Fig. 24.1
The preoperative left coronary angiogram clearly demonstrated severe diffuse coronary artery disease. The LAD was totally occluded and its distal portion was not filled via any collaterals. The circumflex artery was tightly stenotic and the distal portions were diffusely diseased

Fig. 24.2
The left coronary arteriogram (left anterior oblique with cranial angulation) revealed severe diffuse atherosclerosis of whole left coronary artery system. Total occlusion of the proximal LAD, severe diffuse stenoses in diagonal, proximal circumflex, and three marginal branches were noted
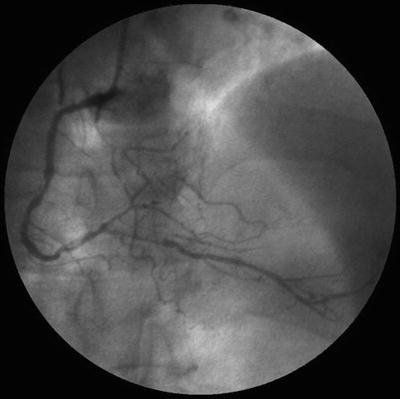
Fig. 24.3
The right coronary artery had multiple severe eccentric stenoses at its mid portion, its distal portion, and the proximal portion of PDA
Under general anesthesia, the left and right internal thoracic arteries and the right gastroepiploic artery were harvested in the skeletonized fashion and wrapped with papaverine-soaked sponge and divided, and PDE III inhibitor was instilled within it. The LAD was carefully identified by close inspection of the anterior wall and found to be diffusely sclerotic small vessel. The target site was chosen for the best arterial wall quality. Marginal branches of the circumflex and the posterior descending artery were also found to be diffusely diseased. These were only 1.0–1.5 mm vessels and not favorable but possible for grafting.
The LAD was opened first. Internal lumen was 1.5 mm. End-to-side anastomosis was constructed using the pedicled RITA with a 7–0 polypropylene running suture. The pedicled LITA was used as a sequential graft to revascularize the two obtuse marginal branches. Both were 1.5 mm in diameter with a mildly diseased wall. The first marginal branch was grafted in side-to-side diamond fashion. Lastly, the GEA was used as a sequential graft to revascularize the posterior descending artery and the distal portion of the circumflex. Both anastomoses were constructed using 7–0 polypropylene running sutures. The PDA was grafted in side-to-side parallel fashion.
He recovered and discharged home uneventfully. Coronary angiography performed at 1 week after surgery demonstrated widely patent coronary anastomoses with excellent flow and distal runoff (Figs. 24.4, 24.5, and 24.6) and markedly improved the left ventricular function.
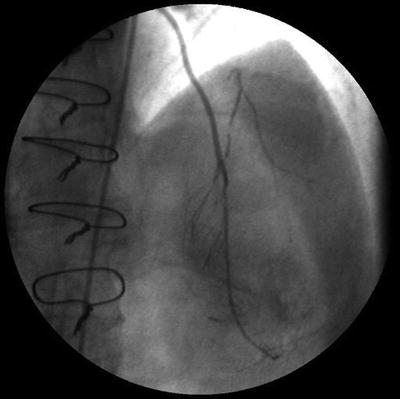


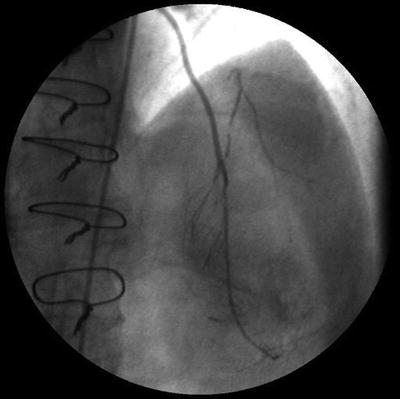
Fig. 24.4
The skeletonized right ITA was grafted to the distal LAD, totally occluded vessel. It was patent with septal branches and a diagonal branch nicely visualized

Fig. 24.5
The postoperative angiogram of the skeletonized left ITA graft demonstrated patency for sequentially bypassed the first and the second obtuse marginal branches of the circumflex artery

Fig. 24.6
The postoperative angiogram of the skeletonized RGEA graft demonstrated patency for sequentially bypassed the PDA and the distal portion of the circumflex artery
24.4 Stented Coronary Arteries
The stented coronary arteries are currently observed in more than 40 % of CABG candidates in our practice. With advent of the drug-eluting stent (DES), percutaneous coronary intervention (PCI) has been widely used for coronary revascularization. However, PCI itself cannot slow down the progressive process of coronary atherosclerosis and some patients are referred for CABG. These patients are generally more elderly, have more advanced and complex disease, and subsequently have smaller-sized target coronary arteries. They often have history of MI and are mostly on dual antiplatelet therapy (DAPT).
We observed specific patterns of lesions related to stented coronary arteries. First, “abrupt occlusion” is an in-stent lesion of the trunk of the stented vessel. This could be caused by stent thrombosis or progression of the atherosclerosis. Second, “in-segment stenosis” sometimes occurs in area outside of stented portion, but just close to the stent. It is the most stressed area with the heartbeat movement. Third, diffuse long segmental stenosis is also common among patients with progressive disease. Fourth, “candy wrapper stenosis” is often observed, just proximal or orifice location at branches of the stented coronary artery. Cardiologists often call these vessels “jailed” branches simply because metal strut of the stent caused jail-like appearance for its branch. These four patterns and progressive new atherosclerotic lesions were commonly observed.
At the time of the surgical revascularization, the stented portions of the coronary arteries are not the best site for the anastomosis of bypass conduits. The specific problems caused by coronary stentings are as follows. We need to make arteriotomy more distal and thinner sized area than that of ordinary cases. We occasionally need to make more number of distal anastomoses due to each major branch separately having tight “candy wrapper” stenosis. Mild stenosis at the in-stent site may preserve some blood flow through it; arterial grafting may be unpredictable in terms of long-term patency. We generally avoid endarterectomy with the stent removal in our practice unless it is necessary. This exposes thrombogenic media and inflamed vessel at the site of anastomosis, which would certainly increase the risk for early graft occlusion as well as native coronary thrombosis. There is no gold standard for surgical revascularization for stented coronary artery. These patients are treated individually, with special care. OPCAB for these patients is technically demanding and tactically complex even with experienced surgeons.
24.4.1 Case Presentation
A 67-year-old diabetic woman has repeatedly received percutaneous coronary intervention for recurrent angina caused by repeated in-stent restenoses during the last 2 years (over 15 times). The latest coronary angiography revealed a total of thirteen stents filling the proximal to middle portions of the three coronary territories (Figs. 24.7, 24.8, and 24.9) and in-stent total occlusion lesions in the middle portion of the LAD and the ostium of the right coronary artery. The obtuse marginal branch was also jailed by a stent (Figs. 24.10, 24.11, and 24.12). She successfully underwent off-pump CABG with in situ left internal thoracic artery graft to the second diagonal branch and the LAD; saphenous vein graft to the first diagonal branch, the OM, and the distal circumflex artery; and in situ gastroepiploic artery graft to the posterior descending artery. She recovered uneventfully, was discharged home after 2 weeks, and was followed in the outpatient clinic.




