disease and positive single-photon emission CT results <2 months previously underwent a customized (20-minute) multidetector CT protocol with myocardial perfusion evaluation at rest and during stress and coronary CTA. Multidetector computed tomography was performed in a 64-slice scanner (Aquillion 64, Toshiba, Ottawara/Japan). Exclusion criteria included asthma, pregnancy, renal insufficiency (serum creatinine >1.5 mg/dl), and known allergy to iodinated contrast or dipyridamole. All patients signed informed consent and our institutional ethic review board approved the study. All patients were instructed to have a diet free of caffeine 24 hours before examination. Multidetector CT customized protocol included 2 contrast-enhanced scans. Calcium score was not performed ( Figure 2 ). The first scan was a stress CT perfusion only, with low resolution. The second scan was done for coronary arteries ( Table 1 ). In addition, perfusion information was sought. Stress CTP image was obtained 2 minutes after intravenous infusion of dipyridamole 0.56 mg/kg every 4 minutes. During dipyridamole infusion, heart rate, blood pressure, electrocardiogram, and patients’ symptoms were monitored continuously. Helical acquisition for CTP was initiated, using a real-time bolus tracking technique, at the time of peak left atrial filling with contrast, which was determined visually (no specific threshold in Hounsfield units was used). Immediately after the stress scan, infusion with aminophylline (USP – São Paulo/Brazil) 240 mg was started to revert vasodilatation induced by dipyridamole. Before a second perfusion/CT angiographic scan at rest, intravenous metoprolol was administered until a maximum dose of 20 mg to lower heart rate and improve image quality. Scanning at rest was performed using automatic trigger detection on the descending aorta set to 180-HU signal density.
| Stress Perfusion | Coronary CTA | |
|---|---|---|
| Data | stress perfusion | rest perfusion coronary anatomy |
| Gating | retrospective | retrospective |
| Contrast | 60 ml (3 ml/s) | 80 ml (5 ml/s) |
| Drugs | dipyridamole | metoprolol |
| mA | 100 (32- × 1.0-mm column) | 240–270 in women, 370–340 in men |
| kV | 120 | 120 |
Two independent blinded observers with no knowledge of clinical data or other examinations performed visual and semiquantitative analyses for each method to include CTP, CTA and CCA and any discordance was resolved by consensus.
Data analysis was performed to correlate myocardium CTP and single-photon emission computed tomography (SPECT) and to compare diagnostic accuracy of myocardium CTP and SPECT to the reference standards (CTA and CCA; coronary stenosis >70% as reference).
The standard American College of Cardiology/American Heart Association 17-segment model was used to identify perfusion defects. For comparison of perfusion data (CTP vs SPECT) with coronary anatomical data derived from CTA/CCA, we consolidated the segmental data into 3 territories according to the American College of Cardiology/American Heart Association recommendation (per-vessel analysis). CTP datasets were evaluated on a true short axis, with 2- and 4-chamber views, with 8-mm–thick multiplanar reformatted images.
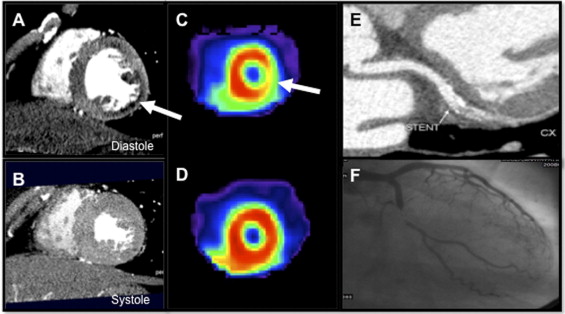
Thicker slices were used to improve low-contrast resolution for visual myocardium perfusion analysis, as described previously. Narrow window and level were also used (350 W and 150 L). Initial evaluation of perfusion defects started in the diastolic phase, and for potential artifacts readers could use the systolic phase to confirm the perfusion defect. True perfusion defects were defined as subendocardial hypoenhancement, encompassing ≥25% of transmural extent, present in different phases of the cardiac cycle and within a specific coronary territory.
CT angiographic raw data analysis was evaluated by 2 level-3 1-year fellowship-trained experts on coronary CTA, and stenoses were graded as 0% to 50% (mild), 51% to 70% (moderate), and >70% (severe). Coronary segments with severe calcification and smaller stents with no lumen visualization were graded as uninterpretable. Quantitative coronary assessment was performed in all patients who underwent CCA. Blinded readers considered coronary stenosis ≥70% as a hemodynamically significant lesion.
Statistical analysis was done using STATA 8.0 (STATA Corp., College Station, Texas). Continuous variables were expressed as mean ±SD and categorical variables as absolute number and percentage. Comparison between discrete variables used chi-square or Fisher’s exact test, as appropriate. Tables of frequency were used for sensitivity, specificity, and predictive values. Diagnostic values for perfusion methods were compared using test of proportions and McNemar test. Kappa analysis was performed to evaluate agreement.
Results
Thirty-six patients (62 ± 8 years old, 20 men) were enrolled in this protocol and underwent SPECT and multidetector computed tomography (stress perfusion and CTA). Clinical data are listed in Table 2 . The most common clinical symptoms were chest pain in 75% and dyspnea in 22%. All 36 patients completed the protocol with no adverse event, with a mean total radiation dose of 14.7 ± 3.0 mSv (minimum 11.4 mSv, maximum 20.3 mSv) and with interpretable scans. Mean, minimum, and maximum radiation doses for CTP scans were 3.4 ± 0.3, 3.0, and 4.1 mSv, respectively, and those for CT angiographic scans were 11.6 ± 2.3, 8.4, and 16.2 mSv.
| Age (years) | 62 ± 8 |
| Men | 20 (55%) |
| Smoker | 7 (19%) |
| Hypercholesterolemia (low-density lipoprotein >130 mg/dl) | 21 (58%) |
| Hypertension (blood pressure >120/80 mm Hg) | 27 (75%) |
| Diabetes mellitus | 8 (22%) |
| Body mass index >30 kg/m 2 | 5 (14%) |
| Body mass index >25 kg/m 2 | 20 (55%) |
Mean basal heart rate was 64 ± 9 beats/min. After dipyridamole stress, heart rate increased to 82 ± 12 beats/min; scan acquisition at rest (after aminophylline and metoprolol administration) showed that heart rate returned to 64 ± 7 beats/min.
In the 36 patients, comparing SPECT to CTP ( Figures 3, 4, and 5 ) by per-patient analysis showed good agreement of 75% with a kappa value of 0.53 (p <0.01; Figure 6 ).