Coronary bifurcation lesions remain challenging even in the era of drug-eluting stents, for technical reasons and for determining the best approach to optimize long-term outcomes. The preferred strategy has evolved to be “provisional” side branch intervention, on the basis of multiple randomized trials. A strategy of routine single-stent implantation of the major branch with provisional side branch stenting was found to be at least as good as, and, in some studies superior, to a mandated 2-stent strategy. These results were found despite a more satisfactory immediate angiographic result with the 2-stent strategy.
At present, what are the requirements to implant a second stent with the provisional strategy, particularly for improving long-term outcomes? Although various angiographic or flow criteria are used empirically in decision making for side branch interventions, none has been validated. Studies using fractional flow reserve (FFR) have demonstrated that angiographic assessment alone may be deceptive. In fact, studies have shown that most side branches with “significant” stenosis (>50% diameter stenosis) have FFR in the normal range. Because studies using FFR have shown that such lesions do not require intervention, the use of angiography alone may overestimate the need to intervene on the side branch, and hence support the “oculostenotic reflex” response from the interventionist.
How then should decision making on side branch stenosis after stenting be determined? FFR is an easily obtainable physiologic parameter that is stenosis specific and reflects the degree of flow limitation in the myocardium supplied by the specific artery. As such, it is an ideal stand-alone tool to determine the presence of a lesion producing ischemia and possibly requiring intervention, although a specific study related to side branch treatment with long-term outcomes has not yet been performed.
In this issue of The American Journal of Cardiology , Kang et al consider a different strategy. Specifically, they asked if there are preintervention angiographic and intravascular ultrasound parameters that will predict side branch compromise after main branch stenting. They used FFR as the “gold standard” for the detection of ischemia to define side branch compromise. They concluded that preintervention intravascular ultrasound minimal luminal area (MLA) of the side branch ostium, MLA of the main branch distal to the carina, the amount of plaque burden at the side branch ostium, and the maximal balloon pressure are not reliable independent predictors of ischemia in the side branch after main branch stenting. No angiographic parameter correlated with side branch compromise after stenting. This study showed that a preintervention MLA of 2.4 mm 2 at the side branch ostium had approximately 50% chance of developing postintervention ischemia using an FFR value of <0.8. Stated another way, there was an equal chance of having side branch ischemia or not using this MLA, a problematic finding for clinical decision making.
Key take-away messages from the study by Kang et al are the following: (1) The incidence of ischemia when FFR <0.80 is used is low (18%) in side branches jailed with the single-stent technique. Were the more more rigorous FFR cutoff of 0.75 utilized, the incidence of ischemia was even less frequent (9%) in their study. (2) Truly stenotic ostial lesions with MLA <2.4 mm 2 appear to be a reasonable cut point in determining ischemia-producing ostial side branch stenosis, but the value is not specific with half of patients in this group do not exhibit ischemia by FFR.
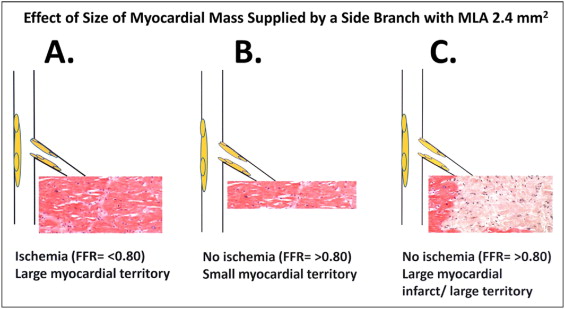
The relatively poor specificity of the MLA threshold may be explained in part by the extent of myocardium supplied by the side branch. It should be emphasized that the probability of ischemia with a reduced side branch luminal size is directly proportional to the amount of viable myocardium supplied by the side branch, as shown in Figure 1 . Thus, the use of a fixed MLA to predict ischemia is ultimately compromised itself by this crucial parameter.