Diffusing Capacity of the Lungs
An important step in the transfer of oxygen from ambient air to the arterial blood is the process of diffusion, that is, the transfer of oxygen from the alveolar gas to the hemoglobin within the red cell. The pertinent anatomy is shown in Figure 4-1A. The path taken by oxygen molecules is shown in Figure 4-1B. They must traverse the alveolar wall, capillary wall, plasma, and red cell membrane and then combine with hemoglobin.
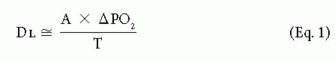
The diffusing capacity of the lungs (DL) estimates the transfer of oxygen from alveolar gas to red cells. The amount of oxygen transferred is largely determined by three factors. One factor is the area (A) of the alveolar-capillary membrane, which consists of the alveolar and capillary walls. The greater the area, the greater the rate of transfer and the higher the DL. Area is influenced by the number of blood-containing capillaries in the alveolar wall. The second factor is the thickness (T) of the membrane. The thicker the membrane, the lower the Dl. The third factor is the driving pressure, that is, the difference in oxygen tension between the alveolar gas and the venous blood (ΔPO2). Alveolar oxygen tension is higher than that in the deoxygenated venous blood of the pulmonary artery. The greater this difference (ΔPO2), the more oxygen transferred. These relations can be expressed as
4A. The Diffusing Capacity for Carbon Monoxide
The diffusing capacity of oxygen (DLO2) can be measured directly, but this is technically extremely difficult. Measuring the diffusing capacity of carbon monoxide (DLCO) is much easier and provides a valid reflection of the diffusion of oxygen. In essence, the difference between alveolar and venous carbon monoxide tension (ΔPCO) is substituted for oxygen in Eq. 1.
Several techniques for estimating DLCO have been described. The most widely used is the single-breath (SB) method (SBDLCO). The subject exhales to residual volume and then inhales a gas mixture containing a very low concentration of carbon monoxide (CO) plus an inert gas, usually helium. After a maximal inhalation, the patient holds his or her breath for 10 seconds and then exhales completely. During the breath hold, CO is absorbed while helium is equilibrating with alveolar gas. A sample of exhaled alveolar gas is collected and analyzed. By measuring the concentration of the exhaled CO and helium, the value of the DLCO can be computed.
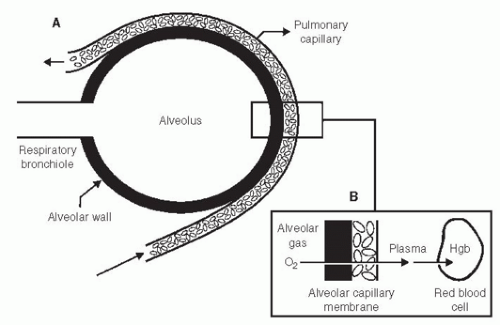 FIG. 4-1. A. Alveolar-capillary membrane through which oxygen must diffuse to enter the blood. In (B), alveolar wall is represented by the black rectangle. Hgb, hemoglobin. |
The helium is used to calculate the alveolar volume, which is nearly equivalent to the total lung capacity (TLC). The exhaled CO is used to calculate the amount of CO transferred to the blood.
DLCO is expressed in milliliters of CO absorbed per minute per mmHg of driving pressure (the difference between partial pressure in alveolar gas and the blood).
The technical details of measurement of SBDLCO are complex. To improve accuracy and reproducibility of testing among laboratories, the American Thoracic Society has established standards for performance of the test.1,2
4B. Normal Values of DLCO
An average normal value is 20 to 30 mL/min/mm Hg; that is, 20 to 30 mL CO is transferred per minute per mm Hg difference in the driving pressure of CO, namely, the difference between the partial pressure of CO in alveolar air and blood. The normal values depend on age (decrease with aging), sex (slightly lower in females), and size (taller people have larger lungs and therefore a higher DLCO). The inclusion of helium provides an estimate of total alveolar volume (VA). Dividing DLCO by VA tends to normalize for difference in size and therefore the DLCO/VA ratio (or Krogh constant) tends to be the same in various-sized normal subjects. To an extent in a given subject, the DLCO is also directly related to the volume of the inhaled breath. The smaller the volume, the lower the DLCO. The DLCO/VA in this situation would change little, however, if at all. This fact is useful, especially when repeated tests are
obtained over time. The volume inhaled might vary from year to year, but the DLCO/VA tends to correct for this. Most patients can hold their breath for 10 seconds, but some subjects with very small vital capacities cannot inhale a sufficient quantity of the gas mixture to give a valid test.
obtained over time. The volume inhaled might vary from year to year, but the DLCO/VA tends to correct for this. Most patients can hold their breath for 10 seconds, but some subjects with very small vital capacities cannot inhale a sufficient quantity of the gas mixture to give a valid test.
PEARL: In the healthy subject, the VA is essentially the same as the TLC and can be used as an estimate of TLC. The VA is also a good estimate of TLC in most restrictive conditions. With obstructive disease, VA underestimates TLC, just as the nitrogen washout and inert gas dilution techniques do (see Section 3C, page 25). However, TLC obtained with plethysmography minus the VA provides an estimate of the severity of nonuniform gas distribution, that is, the volume of poorly ventilated lung (see Chapter 3, first Pearl, page 34).
4C. Causes of Increased DLCO
Usually, an increased DLCO is not a concern. However, there are some interesting causes of an increased DLCO, as follows:
Supine position: Rarely is the DLCO measured while the subject is supine, but this position produces a higher value because of increased perfusion and blood volume of the upper lobes.
Exercise: It is difficult to hold one’s breath for 10 seconds during exercise. When this is done just after exercise, however, DLCO is increased because of increased pulmonary blood volumes.
Asthma: Some patients with asthma, especially when symptom-free, have an increased DLCO, possibly because of more uniform distribution of pulmonary blood flow.
Obesity: The DLCO can be increased in obese persons, especially those who are massively obese. This increase is thought to be due to an increased pulmonary blood volume.
Polycythemia: This is an increase in capillary red cell mass. This essentially amounts to an increase in area (A) in Eq. 1.
Intra-alveolar hemorrhage: In conditions such as Goodpasture syndrome, the hemoglobin in the alveoli combines with CO to produce an artificially high uptake of CO, which causes an increase in the calculated DLCO. Indeed, sequential DLCO measurements have been used to follow increases or decreases in intra-alveolar hemorrhage.
Left-to-right intracardiac shunts: These lead to an increased pulmonary capillary volume.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


