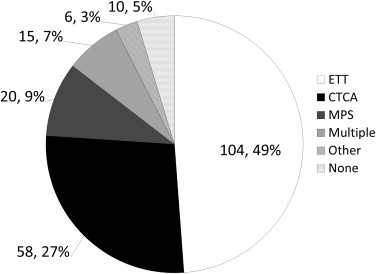
Contemporary professional society recommendations for patients presenting to the emergency department with acute chest pain and low clinical risk encourage noninvasive testing for coronary artery disease (CAD) before, or shortly after, discharge from the emergency department. Recent reports indicate that a strategy of universal testing has a low diagnostic yield and may not be necessary. We examined data from a prospective cohort of patients who underwent evaluation of acute chest pain in our chest pain evaluation center (CPEC). Patients presenting with normal initial electrocardiogram and cardiac injury markers were eligible for observation and noninvasive testing for CAD in our CPEC. All patients were asked to participate in the prospective registry. The 213 subjects who consented were young, obese, and predominantly women (mean age 43.8 ± 12.5, mean body mass index of 30.8 ± 7, 64.8% women). Prevalence of diabetes was 10.3% (hypertension 37.1%, hyperlipidemia 17.8%, and current tobacco use 23.5%) Exercise treadmill testing was the primary method of evaluation (n = 104, 49%) followed by computed tomography coronary angiography (n = 58, 27%) and myocardial perfusion imaging (n = 20, 9%). Of 203 patients who underwent testing, 11 had abnormal test results, 4 of whom had obstructive CAD based on invasive coronary angiography. The positive predictive value for obstructive CAD after an abnormal test was 45.5%, and the overall diagnostic yield for obstructive CAD was 2.5%. In conclusion, in patients with acute chest pain evaluated in a CPEC, the yield of routine use of noninvasive testing for CAD was minimal and the positive predictive value of an abnormal test was low.
Professional societies encourage provocative testing for low-risk chest pain patient during, or shortly after, an encounter in the emergency department (ED). Recent literature suggests that indiscriminate testing of these patients with chest pain has poor diagnostic performance. In 2011, our institution established a chest pain evaluation center (CPEC) within our ED. Patients in the CPEC were enrolled in a prospective registry to track the results of their cardiovascular evaluation. We determined the diagnostic yield of routine noninvasive cardiovascular testing in this contemporary, acute chest pain population preselected to be at low cardiovascular risk. We hypothesized that few patients would be diagnosed with coronary artery disease (CAD) and that the diagnostic yield of routine testing within this population would be low.
Methods
The design of our CPEC and the accompanying registry have been described previously. The CPEC has 8 bed spaces located within the ED at our medical center. The unit is staffed by a nurse practitioner or physician assistant with specialized training in assessment and management of patients with chest pain. Supervision is provided by a member of the ED faculty. Patients were selected for observation within the CPEC if they had no known heart disease and no evidence of ischemia based on initial electrocardiogram and biomarker testing. Selection of tests for CAD were guided by a custom decision support tool that helped estimate CAD risk using the patient’s symptoms, age, and risk factors. Anginal symptoms classified by the system by Diamond and Forrester were used for CPEC selection and collected in the registry. Advanced providers are trained to supervise exercise treadmill tests (ETTs), which are performed in the unit during weekdays from 8 am to 5 pm and from 8 am to 12 pm on weekend days. ETT is encouraged as the primary testing technique, whereas the primary noninvasive cardiovascular imaging test is computed tomographic coronary angiography (CTCA) performed on an Aquilion One CT scanner (Toshiba, Tustin, California) with 320 detectors and images reviewed on a Vital workstation (Vitrea, Minnetonka, Minnesota) by an interdisciplinary team of radiologists and cardiologists trained in CTCA. Nuclear myocardial perfusion imaging is also available on weekdays using technetium-99m single-photon emission computed tomography.
All patients in the CPEC were asked to participate in the CPEC registry. For those who agreed and provided written informed consent, data regarding the patient’s evaluation were recorded by research staff in a Web-based database using REDcap software (Vanderbilt University, Nashville, Tennessee). Data gathered included a detailed structured description of the patient’s symptoms, medical history, subsequent cardiovascular testing, and test results.
ETT were classified as ischemic, nonischemic, or uninterpretable by an attending cardiologist using standard criteria for ischemia: horizontal or downsloping ST depression ≥1.0 mm in contiguous leads, exercise-induced hypotension, or ventricular arrhythmias; Duke treadmill scores were also calculated. CTCA results were classified as normal (zero calcium and no coronary lesions), nonobstructive (all coronary lesions <50% stenosis), or obstructive (at least 1 lesion ≥50% stenosis). If images were nondiagnostic, the CTCA was not categorized. The “normal testing” group included all subjects with nonischemic ETT, those with normal or nonobstructive CTCA results, and those who did not undergo testing (i.e., their risk was so low as to not warrant testing). “Abnormal testing” was defined as all subjects with at least 1 abnormal test result: ischemic ETT, CTCA with obstructive CAD, or abnormal alternative testing. If a patient underwent more than 1 cardiovascular test or other noncardiac imaging tests (such as pulmonary embolus study or lower extremity Doppler), the patient was categorized as having multiple tests.
The primary outcome was the proportion of patients in the CPEC diagnosed with obstructive CAD after undergoing noninvasive testing. Secondarily, we compared patients with and without an abnormal test result by characteristics of their angina to determine any correlation between symptoms and test results. Proportions were compared by the chi-square test and continuous data by the Student’s t test. Statistical analyses were performed using SPSS, version 21 (IBM, Armonk, New York).
Results
A total of 213 subjects were evaluated in the CPEC and agreed to participate in the registry from December 2011 to April 2013. Approximately 20% of patients with chest pain presenting to our ED were treated in the CPEC, of which approximately 10% consented to participate in the registry. The following tests were performed: ETT for 104 (49%), CTCA for 58 (27%), other/multiple tests for 41 (19%), and no test for 10 (5%; Figure 1 ). The study population was young (mean age 43.8 years, range 20 to 67 years) with relatively low burden of cardiovascular risk factors ( Table 1 ).
| Age (years, mean ± SD) | 43.8 ± 12.5 |
| Body Mass Index (kg/m 2 ) | 30.8 ± 7.5 |
| Female | 138 (65%) |
| Diabetes Mellitus | 22 (10%) |
| Hypertension ∗ | 79 (37%) |
| Hyperlipidemia ∗ | 38 (18%) |
| Current Smoker | 50 (24%) |
| Aspirin | 14 (7%) |
| Statin | 14 (7%) |
| Beta Blocker | 13 (6%) |
∗ Hypertension and Hyperlipidemia were extracted as data fields from the electronic health record for each patient.
The numbers of each test performed exceed the number of patients in the study cohort because some patients underwent multiple tests. A total of 119 ETTs were performed, including those with ETT as the primary diagnostic strategy and some who underwent multiple tests. Only 4 ETTs demonstrated ischemia, whereas 96 were nonischemic and 19 were inconclusive. The mean Duke treadmill score was 6.6 (range −5 to 15). CTCA was performed in 71 subjects including 33 who were normal, 30 who had nonobstructive CAD, 6 who had obstructive CAD, and 1 who was inconclusive (because of mistiming of contrast bolus). Of 20 nuclear stress tests performed, only 1 had abnormal test result with a small fixed defect (summed stress score = 5, summed difference score = 0). A total of 6 patients underwent other imaging tests: 3 stress echocardiograms (none abnormal) and 3 noncardiac chest CTs. Testing was not performed for 10 of the subjects in the CPEC registry. One subject recently had normal test result at another facility, 4 were referred for outpatient follow-up, 1 left against medical advice, and the remaining 4 were felt to clinically not warrant any additional testing.
A total of 11 patients had abnormal test results ( Table 2 ). Subsequent invasive coronary angiography was performed in 8 patients. One patient with a fixed defect on myocardial perfusion imaging did not undergo invasive angiography was presumed to have CAD and was treated medically. In total, 5 patients were diagnosed with obstructive CAD for a diagnostic yield of 2.5% (5 of 203). Ten patients who did not undergo testing were not included in our calculation. The positive predictive value of noninvasive testing in this low-risk population was 46% (5 of 11). When we compared patients with and without abnormal test results based on angina duration, CAD risk, and symptom characteristics, none of the comparisons were significant (p = 0.8, 0.078, and 0.18, respectively; Table 3 ).
| Age (years) | BMI (kg/m 2 ) | Gender | DM | SH | HLD | CS | DST ∗ | D&F † | Abnormal test | Coronary Angiography | Obstructive CAD |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 52 | 30.5 | F | – | + | – | – | Intermediate | Typical | CTCA | + | 0 |
| 47 | 24.4 | M | – | + | – | – | Intermediate | Noncardiac | ETT | + | 0 |
| 50 | 17.9 | F | – | + | – | – | Intermediate | Atypical | CTCA | + | + |
| 30 | 23.9 | F | – | – | – | – | Low | Typical | ETT | 0 | 0 |
| 48 | 42.5 | F | + | – | – | – | High | Noncardiac | MPI | 0 | + |
| 57 | 29.0 | M | – | + | – | + | High | Noncardiac | CTCA | + | 0 |
| 55 | 33.8 | M | – | – | + | – | Intermediate | Typical | ETT | + | + |
| 35 | 29.4 | M | – | – | – | – | Low | Atypical | CTCA | + | 0 |
| 58 | 41.9 | M | – | + | + | – | Low | Atypical | CTCA | + | + |
| 43 | 26.4 | M | – | + | – | + | Low | Atypical | ETT | 0 | 0 |
| 47 | 25.6 | F | – | – | – | + | Intermediate | Atypical | CTCA | + | 0 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


