Fig. 18.1
Site of election for valve repair. Valve B in FV below profunda takeoff is preferred. Valve A at CFV is very prominent and tempting. Repair of this would still permit reflux of blood entering FV from profunda
In the popliteal vein valve is located at adductor tubercle level or at mid/distal segment [3]. Preoperative descending venogram and duplex scan can help in localizing the valves precisely.
Reflux in the deep veins is confirmed by the intraoperative strip test. The valve apparatus is located first and the infravalvular portion is controlled with a bulldog to prevent inflow. This segment is milked up through the valve to empty all blood. If the valve is competent, the infravalvular portion of the vein will remain collapsed; if it is incompetent, this segment will fill from above. To augment the reflux, the supravalvular portion can also be gently squeezed toward the valve [3, 4].
Techniques of Valve Repair
Several techniques of valve repair are available. The choice depends basically on the pathological process involved. The expertise and preference of the operating surgeon are the other factors that govern the choice of the procedure. The commonly practiced procedures are:
Internal valvuloplasty
External valvuloplasty
Axillary vein transfer
Segment transposition
Internal Valvuloplasty
The technique is suitable for patients with PVI. It is not feasible for the post-thrombotic group. The valve in the femoral vein just below profunda takeoff is the preferred site for internal valvuloplasty. The technique involves exposure and control of CFV, FV, and profunda in the groin. Venotomy of the femoral vein at the appropriate position is performed after vascular control and intraoperative heparinization. Repair of the elongated valve leaflets are done under direct visualization. The redundant cusps are plicated with 7–0 polypropylene sutures to reduce the redundancy by 20 % and to ensure proper coaptation of the cusps. The knots are tied on the external aspect at the level of commissure. Loupe magnification (×2) and frequent saline irrigation are used to define the cusps. Venotomy is closed with meticulous care and competence is checked again (Fig. 18.2).
Fig. 18.2
Internal valvuloplasty. (a) Valve cusp before repair. Long floppy and incompetent. (b) Post repair cusp shortened and competent
Several types of venotomies have been described: Kistner has described longitudinal venotomy starting 10–15 mm caudal to valve attachment line and extending up through the commissural apex [7]. Raju recommends transverse venotomy 5 mm above the commissural apex [8]. Sottiurai introduced T incision, a supravalvular transverse incision with distal extension into valve sinus [9]. Tripathi introduced trapdoor venotomy, two transverse incisions connected by a vertical limb, for optimum exposure [10].
The advantages of internal valvuloplasty are that it offers an anatomically precise repair since it is carried out under direct vision and the results are more lasting. The disadvantages of the techniques are that it is time consuming, is not feasible for multiple site repairs, and needs postoperative anticoagulation. The technique is unsuitable for damaged and deformed cusps of the post-thrombotic limb.
External Valvuloplasty
This technique was also introduced by Robert Kistner. It does not require a venotomy and is suitable only for PVI. In this procedure, the valves are repaired by placing sutures transmurally. Widening of the angle between the cusps is considered to be the reason for incompetence. When the angle is narrowed, the valve sinus becomes deepened and prevents reflux. A series of interrupted or continuous sutures placed both at the anterior and posterior valve attachment lines to cover about 20 % of the line. This is sufficient to restore competence. If more narrowing is needed, it is better to abandon the procedure in favor of axillary vein transfer [3] (Fig. 18.3).
Fig. 18.3
External valvuloplasty. (a) Before repair. Note the wie angle between the cusps. (b) Post repair. Angle narrowed
Advantages of external valvuloplasty are many. It avoids venotomy and hence postoperative anticoagulation is not needed. The technique needs less time compared to the internal technique. Multiple site repairs can be undertaken: femoral and profunda vein at the groin and the popliteal/posterior tibial vein at the knee level. This is known as triple external valvuloplasty. The major disadvantage is that it is unsuitable for the post-thrombotic pathology.
Modifications of External Valvuloplasty
External banding technique is suitable when venospasm during surgery restores competence. These are cases where the incompetence results from vein wall dilatation. There are two methods.
1.
Prosthetic sleeve. An external wrap using a Dacron/Teflon graft is wrapped around the vein at the level of the valve with tightness sufficient to restore competence. This acts as a restraint to prevent undue dilatation of the vein wall around the valve. The graft is anchored to the adventitia to prevent migration [4]. This method is employed to prevent late dilatation after any technique of valvuloplasty [4] (Fig. 18.4).
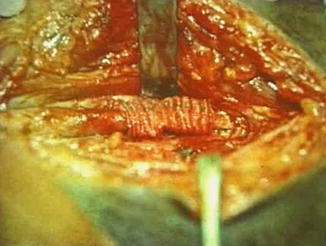
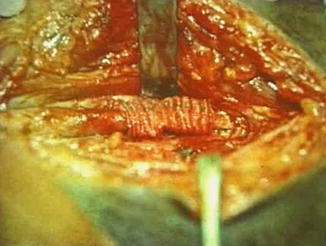
Fig. 18.4
External wraparound with Dacron sleeve
Angioscopic repair is a modification of the external valvuloplasty. The valve apparatus is visualized through an angioscope passed through a small venotomy above valve station or through a side branch of GSV. The repair is done under vision. The sutures are placed transluminally instead of transmurally, at the level of valve attachment lines to tighten them. The venotomy is closed after repair. The technique was pioneered by Gloviczki and his colleagues from the Mayo clinic [13].
Transcommissural valvuloplasty was pioneered by Raju. Transluminal sutures are placed as in the previous case but “blindly” without the aid of angioscope. Initial suture starts at the commissural angle and is shallow. Each subsequent suture should be placed slightly deeper into the lumen than the previous one and tied. According to Raju, although this is a blind technique, valve competency can be routinely achieved [14].
Limited anterior plication. Circumferential dissection of the vein is reported to increase late post-repair dilatation. The technique of limited anterior plication was introduced to prevent late dilatation. Both transmural and transluminal sutures with the use of angioscope have been described. The procedure involves dissection of femoral vein over anterior aspect only. Running mattress sutures are placed only at the anterior commissure. The sutures start from a point 3 to 4 mm proximal to angle of valve cusp and extend up to the angle. Combined with high ligation and stripping, this method is reported to provide good long term results [4].
Vein Valve Transplantation (Axillary Vein Transfer)
This technique was first introduced by Taheri and his group in 1982. The procedure is useful in post-thrombotic pathology. The axillary vein is exposed by a transverse incision along the skin crease in the axilla. Two to three cm of axillary/brachial vein bearing a competent valve is harvested. The axillary vein would be a suitable size match for the femoral vein. Ligation of the cut ends of the donor vein does not produce any ill effects [3]. The recipient vein can be either the femoral vein in the groin, just below the takeoff of the profunda or the popliteal vein. The latter site is the “gateway” to control all the proximal reflux. A full prone position is preferred to expose the popliteal vein.
After heparinization, the recipient vein is divided at the appropriate level. The proximal anastomosis is completed first. Interrupted sutures are preferred since continuous sutures can produce luminal narrowing. Valve competence is confirmed by releasing the clamp after proximal anastomosis. Forty percent of the axillary valves may be incompetent [4]. This can be repaired by transcommissural valvuloplasty. The distal anastomosis is completed without reapplying the clamp. This is to allow full distention of the donor segment. The distal end of the recipient vein can be trimmed to achieve optimum tension. Torsion and tension are to be strictly avoided. A Dacron sleeve wraparound helps to prevent late dilatation. In post-thrombotic veins, intraluminal synechiae in the recipient femoral vein could be excised to create a suitable lumen for anastomosis [3] (Fig. 18.5).
Fig. 18.5




Axillary segment transfer. (a) Axillary vein with competent valve being harvested. (b) Incompetent FV. (c) Segment of FV excised. (d) Replaced by axillary vein segment with competent valve. (e) Operating photograph axillary vein segment transferred (yellow arrow) to PV
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


