2 Differences between Medical Thoracoscopy/Pleuroscopy and Surgical Thoracoscopy/Video-assisted Thoracic Surgery
As already explained in Chapter 1, two different techniques have emerged, video-assisted thoracoscopic surgery (VATS) and medical thoracoscopy/pleuroscopy (MT/ P). VATS is performed in an operating room under general anesthesia with selective intubation. For MT/P the patient does not need to be intubated and usually breathes spontaneously with moderate sedation and local anesthesia. The main differences between the two techniques are listed in Table 2.1. However, we feel that it is appropriate to explain the differences in the techniques as well as in the indications of MT/P and VATS in more detail because appreciation of the precise distinction between the two procedures is sometimes lacking.
A variety of definitions for MT/P have now emerged. In a paper in the New England Journal of Medicine it is given as follows:
Pleuroscopy as performed by interventional pulmonologists differs from video-assisted thoracic surgery, in that local anesthesia and conscious sedation are most often used in lieu of general anesthesia, a single thoracic puncture is made rather than multiple incisions, and the procedure can be safely performed in an ambulatory care setting. Although pleuroscopy is primarily used for the diagnosis and management of pleural disorders, it can also be used to perform lung biopsy and manage spontaneous pneumothorax. Mortality rates associated with pleuroscopy are extremely low, ranging from 0.01-0.24%. Complications of the procedure include bleeding, persistent pneumothorax, and intercostal nerve or vessel injury. (Seijo and Sterman 2001)
Table 2.1 Main differences between medical thoracoscopy/pleuroscopy versus surgical thoracoscopy/video-assisted thoracic surgery (VATS)
Feature | Medical thoracoscopy/pleuroscopy | VATS |
|---|---|---|
Purpose | Diagnosis | Minimally invasive thoracic surgery |
Location | Endoscope suite | Operating room |
Anesthesia | Local with moderate sedation | Single-lung ventilation |
Technique | Single puncture | Multiple punctures |
Instruments | Nondisposable Simple | Disposable Complex |
Another definition is mentioned in the ACCP Guidelines on “Interventional Pulmonary Procedures”:
Medical thoracoscopy/pleuroscopy is a minimally invasive procedure that allows access to the pleural space using a combination of viewing and working instruments. It also allows for basic diagnostic (undiagnosed pleural fluid or pleural thickening) and therapeutic procedures (pleurodesis) to be performed safely. This procedure is distinct from video-assisted thoracoscopic surgery, an invasive procedure that uses a sophisticated access platform and multiple ports for separate viewing and working instruments to access pleural space. It requires one-lung ventilation for adequate creation of a working space in the hemithorax. Complete visualization of the entire hemithorax, multiple angles of attack to pleural, pulmonary (parenchymal), and mediastinal pathology with the ability to introduce multiple instruments into the operative field allow for both basic and advanced procedures to be performed safely. (Ernst et al. 2003)
Video-assisted Thoracic Surgery (VATS)
The indications for VATS are different from those for MT/P, although there are some gray zones with overlapping indications for both techniques (Table 2.2).
Surgeons can be more ambitious since they are able to perform thoracotomy promptly if needed. Many operations traditionally performed via thoracotomy can now be done using VATS (LoCicero 1992; Miller et al. 1992; McKenna 2000; Yim et al. 2001; Loddenkemper and McKenna 2005). VATS involves the use of small incisions to perform therapeutic interventions in the chest without spreading the ribs. The surgeon generally needs at least three entry sites (Fig.2.1). However, it often may become necessary to perform an additional minithoracotomy, 5-7 cm long, to remove large specimens. VATS, which takes its roots from MT/P, has now been technically developed so far that it can replace thoracotomy in almost all indications, if certain limitations such as dense pleural symphysis are not present. VATS requires an operating room, general anesthesia with single-lung ventilation, more than two—usually three—entry sites, and complex instruments. It is a more invasive and expensive technique with a higher risk.
Table 2.2 Indications for medical thoracoscopy/pleuroscopy (MT/P) versus surgical thoracoscopy (VATS) versus the middle column where both methods can be used
MT/P | MT/P or VATS | VATS |
|---|---|---|
Pleural effusions | Spontaneous pneumothorax | Lung procedures |
Pleural effusions of unknown etiology | Staging | Lung biopsy |
Staging of lung cancer | Pleurodesis by talc poudrage | Lobectomy |
Staging of diffuse malignant mesothelioma | Empyema (stage I/II) | Pneumonectomy |
Pleurodesis by talc poudrage or any other agent | Drainage | Decortication |
Diffuse pulmonary diseases | Lung volume reduction surgery | |
Localized lesions | Pleura procedures | |
Chest wall, diaphragm | Pleurectomy (pneumothorax) | |
Sympathectomy, splanchnicectomy | Drainage/decortication (empyema stage III) | |
Esophageal procedures | ||
Excision of cyst, benign tumors, esophagectomy, anti-reflux procedures, mediastinal procedures | ||
Resection of mediastinal mass | ||
Thoracic duct ligation | ||
Pericardial window | ||
Sympathectomy |
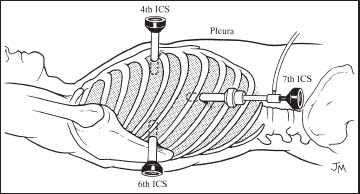
Fig. 2.1 Schematic drawing of the VATS access through three entry sites. (From Beamis JF Jr, Mathur PN, eds. Interventional Pulmonology. New York: McGraw-Hill; 1999. Reprinted with kind permission of McGraw Hill.)
The procedures that can be performed by VATS are on the lung, esophagus, heart, pleural space, and mediastinum. This would include resection of lung mass; bullectomy, pleurectomy, pleural abrasion; collection of biopsy samples from thoracic lymph nodes from the mediastinum and hilus; resection of mediastinal cysts; drainage of vertebral abscess; treatment of bronchopleural fistula, lobectomy, pneumonectomy and esophagectomy, and some further procedures. The scope of indications is gradually being extended to include almost all the surgical indications. In most cases the benefits for the patient are obvious in terms of postoperative pain, hospital stay, and recovery. However, it has a higher initial cost than open thoracotomy (Van Schil 2003). It has also been performed as an outpatient procedure (Molins et al. 2006; McKenna et al. 2007). Chronic pain after VATS is not uncommon. Persistant pain was observed 3-18 months after VATS (36%) as often as after thoracotomy (33%) in patients undergoing lung resections (Furrer et al. 1997). A similar incidence of chronic pain (32%) was seen after VATS performed for spontaneous pneumothorax (Passlick et al. 2001).
MT/P, on the other hand, is used mainly for diagnostic purposes in pleural diseases. The most common indications for pleuroscopy are diagnosis of pleural effusion with inspection of the pleural cavity, combined with biopsies from the parietal and visceral pleura, as well as treatment of malignant or other therapy-refractory effusions by talc pleurodesis (poudrage). There are also some further indications as shown in the following chapters.
General Approach to VATS Procedures
VATS procedures, compared with a thoracotomy, allow a minimally invasive approach that will reduce the morbidity and mortality for patients and will allow a quicker return to normal activities. Increasing evidence suggests that this is true. VATS should be a standard complete operation done for the standard indications and is not a compromised operation. VATS lobectomy does allow a standard complete anatomical resection of the lobe with lymph node sampling or dissection (McKenna 1994; Howington 2007). A variety of equipment is available for VATS. Instruments used may be instruments designed for laparoscopy, instruments designed for thoracoscopy, or standard instruments that are used for open procedures. There are many disposable endoscopic instruments that are used, but some may prefer to use standard instruments for open thoracic procedures (Rocco et al. 2008). Even robotic systems have been applied in VATS (Al-Muffarej et al. 2010).
Anesthesia
VATS is performed under general anesthesia with one-lung ventilation and collapse of the other lung, which gives good exposure. Single-lung ventilation is performed by the use of a double-lumen tube or more commonly with the use of bronchial blockers. Unlike with a laparotomy, there is no need for carbon dioxide insufflation into the pleural space. It is important that the pleural space is not insufflated under positive pressure, so as not to create a tension pneumothorax. Most thoracic surgeons have their own variation along with their anesthetist. Most important is that this unit has to work as a team and its members must understand each other’s needs.
Indications and Contraindications
Most thoracic surgery can now be performed with VATS, provided the necessary training is completed and the practice guidelines for VATS are observed, such as those proposed by the Society of Thoracic Surgeons (McKneally et al. 1992; Society of Thoracic Surgeons 1994; Kaiser 1994 b).
For example, a large number of lobectomies are performed by VATS. The surgeon has to determine when a thoracotomy or VATS is appropriate. Basically, the choice of procedure is based on the goal of the operation. Certain situations may require a thoracotomy: a mass attached to the chest wall that requires resection of the mass and the ribs, or a mass that is too large for removal through a small incision; suturing requirements beyond the skills of the surgeon; and pleural adhesions from chemotherapy, radiation therapy, or infection that make dissection more difficult.
Certain procedures can be performed either way, such as an open lung biopsy. However, if the patient is unable to tolerate single-lung ventilation it may be more appropriate to perform a thoracotomy. Surgeons should understand their own limitations; these may include skills in operating with video assistance, though these skills will improve with time. The ability of general surgeons (non-thoracic surgeons) with their abdominal surgery video skills has brought several nonthoracic surgeons into dabbling in thoracic surgery.
Lung Procedures Performed with VATS
Almost all pulmonary procedures can be performed with VATS and currently it is a common skill for thoracic surgeons. They should understand their own technical limitations, however.
Lung Biopsy
Lung biopsy is the most common procedure performed by VATS (Ayed 2003; Qureshi et al. 2007). This usually involves three standard incisions, which generally do not vary except that the incision in the mid-axillary line may be in the fourth intercostal space or the fifth intercostal space for interstitial lung diseases or parenchymal infections. An endoscopic stapler is used to resect the appropriate area of lung parenchyma.
Wedge Resection
Careful inspection of the preoperative chest CT scan is extremely important to allow the surgeon to know where the mass is located. All masses can be palpated because the lung is a very mobile organ. The mass can then be manipulated by forceps and grasper. When resected, the mass should be placed into a bag for removal through the utility incision to prevent tumor seeding.
A variety of new techniques have emerged for preoperative localization of a mass, such as wire localization, or use of dye or of radioisotopes under certain circumstances (Mack et al. 1993). If the mass is small (< 1 cm), more than 1 cm below the pleural surface, or a ground-glass opacity that would be soft and difficult to palpate, the radiologist can place a hook wire under CT guidance. The wire should then be cut at skin level. The patient then goes to the operating room for the VATS procedure. The surgeon resects the area of lung within the hook wire. An endoscopic stapler is used to resect the appropriate area of lung parenchyma. VATS wedge resection is a procedure very commonly performed by surgeons. The morbidity and mortality are extremely low.
Pulmonary Metastases
VATS can be used for either the diagnosis or the treatment of pulmonary metastases(Mack et al. 1993; Lenglinger et al. 1994; Burdine et al. 2002; Mutsaerts et al. 2002; Pittet et al. 2007; Gonfiotti et al. 2007; Treasure et al. 2008). The procedure is performed with the standard technique for a wedge resection. If the intent of the procedure is therapeutic, careful, complete palpation is imperative because additional lesions, not identified on CT scan, are found in approximately 30% of patients. This indication for VATS is controversial because some surgeons question how well the entire lung can be examined during a VATS procedure. The advent of thin-cut CT scans, allows much better visualization of pulmonary lesions that otherwise could only be palpated.
Lobectomy
Although most surgeons perform lobectomies via a thoracotomy incision, there is now a large and growing worldwide experience with VATS lobectomy to suggest that the VATS approach may have advantages over an open lobectomy (McKenna 1998; Nakajima et al. 2000; Hoksch et al. 2003; Li et al. 2003; Nomori et al. 2003; Shigemura et al. 2006; Shigemura and Yim 2007; Swanson et al. 2007; Whit-son et al. 2007; Balderson and D’Amico 2008; Congregado etal.2008; Solaini et al. 2008; Iwasaki et al. 2008; Mahtabifard et al. 2008; Park and Flores 2008; Reed et al. 2008).
This standard procedure should involve a complete anatomical dissection and removal of lymph nodes. Generally an 8-mm trocar and thoracoscope are placed in the mid-axillary line of the eighth intercostal space. This is followed by a 2-cm incision which is placed in the mid-clavicular line of the sixth intercostal space. The utility incision is an incision of approximately 4-5 cm in the fourth or fifth intercostal space in the mid-axillary line. Standard instruments are used to dissect and transect the artery, vein, and bronchus for the lobe to be removed. The mortality rate with VATS is less than 1% (Mack et al. 1993; Qureshi et al. 2007), it has a lower complication rate (Qureshi et al. 2007), lower costs (Li et al. 2003), less impairment of shoulder function (Nomori et al. 2003), no significant impact on the vital capacity and 6-minute walk (Fishman et al. 2003), and less use of postoperative analgesics. Long-term survival of either VATS lobectomy or an open procedure is the same; thus, when appropriate, if the surgeon is familiar with VATS lobectomy it may be the preferred operation (McKenna 1998; Fishman et al. 2003; Shigemura et al. 2006; Iwasaki et al. 2008; Park and Flores 2008). The important issue is that proper mediastinal dissection has to be performed. Thoracic surgeons with good skills have little difficulty with dissection of pulmonary vessels and controlling bleeding. To reduce tumor seeding at the site of the incisions, the mass has to be placed in a bag prior to removal.
Lung Volume Reduction Surgery
Lung volume reduction surgery (LVRS) is an effective treatment for selected patients with emphysema (Fishman et al. 2003). It has been successful in patients who have failed medical management and have an upper-lobe heterogeneous pattern of emphysema. LVRS carries a hospital mortality and morbidity rate of approximately 5% (Fishman et al. 2003). In a selected group of patients when compared with medical management, LVRS provides better exercise tolerance, pulmonary function, and quality of life. LVRS provides increased survival for patients with upper lobe emphysema and low exercise tolerance. LVRS involves resection of approximately 30% of the parenchyma of each lung. The National Emphysema Treatment Trial (NETT) showed that LVRS can be performed with equal efficacy by VATS and by thoracotomy via median sternotomy, but the VATS approach provided easier recovery with less expense.
LVRS can also be performed by VATS, with the patient in the lateral decubitus position. The standard three incisions are used. The lung is held with a forceps through the incision in the fourth intercostal space and the stapler enters the chest through the incision in the sixth intercostal space in the mid-clavicular line. As the emphysematous parenchyma does not hold staples well, some form of buttress is needed to prevent air leaks. The thoracic surgeon has to determine the location and amount of lung tissue to be resected. The preoperative CT scan and ventilation and perfusion scans can be helpful in the determination.
Pleural Procedures Performed with VATS
Treatment of Pneumothorax
VATS has proved a good approach for the treatment of spontaneous pneumothorax. It is performed when there is persistent leak, bilateral pneumothorax, or recurrent spontaneous pneumothorax. The standard incisions are used and the lungs are carefully inspected to identify the bleb that has caused the pneumothorax. The bleb and a margin of normal lung tissue are excised with staples. A mechanical pleurodesis is performed with a ring forceps that holds a gauze pad or the scratch pad used for the electrocautery. Long-term success for this procedure is 90-95%. However, there is controversy attached to this approach as the blebs seem not to be responsible for the pneumothorax.
Another pleural procedure may be indicated for catamenial pneumothorax, recurrent pneumothorax after surgical treatment, or when a bleb is not found. Then, a more aggressive pleural procedure, either a talc pleurodesis or a parietal pleurectomy, is performed (Boutin et al. 1995 a; Schramel et al. 1997; Ayed et al. 2006; Noppen et al. 2006; Tschopp et al. 2006; Amjadi et al. 2007; Barker et al. 2007; Cardillo et al. 2007; Vohra et al. 2008).
However, the management of pneumothorax is also an excellent indication for MT/P, which is outlined in the section “The Place of Medical Thoracoscopy/Pleuroscopy in the Management of Pneumothorax,” Chapter 3, p. 41 ff.
Pleural effusions are the domain of MT/P, for diagnostic purposes as well as for talc pleurodesis. It can also be successfully used in early empyema cases. The latter use is described in detail in Chapter 3 on indications for medical thoracoscopy/pleuroscopy (“Parapneumonic Effusions and Pleural Empyema,” Chapter 3, p. 31 f.).
Decortication
VATS has been used successfully in the treatment of empyema, especially in the later stages (Angelillo-Mackinlay et al. 1999; Cameron 2002; Chen et al. 2002; Hampson et al. 2008; Luhetal.2008; Medfordetal.2008). Generally, theef-fusion is drained by either large-bore or small-bore chest tubes. If the purulent effusion (empyema) cannot be drained due to multiple loculations, the patient remains febrile, and more conservative therapies including antibiotics are failing, VATS should be considered, in particular when decortication is needed (empyema stage III) and the patient does not have a high surgical risk. The thickened visceral pleura (peel) is incised and a blunt dissection is made by which the peel can be removed from the lung. Gentle ventilation and partial expansion of the lung facilitate this dissection. The process continues until there is a minimal amount of pleural debris and the lung fully reexpands to fill the entire pleural space. However, there are thoracic surgeons who find VATS a tedious operation and find a muscle-sparing thoracotomy to be an efficient way to complete the decortication.
Esophageal Procedures Performed with VATS
Excision of Cysts and Benign Tumors
VATS has also been used for masses in the middle mediastinum (esophageal leiomyomas (Li et al. 2009 b), esophageal duplication cysts, bronchogenic cysts, or pericardial cysts) or the posterior mediastinum (benign neurogenic tumors). For these procedures, the standard incisions are used, and the lung is retracted anteriorly. For an esophageal mass, the longitudinal muscles of the esophagus are separated and retracted laterally. The cyst or tumor is mobilized with a combination of blunt and sharp dissection. Retraction by placement of a suture into the tumor may help separate the tumor from the esophagus.
Anti-reflux Procedures
A significant number of Nissen fundoplications as an anti-reflux procedure are primarily performed with minimally invasive surgery (Grant et al. 2008; Chen et al. 2009; Hartmann et al. 2009; Vlug et al. 2009).
Esophagectomy
VATS can used for mobilization of the esophagus and an open trans-hiatal esophagectomy, or can be a totally minimally invasive procedure utilizing laparoscopy for gastric mobilization and feeding jejunostomy, VATS for esophageal mobilization, and a cervical incision for the esophago-gastrostomy. The technique for a minimally invasive esophagectomy has been well described (Perry et al. 2002). One randomized trial showed that the same operation and same node dissection can be achieved with equal survival. The ultimate role for the minimally invasive esophagectomy has yet to be defined. There is a significant learning curve for surgeons trying to master this technique (Perry et al. 2002; Osugi et al. 2003; Shichinohe et al. 2008).
Mediastinal Procedures
Thymectomy
Minimally invasive thymectomy has been performed for thymomas (Savcenko et al. 2002; Wright et al. 2002). Concern about spreading the tumor has led some surgeons to recommend a median sternotomy, rather than VATS, when a thymoma is present. However, VATS thymectomy for myasthenia gravis appears to offer results comparable with those of an open or transcervical thymectomy (Savcenko et al. 2002; Wright et al. 2002). The mean length of hospital stay for the VATS approach was 1.64 days (range 0-8 days) with a median stay of 1 day. The mean length of follow-up is 53 months (range 4-126 months). Overall, clinical improvement at follow-up was observed in 30 of 36 patients (83.0%), with 5 of 36 patients (14.0%) in complete stable remission (Savcenko et al. 2002).
Thoracic Duct Ligation
Patients with a chylothorax due to thoracic duct leakage can undergo ligation of the thoracic duct via VATS. The duct can then be identified as it crosses through the diaphragm by the right anterior surface of the aorta. Several clips are placed on the duct (Terashima et al. 2003).
Pericardial Window
A large pericardial window may be achieved through either the right or the left chest (O’Brien et al. 2005; Georghiou et al. 2005; Rocco et al. 2006). If there is a concomitant pleural effusion, the side of the pleural effusion should be chosen for the VATS so that a talc pleurodesis may be performed to control the pleural effusion.
Sympathectomy
Sympathectomy is the treatment of choice for the treatment of palmar hyperhidrosis (Noppen et al. 1995; Noppen and Vincken 1996). Affecting 1-2% of the population, palmar hyperhidrosis can be a severely debilitating and socially embarrassing disease. The procedure can be performed by both VATS or MT/P (see Chapter 3, p. 48–50). The procedure is performed under general anesthesia and can be done on an outpatient basis. As the patient is in the supine position with the arms extended, a bilateral procedure can be performed without repositioning the patient. A1 -cm incision is made in the anterior axillary line at the inferior margin of the hair line. A trocar and the thoracoscope are passed through the incision. There are several approaches for the procedure. Some surgeons resect part of the nerve or burn the ganglion, while others transect or clip the nerve. The results appear to be similar after all procedures. Many patients have accessory nerves, and an attempt is made to identify and transect these nerves. The lung is then reexpanded, and the procedure is performed on the opposite side. Complications after sympathectomy are infrequent. These include Horner syndrome (< 1 %) and bleeding (Boley et al. 2007; Krasna 2008; Marhold et al. 2008; Li et al. 2009 a; Martins Rua et al. 2009).
Thoracic Lymphadenectomy
A complete lymphadenectomy, usually done as part of a lung cancer operation, can be performed by VATS (Congregado et al. 2008). The incisions are, therefore, usually the same incisions that are used for lobectomy.
Paratracheal node dissection starts with inferior retraction of the lung. Blunt dissection along the trachea, the pericardium over the ascending aorta, and the superior vena cava mobilizes all of the level 2, 3, and 4 lymph nodes. Subcarinal node dissection starts with anterior retraction of the lung through the incision in the sixth intercostal space in the mid-clavicular line. Blunt dissection along the pericardium, esophagus, and both main-stem bronchi mobilizes the subcarinal nodes.
Cervical Mediastinoscopy versus VATS
Accurate staging is critical for determining the appropriate treatment for lung cancer. Cervical mediastinoscopy provides access for removal of paratracheal (level 2 and 4 nodes), pretracheal nodes (level 3), tracheobronchial angle/hilar nodes (level 10), and subcarinal nodes (level 7). The middle mediastinum is accessible to mediastinoscopy, but not the anterior mediastinal space. This procedure is performed through a 2-cm incision in the base of the neck. It is generally an outpatient procedure, done under general anesthesia (Karfis et al. 2008; Molins et al. 2008).
VATS has not replaced mediastinoscopy because the latter is a simpler procedure that does not require either hospitalization or a double-lumen tube. Therefore, if the goal of the procedure is biopsy of level 2, 3, 4, 7, and 10 nodes, mediastinoscopy is preferred over VATS.
Anterior Mediastinotomy versus VATS
Biopsy of an anterior mediastinal mass or level 5 and 6 nodes is often accomplished with an anterior mediastinotomy (Chamberlain procedure) (Landreneau et al. 1993). Removal of the cartilaginous portion of the left second rib provides excellent exposure for these areas.
VATS has not replaced anterior mediastinotomy because the latter is a simpler procedure that does not require either hospitalization or a double-lumen tube. Therefore, if the goal of the procedure is biopsy of level 5 and 6 nodes, anterior mediastinotomy is preferred over VATS.
Summary
MT/P compared with video-assisted thoracic surgery (VATS)/surgical thoracoscopy has the advantage that it can be performed under local anesthesia or conscious sedation, in an endoscopy suite, using nondisposable rigid instruments. Thus, it is considerably less expensive and, for the patient, less cumbersome.
MT/P procedures are safe procedures and are even easier to learn than flexible bronchoscopy, provided sufficient experience with chest tube placement has been gained. However, as with all technical procedures, there is a learning curve before full competence is achieved.
The main indications for MT/P are pleural effusions, in particular exudates of unknown etiology, or for staging in diffuse malignant mesothelioma or lung cancer, and for talc poudrage. But there are additional indications, which are outlined in the corresponding chapters.
VATS has made tremendous progress during the last decade. The advances in endoscopic technology, with sophisticated endoscopic instruments and endoscopic telescopes, allow the replacement of thoracotomy in many indications. Although it necessitates selective double-lumen intubation under general anesthesia, it is much less invasive, and increasing evidence suggests that it reduces the morbidity and mortality compared with thoracotomy. However, just as there is an overlap between MT/P and VATS procedures, there is also an overlap between VATS and open surgical procedures, and the decision between these procedures depends on the performance status and prognosis of the patient, as well as on the expertise of the thoracic surgeon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


