Fig. 34.1
OR-adjacent Induction Room: Layout illustrating OR-adjacent induction rooms (often referred to as “anaesthesia rooms” (Used with permission from Stantec Architecture, Inc. ©2013 Stantec)
In contrast, in-room induction – common throughout much of North America and Scandinavia – is designed for serial processing in which the patient is anesthetized in the operating room, after (rather than while) the operating room is being set-up. Compared to OR-adjacent induction, in-room induction generally requires less overall space because dedicated induction rooms are not needed, but case turn-over time is potentially increased because induction cannot take place concurrently while the operating room is being set up. Some facilities designed for in-room induction for adult surgery, however, are designed for OR-adjacent induction for pediatric surgery.
What remains unclear is the impact of an induction room model on the whole surgical process, its phases and delays between the phases, and the number of cases performed. Torkki et al., found that the mean non-operative time was reduced by 45.6 %, whereas the surgery time remained unchanged [13]. The time savings contributed to the concurrent anesthesia induction and the cut down in delays between the phases. The new model allowed one additional case to be performed during a 7-h working day. The daily raw utilization of the surgical procedure room increased by 8.9 %.
The decision to choose one of the parallel workflow models that could be economically favorable will depend on several physical and organizational variables, such as:
The cost of the additional space and equipment required to allow the parallel processing to occur;
The utilization of the procedure room and induction room;
The cost of each additional person, whether it be physician, nurse, or technician; and,
The duration of cases: short procedures benefit the most from individual induction rooms.
In contrast, if a surgery suite has longer cases with fewer turnovers, a single centralized induction room serving several multiple procedure rooms may be the way to go.
The revenues gained by parallel processing would need to offset any increased costs of personnel and loss of revenue producing procedure room spaces. Success for such parallel processes may be best achievable with a select patient population and a limited number of types of cases.
Intra-room Workflow
In contrast to intra-departmental workflow which is influenced by traffic to and from the operating room, intra-room workflow considers various types of flow possibilities and limitations within the operating room. Variations to the built environment that most greatly influence intra-room work flow include the number and location of doors into the operating room, how the flow of clean and soiled goods are (or are not) separated as they enter and exit the space, how the surgical table is placed within the room, and the position and configuration of medical and information technology (IT) devices. Related, Lynch et al have showed that the number of OR door openings increases in direct proportion to case length, compromising the sterile environment of the operating room and increasing risk of mediastinal infections [14]. Young and O’Regan demonstrated that in 46 cases analyzed, there were 4,273 door openings recorded. The mean frequency of door openings per case was 92.9 (45–205), with 19.2 (6.4–38.2) openings per hour. The theatre door was open for 10.7 % of each hour of operating. Door opening disturbs theatre airflow and results in increased air and wound contamination and may be a contributor to surgical mistakes [15].
Functional zones within the operating room should be clearly delineated and the design team must understand the various processes (such as room set-up, patient transport, pre-operative preparation, surgical procedures, post-operative activities, room turn-over, and so forth) as well as the numerous personnel types (such as surgeons, nurses, anesthesiologists, perfusionists, imaging technologists, students fellow, residents, and so forth) that participate in the many procedures that the room will accommodate. In general, a room that has clear separation and delineation of sterile, circulating and anesthesia zones within the operating room (Fig. 34.2) should yield efficient and effective intra-room work flow and accommodate a greater variety of procedure types. Specifically, consideration should be given to the ease of transporting the patient into the room and loading them onto the surgical table without intruding into the sterile or anesthesia zones; ease of bringing clean and sterile supplies into the room and placing them where they are needed without disrupting other activities; and, the ease of emergency access and egress during critical events.
Fig. 34.2
Operating Room Zoning Diagram: Diagram illustrating the various functional zones within a typical operating room (OR) (Used with permission from Stantec Architecture, Inc. ©2013 Stantec)
While numerous studies have examined causes of surgical errors, few focus on causation related to the built environment. One pilot study conducted at the Medical University of South Carolina [16] examines how the design of a cardiothoracic operating room can influence flow disruptions. While studying disruptions related to communications, environmental hazards, equipment failures, general interruptions, room layout and usability across pre-operative, peri-operative and post-operative phases, the most frequent flow disruptions were related to room layout. These occurred most often in the peri-operative phase and least often in the post-operative phase. Room design recommendations for the specific operating room that was studied include, “expand the anesthesia work space at the head of the table, expand space for perfusion between table and wall and/or eliminate travel through area, swing entry doors out and/or relocate closer to the footwall of the room”.
While these recommendations apply to the particular design features of the specific room studied, one can apply general considerations of overall room size and configuration, size and configuration of internal room zoning, door placement and direction of swing, and placement and movement of equipment and devices to the design of most operating rooms. Careful consideration should be given to the placement of patient entry doors so that patient transport does not conflict with anesthesia and sterile set-up. Similarly, circulating traffic should enable supplies to be brought directly to their primary places of use without passing through unrelated zones. Where possible, door leaves should not swing directly into areas of congestion or where disruption is most detrimental. The use of bypass or sliding doors in jurisdictions where they are permitted may further reduce spatial conflicts and collisions.
Another suggested design feature is to orient nurse charting stations so the person doing the charting faces the area where the surgery is being conducted rather than facing the opposite wall. The charting station, however, should not adversely protrude into the room or circulation zones and corners of the workstation should be rounded.
Design for proper intra-room work flow can become increasingly complex for hybrid operating rooms or other surgical rooms where the often opposing requirements of both surgical and imaging equipment and personnel must be considered. Design considerations for hybrid operating rooms are discussed later in this chapter.
Work Flow Typologies
Design strategies for separating clean and soiled goods influence both intra-room work flow and intra-department work flow. Three key surgical suite typologies are common (Fig. 34.3). A “clean core” layout places several operating rooms around a common clean core, from which clean and wrapped sterile goods flow “one way” into a dedicated “clean” side of each operating room and exit through a dedicated “soiled” side of the room. A clean core often includes dedicated clean and soiled lifts connecting the core to a central sterile supply area on a different floor but directly above or below the core, enabling a dedicated vertical connection via the lifts. A clean core layout often requires more space than the other typologies.
Fig. 34.3
Surgical Suite Typologies: Three surgical suite layout typologies: (a) clean core; (b) dedicated clean and soiled corridors and (c) combined clean and soiled corridor; (Used with permission from Stantec Architecture, Inc. ©2013 Stantec)
Dedicated “clean and soiled corridors” layouts provide similar flow of soiled and clean goods as does the clean core layout, but does not store the clean supplies in a dedicated core. Instead they typically travel in case carts from a nearby satellite clean supply storage area or to and from the primary central sterile supply area. This type of layout usually requires less overall space than a clean core layout.
A combined “clean and soiled corridor” layout relies on covered case carts to separate clean and soiled goods as both types of material share the same corridor. Of the three typologies, the combined corridor layout typically requires the least amount of space, but requires a well-managed transport system to maintain appropriate infection control. This also requires more oversight to ensure effective infection control.
Standardization
Adopting standardized processes from non-healthcare industries, such as aerospace and manufacturing has long been applied to healthcare in an effort to improve safety and communications [17]. A well-known example is incorporating aeronautical flight-ready checklists into operating room protocol to reduce the risk of wrong-patient and wrong site procedures as well as to invoke other safe practices.
Standardization can also be applied to room design. For example, standardized inpatient nursing units – with ‘handed’ instead of ‘mirrored’ patient rooms – have been designed and built for decades. A handed nursing unit configures all patient rooms identically, for example all with the entrance door on the right side and the headwall on the left side of the room. In contrast, a mirrored layout configures each pair of rooms identically, but the rooms within each room pair are mirror opposites of each other, often sharing a common plumbing wall between the pair. The assumed benefit of same-handed rooms is that staff will intuitively know exactly where essential supplies are at critical times and all process will be standardized due to the unvarying built environment, thus improving safety by eliminating physical variation. While this logic may appear to be sound, definitive evidence of the overall benefit of room standardization, and in particular its impact on perioperative room design remains elusive.
Similarly, standardized “handed” operating rooms are based on the logic that standardized work process and consistent placement of critical supplies and devices improve work flow and safety. Historically, surgical suites have been configured with pairs of mirrored operating rooms symmetrical around a shared sub-sterile room in much the way that mirrored inpatient rooms are placed symmetrically around a shared plumbing wall. New approaches to surgical infection control, including recommendations against routine use of flash sterilization [18] , have resulted in surgical suite layouts that either eliminate sub-sterile rooms or incorporate a satellite instrument processing station adjacent to a shared clean core. Such layouts easily accommodate all operating rooms to be handed rather than mirrored (Fig. 34.4).
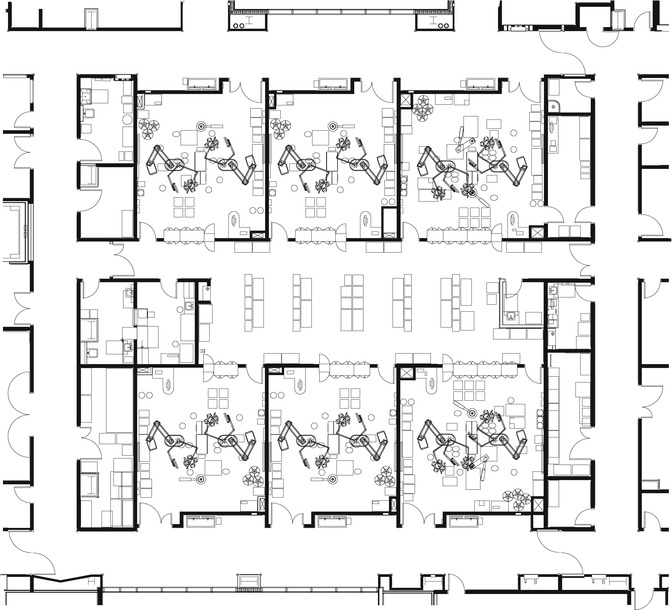
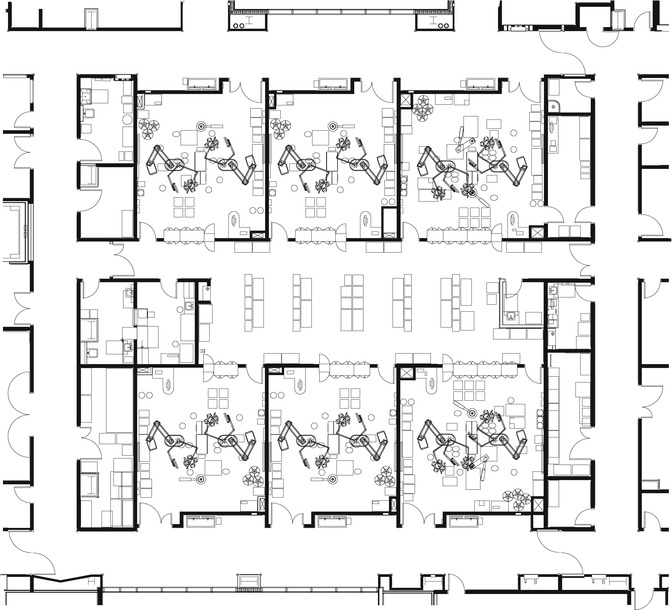
Fig. 34.4
Clean Core Surgical Suite: Six operating rooms organized around a central clean supply core. Architect of Record: Co Architects; Associate Architect: Stantec. (Used with permission from Palomar Pomerado Health. ©2013 PPH)
Air Flow
Hospital operating rooms are among the most infection-sensitive environments in health care facilities. Surgical procedures increase patient vulnerability to pathogens transmitted from surgical personnel, surgical equipment, the air and a patient’s own skin flora. Air flow is one of the most important aspects of the built surgical environment with regard to infection control, human comfort and clinical outcomes. Surgical site infections account for roughly 15 % of all nosocomial infections among hospitalized patients [19] and of those, 80–90 % of surgical wound bacterial contamination comes from the ambient air. In the United States alone, approximately 700,000 patients a year are affected by surgical site infections [20]. Recent evidence shows that IV poles, anesthesia workstations and OR personnel are teeming with antimicrobial bugs and serve as a significant source of patient environmental contamination in the operating room [21].
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


