Diffuse Pleural Thickening
Jeffrey P. Kanne, MD
DIFFERENTIAL DIAGNOSIS
Common
Exudative Pleural Effusion
Empyema
Asbestos-related Pleural Disease
Hemothorax
Thoracotomy
Less Common
Pleural Metastasis
Radiation-induced Lung Disease
Systemic Lupus Erythematosus
Rheumatoid Arthritis
Pleurodesis
Rare but Important
Intrathoracic Drug Reaction
Malignant Mesothelioma
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Definition of diffuse pleural thickening not standardized
Commonly used definitions
Radiography
Extends more than 25% of chest wall
> 5 mm thickness at least at 1 site
Often involves costophrenic sulcus
CT
> 5 cm wide
> 8 cm craniocaudad extent
> 3 mm thick
Less rigorous criteria may be appropriate
Lesser degree of pleural thickening may be functionally significant
Extrapleural fat can mimic diffuse pleural thickening (fat attenuation)
Typically bilateral, symmetric, sparing costophrenic sulcus
Often associated with parenchymal bands and rounded atelectasis
Helpful Clues for Common Diagnoses
Exudative Pleural Effusion
Usually unilateral
Pleural thickening is late finding
Persists despite resolution of pleural effusion
Adjacent pneumonia or other pulmonary inflammation may present initially
Streptococcal and staphylococcal species most common
Nosocomial infection with gram-negative anaerobes and methicillin-resistant Staphylococcus aureus (MRSA)
Can calcify over time, though uncommon
Empyema
Tuberculosis and streptococcal pneumonia most common causes
Usually unilateral
Pleural thickening is late finding
Adjacent pneumonia or other pulmonary inflammation may initially be present
Extensive calcification most commonly from tuberculosis
Asbestos-related Pleural Disease
10% of asbestos-exposed individuals affected
Distinct from pleural plaques
Affects primarily visceral pleura
Bilateral involvement more common than unilateral involvement
Often associated with significant restrictive respiratory impairment
Often associated with parenchymal bands and rounded atelectasis
Hemothorax
Usually unilateral
Blunt or penetrating trauma
Iatrogenic
Parietal or visceral pleural thickening
Can develop rather quickly
Varying amount of residual pleural fluid
May calcify over time
Adjacent rib fractures suggestive
Thoracotomy
Mild residual pleural thickening common
Usually smooth, mild thickening
Can result from postoperative hemothorax
Helpful Clues for Less Common Diagnoses
Pleural Metastasis
˜ 90% of all pleural neoplasms
Lung carcinoma leading cause
Breast, ovary, and gastric carcinomas and lymphoma also common causes
Usually multiple
Can simulate benign pleural disease
Nodular, circumferential, and mediastinal pleural involvement suggestive of malignancy
Associated pleural effusion common
Can have lung or thoracic lymph node metastases
Radiation-induced Lung Disease
Usually complication of radiation therapy for breast cancer, lung cancer, or lymphoma
Small residual pleural effusion may be present
Radiation-induced lung fibrosis often present in radiation field
Systemic Lupus Erythematosus
Pleural thickening most common intrathoracic manifestation
Occurs in up to 30% in autopsy series
Unilateral more common than bilateral
Pleural effusion frequently present
Rheumatoid Arthritis
Pleural diseases are most common intrathoracic manifestation
40-70% pleural involvement in autopsy series
Pleural effusion may accompany pleural thickening
Unilateral more common than bilateral
Pleurodesis
Variable degrees of pleural thickening and nodularity
Remain stable over time
May enhance with large amount of granulation tissue
Residual loculations of fluid common
High-attenuation deposits (from talc) mimic pleural calcification
Usually adjacent to dependent lung
May be lentiform
Helpful Clues for Rare Diagnoses
Intrathoracic Drug Reaction
Numerous drugs linked to pleural effusions and thickening
Common agents include
Nitrofurantoin
Bromocriptine
Amiodarone
Procarbazine
Methotrexate
Bleomycin
Mitomycin
Dantrolene
Bilateral more common than unilateral
Generally resolve after cessation of therapy
Malignant Mesothelioma
Most result from asbestos exposure
Latency of up to 40 years
Can simulate benign pleural disease
Nodular, circumferential, and mediastinal pleural involvement suggestive of malignancy
Mediastinum relatively “fixed” with little or no shift
Presence of pleural plaques biomarker of exposure
Associated pleural effusion may be present
Extrapleural spread
Chest wall, mediastinum, diaphragm
Image Gallery
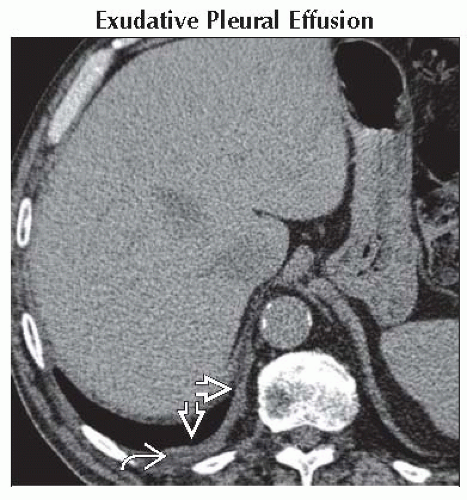 Axial NECT shows smooth right posterobasal pleural thickening
 with tiny residual effusion with tiny residual effusion  in this patient with recent pneumonia and parapneumonic effusion. in this patient with recent pneumonia and parapneumonic effusion.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|