A. Urgent aortic valvuloplasty
B. Initiation of IV milrinone
C. Pericardiocentesis
D. Urgent atrial balloon septostomy
E. Initiation of ECMO
15. In which of the following patients can an MRI be safely utilized to assess RV function?
A. 40 y/o status post placement of a permanent pacemaker lead without a generator
B. 18 y/o status post AICD placement for long QT syndrome
C. 19 y/o 1 week status post covered stent placement for coarctation of the aorta
D. 25 y/o status post repair of tetralogy of Fallot and status post DDD pacemaker placement
E. 26 y/o status post placement of a 36 mm Amplatzer septal occluder
16. A 1-week-old patient is referred to you for a murmur. On ECG, they have evidence of left axis deviation. Which of the following is the most likely diagnostic cause of the left axis deviation?
A. Complete AV canal defect
B. Total anomalous pulmonary venous connection
C. Concentric LVH
D. Secundum atrial septal defect
E. Double-outlet right ventricle (DORV)
17. A 15-year-old female presents to the clinic complaining of a rapid heart rate, which she has noticed for the past month. She denies any chest pain, syncope, or pre-syncope. Heart rate is 110/min while sitting on the examination table. Blood pressure is 110/70 mm Hg. BMI is 16. A faint systolic ejection murmur is heard. Of the following, which would be the most appropriate laboratory test to order?
A. Electrolyte panel
B. Thyroid-stimulating hormone (TSH)
C. Chromosome panel (karyotype)
D. Hemoglobin A1C
E. Serum cortisol
18. A 9-year-old daughter of migrant workers is brought to the emergency department with new-onset pain in her knees and wrists. Her knees are swollen and red and are tender to the touch. You also note several erythematous, serpiginous, macular lesions with pale centers on her trunk that are not pruritic. She is febrile (temp = 39.5°C), and is found to have an elevated serum streptococcal antibody titer. Of the following, which is the most likely diagnosis?
A. Juvenile rheumatoid arthritis
B. RF
C. Systemic lupus erythematosus (SLE)
D. Juvenile dermatomyositis
E. Kawasaki’s disease
19. An 18-year-old female is referred to you for hypertension. Basic laboratory studies are normal, and an abdominal ultrasound with renal Doppler is normal. An echocardiogram is performed and thought to be normal, but images are difficult secondary to patient size. The chest x-ray in Figure 3.2. is taken.
Which of the following is the next best diagnostic test to order?

A. Left and right heart catheterization
B. Stress echocardiogram
C. Exercise treadmill test using the Bruce protocol
D. Urine metanephrines
E. Computed tomography scan of the chest
20. A 38-week-old term infant with CHD is diagnosed with necrotizing enterocolitis (NEC). Which of the following diagnoses is associated with the highest risk of developing NEC in a term neonate?
A. Tetralogy of Fallot
B. Patent ductus arteriosus
C. Truncus arteriosus
D. Tricuspid atresia
E. Complete AV canal
21. A 3-month-old female infant is brought to the emergency department with tachypnea. Her parents report that she has a history of tiring with feeding, which has been getting progressively worse in the last month. A chest x-ray is obtained and shows marked cardiomegaly. On examination, you hear a 2/6 holosystolic murmur at the apex and axilla. Electrocardiography demonstrates prominent Q-waves in the lateral leads. Which of the following is the most likely diagnosis?
A. ALCAPA
B. Ventricular septal defect
C. Complete AV canal
D. Tetralogy of Fallot
E. Pulmonary hypertension
22. A 5-year-old male presents to the emergency department following a motor vehicle accident. The attending physician notes that his blood pressure is now 70/40 and that his heart sounds are distant. Which of the following physical exam findings would be consistent with traumatic cardiac tamponade?
A. A third heart sound
B. Neck vein distention
C. A precordial rub
D. A precordial knock
E. Bradycardia
23. You are seeing a 12-year-old girl in clinic, who was referred to you for cardiomegaly. On examination, you hear distant breath sounds as well as pulsus paradoxus. Her heart rate is 65. She has complained of progressively worsening fatigue over the last 2 months, which she attributes to her recent 20-lb weight gain. Which of the following is the most likely cause of her pericardial effusion?
A. RF
B. Recent isoniazid administration
C. Renal failure
D. Hypothyroidism
E. Purulent pericarditis
24. Which cardiac defect(s) are most commonly associated with congenital rubella infection?
A. Coarctation of the aorta and tetralogy of Fallot
B. Transposition of the great arteries and atrial septal defect
C. Tetralogy of Fallot only
D. Pulmonary stenosis and PDA
E. Ectopia cordis
25. A 7-year-old boy presents to your office with exercise intolerance. You note a 3/6 systolic ejection murmur at the left upper sternal border with a widely fixed split S2 and a soft mid-diastolic rumble. Which of the following would you most likely find on further investigation?
A. Evidence of LVH on ECG
B. Qp:Qs = 1.5
C. Accessory left anterior descending coronary artery
D. Peaked P waves on ECG
E. Spontaneous closure of the defect by age 10
26. A 1-year-old female presents with fever and shock. An echocardiogram reveals a large pericardial effusion; you suspect that the patient has bacterial pericarditis. Which of the following is the most likely organism that will be isolated from pericardial fluid?
A.Haemophilus influenzae
B.Streptococcus pneumoniae
C.Neisseria meningitidis
D.Staphylococcus aureus
E.Escherichia coli
27. You are seeing a neonate in the ICU who presented with cyanosis. The sonographer has indicated the diagnosis of an aortopulmonary (AP) window with intact ventricular septum and suspects that there is also an interrupted aortic arch. Which type of interrupted arch is most likely for this patient?
A. Type A (interruption distal to the left subclavian artery)
B. Type B (interruption between the left carotid and left subclavian arteries)
C. Type C (interruption between the carotid arteries)
D. Type D (interruption proximal to the innominate artery)
E. All types occur with equal frequency
28. A 15-year-old female is found to have separate origins of the left anterior descending and left circumflex arteries within the left aortic sinus of Valsalva. Which of the following is true regarding this finding?
A. The patient should be restricted from all athletic activities
B. It is found more commonly in patients with benign syncope
C. It is a known risk factor for sudden death
D. It is more frequent in patients with mitral valve prolapse
E. It does not appear to have any clinical significance
29. A 30-year-old female with history of tricuspid atresia status post complete Fontan (nonfenestrated) at age 5 years presents with a 2-year history of dyspnea on exertion and cyanosis that is worse when in the standing position. What is the most likely cause of her symptoms?
A. Hepatic arteriovenous malformation (AVM)
B. Vein of Galen malformation
C. Lower extremity AVM
D. Upper extremity AVM
E. Pulmonary AVM
30. A 25-year-old male presents to your clinic with exertional cyanosis. He has a history of heart block following Mustard palliation of d-TGA and required intravenous pacemaker lead placement. He had an echocardiogram which revealed a small SVC baffle leak with bidirectional shunting. Which of the following is the most appropriate treatment for this patient?
A. Balloon dilation of baffle leak
B. Closure of baffle leak using a device
C. Stent placement in the SVC baffle
D. Stent placement in the IVC baffle
E. Surgical MAZE procedure
31. You are seeing an 8-year-old female, who had an episode of fainting the previous week while running in gym class. Her mother reports that she was having URI symptoms including fever at the time, but that these have now resolved. You obtain an ECG (Fig. 3.3).
Which of the following is the most likely diagnosis?
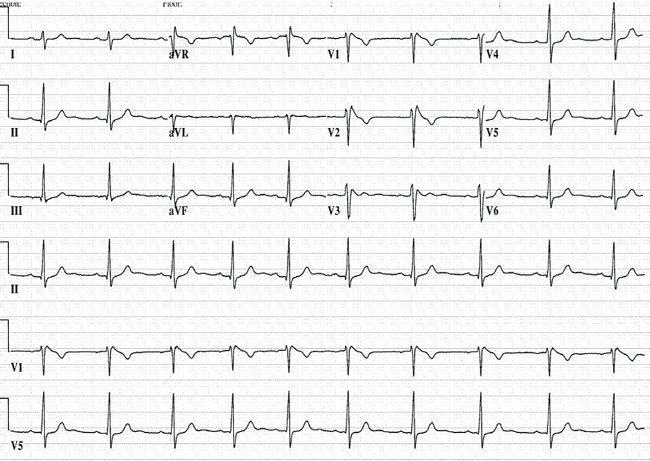
A. Long QT syndrome
B. Brugada syndrome
C. Vasovagal syncope
D. Wolff–Parkinson–White (WPW) syndrome
E. Hypertrophic cardiomyopathy
32. A murmur is heard at a 1-week well child examination. The infant is referred for an echocardiogram, which reveals a well-circumscribed mass in the wall of the left ventricle. What is the most likely diagnosis?
A. Fibroma
B. Myxoma
C. Rhabdomyoma
D. Blood cyst
E. Hemangioma
33. You see a 5-year-old male with aortic stenosis in follow-up. You note that he has a single S2 heart sound. Which of the following is characteristic of the S2 heart sound in patients with aortic stenosis?
A. The S2 becomes more widely split with inspiration in severe AS
B. The S2 has normal physiologic splitting in patients with mild AS
C. Paradoxical splitting of S2 often occurs with mild AS
D. The pulmonic component of S2 is often decreased with severe AS
E. The S2 is single in mild AS
34. A 14-year-old male patient is referred to you for a murmur. On history, the patient reports recurrent low-grade fevers, malaise, and a 20-lb weight loss in the last 2 months. On his echocardiogram, you find a pedunculated mass (2 cm × 2 cm) attached to the fossa ovalis in the left atrium. What is the most likely diagnosis?
A. Rhabdomyoma
B. Teratoma
C. Fibroma
D. IVC extension of Wilms tumor
E. Myxoma
35. A 12-year-old patient with a history of aortic stenosis, status post Ross procedure at the age of 2, presents with chest pain after exercise. Chest radiography is normal. Echocardiography reveals possible wall motion abnormalities in the left ventricle. In addition to other studies, further cardiac imaging studies are planned. Which of the following techniques will be most useful in this patient?
A. Cardiac MR with bright-blood imaging
B. Cardiac MR with dark-blood imaging
C. Cardiac MR with delayed gadolinium imaging
D. Multidetector CT with 3D reconstruction
E. Strain imaging
36. A 14-year-old male patient is referred to you for a murmur. On examination, you note that he has significant scoliosis, pectus carinatum, and pes planus (flat feet). His height is 190 cm, and his arm span is 210 cm. His aortic sinus of Valsalva measures 45 mm in diameter. His carotid arteries, aortic arch, and descending aorta are normal. There is no significant family history. He admits of being admitted twice in the past with spontaneous pneumothoraces. Which of the following is true regarding this young man’s diagnosis?
A. He likely has Loeys–Dietz syndrome
B. He satisfies the Ghent criteria for Marfan syndrome
C. He should have a repeat echocardiogram in 5 years
D. He does not need an eye examination
E. He needs an ECG to assess for a prolonged QT interval
37. A 12-year-old male with CHD is noted to have complete AV block. Which of the following is the most likely cardiac diagnosis for this patient?
A. Atrial septal defect
B. D-transposition of the great arteries
C. Polysplenia
D. Asplenia with Tetralogy of Fallot
E. Maternal lupus
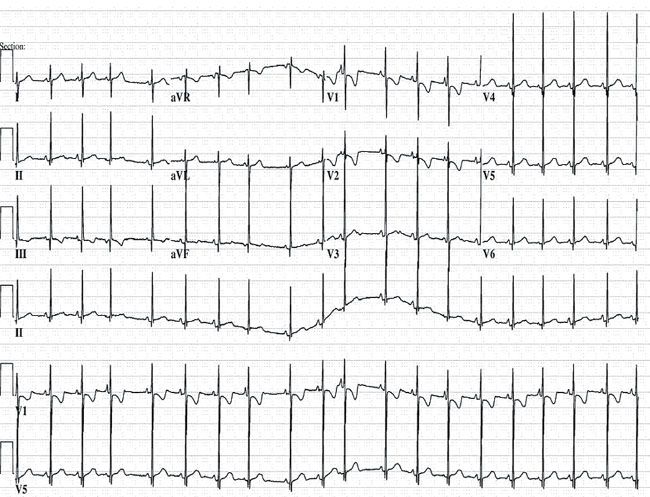
38. An echocardiogram performed on a neonate reveals severe tricuspid valve dysplasia with prolapse and severe mitral valve prolapse (Figure 3.4.). He is ultimately diagnosed with congenital polyvalvular dysplasia. Which of the following is the most likely genetic diagnosis in this patient?

A. Trisomy 18
B. Down syndrome
C. Noonan syndrome
D. DiGeorge syndrome
E. Alagille syndrome
39. Which of the following genetic syndromes are associated with an increased incidence of partial anomalous pulmonary venous return?
A. Trisomy 18 and Trisomy 21
B. Turner and Noonan
C. Holt–Oram and Marfan
D. Turner and Trisomy 21
E. Noonan and Alagille
40. A 5-year-old male is diagnosed with WPW syndrome. He is found to have an abnormal echocardiogram. Which of the following forms of CHD is most commonly associated with WPW?
A. Ventricular septal defect
B. Bicuspid aortic valve
C. Tetralogy of Fallot
D. Ebstein’s anomaly
E. Atrial septal defect
41. You have been following a 2-year-old male with pulmonary stenosis. Which of the following would be a clinical clue that the degree of stenosis has worsened?
A. The murmur peaks earlier
B. The ejection click occurs later
C. The split of S2 becomes wider
D. The “a” wave becomes less prominent
E. S1 becomes more prominent
42. A 13-year-old girl presents to you for the evaluation of a murmur. The patient is asymptomatic, but does not participate in athletic activity. Her family history is significant for a paternal uncle, grandfather, and great grandfather who had “thick heart muscle.” On examination, she has short stature, a triangular face, pectus excavatum, and a webbed neck. Her heart examination reveals an RV lift and a soft short systolic ejection murmur at the LUSB. What are you most likely to find on her echocardiogram?
A. Bicuspid aortic valve with or without coarctation
B. Discrete supravalvular pulmonary stenosis
C. Thickened pulmonary valve with mild stenosis
D. Bilateral pulmonary branch stenosis
E. Right aortic arch
43. A 16-year-old male is referred to your clinic. He has a history of recurrent sinusitis for which he has undergone numerous courses of antibiotics. A chest x-ray is performed that shows evidence of dextrocardia. In addition, the stomach bubble is located on the right side of the abdomen. A CT scan of the chest reveals bronchiectasis. Which of the following is the most likely diagnosis?
A. Carney complex
B. DiGeorge syndrome
C. Wiskott–Aldrich syndrome
D. Turner syndrome
E. Kartagener syndrome
44. You are referred a 5-day-old female infant due to an irregular heart rhythm. There is no significant family history for arrhythmias, sudden death, or CHD. She has an ECG performed prior to seeing you (Fig. 3.5).
Which of the following is the next best course of action?
A. Start the patient on propranolol
B. Urgent cardiac surgical referral
C. Administer a dose of IV adenosine
D. Reassure the parents
E. Check a TSH level
45. You are consulting on a 17-year-old female in the hospital with a concern for dyspnea on exertion. On examination, she is comfortable. Her S1 and S2 sounds are normal, but there is a harsh 3/6 systolic murmur with a musical quality heard from the sternal border down to the apex. There are no clicks, thrills, or rubs, and diastole is quiet. Just after a PVC that you note on her cardiac monitor, the murmur increases in intensity.
What is the most likely cause of the murmur?
A. Ventricular septal defect
B. Mitral regurgitation
C. Pulmonary stenosis
D. Aortic stenosis
E. Innocent murmur
46.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


