The goal should be to use the lowest dose and volume of contrast necessary for adequate clinical angiography. Broadly, there are two types of agents, high-osmolality and low-osmolality agents. The major resistance to the use of low-osmolality agents used to be expense, but recent price reductions have made this a relative nonissue. High-osmolality agents are rarely used in practice now. Third-generation nonionic contrast agents reduce osmolality even further by creating a dimer. Iodixanol is a dimeric contrast agent in this class and is iso-osmolal with plasma. Nonionic, low osmolal contrast agents are now routinely used for angiography. Individuals with prior significant contrast reactions, active asthma, severe congestive heart failure, active significant arrhythmia, aortic stenosis, pulmonary hypertension, or significant renal dysfunction (serum creatinine greater than 2 mg/dL) should receive a low-osmolal or preferably an iso-osmolal agent. For diagnostic vascular angiography, we use an iso-osmolal agent iodixanol (Visipaque, GE Healthcare, Little Chalfont, Buckinghamshire) that has been shown to cause significantly less discomfort for patients and also significantly reduces the relative risk of developing contrast media-induced renal failure. In individuals with prior severe allergic reaction to contrast agents, gadolinium can be used for angiography using digital subtraction angiography (DSA) provided GFR is greater than 30 mL/min. Carbon dioxide has a limited role as a vascular contrast agent because of poor opacification of the vessels despite use of DSA.
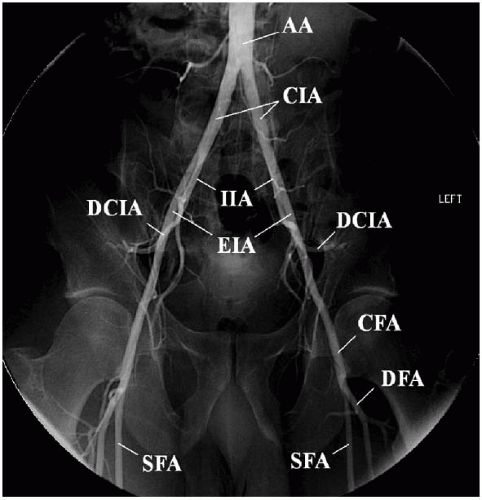
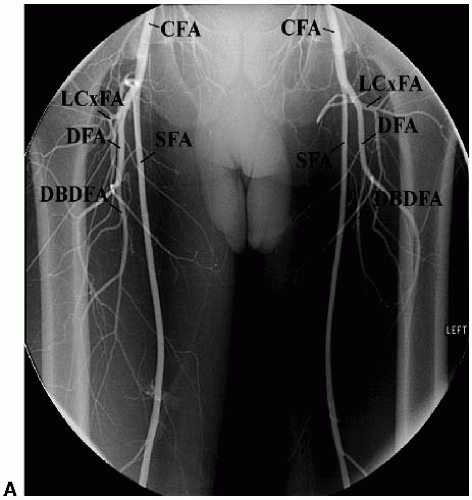
is recommended (Fig. 3.3B). The bolus chase technology combines the advantages of digital subtraction and step table technology. Mask images are obtained prior to acquisition of contrast images to further accentuate the arterial tree. Figure 3.4 is a schematic of the arterial supply to the lower extremities.
TABLE 3.1 RECOMMENDATIONS FOR DIAGNOSTIC VASCULAR ANGIOGRAPHY | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
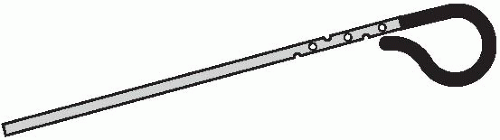 FIGURE 3-2. A straight pigtail catheter (Omniflush) is used to perform abdominal and pelvic aortograms. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree