Debulking Approaches Prior to Stenting in Interventional Cardiology
Samin K. Sharma
Ramanjit S. Bagga
Annapoorna S. Kini
Intracoronary stenting (ICS) has become the primary interventional strategy for patients undergoing percutaneous coronary intervention (PCI), particularly in the era of drug-eluting stents (DES). Randomized trials, in the lesions studied, have shown a very low incidence of angiographic restenosis and target lesion revascularization (TLR) (1,2). With increased operator experience and improved technology, growth has been constant in the number of complex lesions (i.e., calcified lesions, nondilatable rigid lesions, ostial lesions, bifurcations, and chronic total occlusions) attempted by interventionalists with the use of DES, despite a lack of compelling data proving effectiveness for some of these. Procedural complexity, in-hospital complications, and long-term recurrence remain major concerns of DES in these complex lesions because of the large and/or resistant plaque burden that might lead to stent underexpansion and increase the chances of stent thrombosis and restenosis. Stent deployment sometimes is difficult in complex calcified lesions and is prone to problems such as stent entrapment, stent striping, underexpansion, and balloon rupture, with the attendant risks of major coronary dissection and acute in-hospital complications. Optimal stent expansion and final minimal lumen diameter remain important predictors of restenosis even after DES implantation (3). Uniform, rather than nonuniform stent expansion, will guarantee homogenous drug delivery and diffusion into the lesion after DES by maintaining the adequate distance between stent struts. The pretreatment of these complex lesions with high-pressure noncompliant balloon inflation before DES is surely an option, but is not always successful and may be limited by plaque shift, very rigid plaque, dissection, and vessel perforation. Incomplete stent apposition has been reported to be a predictor for late stent thrombosis with DES. Postmortem histopathologic studies in human coronary arteries also have shown that high-pressure stent implantation, used to ensure adequate stent expansion, may cause arterial medial disruption (break in internal elastic lamina) or lipid core penetration by stent struts; this induces arterial inflammation that is associated with increased neointimal growth (Fig. 10.1) (5). In studies using intravascular ultrasound (IVUS), it has been suggested that neointimal area and late restenosis response were predicted by the degree of underlying plaque burden (plaque area) before PCI and the minimal lumen area achieved after PCI (6). In addition, Prati et al. demonstrated with IVUS analysis that late loss (degree of internal hyperplasia) has a direct correlation with the amount of residual plaque burden after stent implantation, suggesting that debulking before stenting might reduce restenosis (7).
Therefore, approaching complex lesions is challenging, and lesion preparation with plaque modification (debulking) techniques is suggested as an adjunct to stenting that will maintain the integrity of the DES delivery system and the polymer by causing uniform and optimal stent expansion. The routine use of IVUS, in addition to good visualization on angiography, is suggested in selecting the appropriate plaque modification strategy.
These plaque modification techniques can be classified into the following groups: (a) atherectomy devices, which
remove the plaque, such as directional coronary atherectomy (DCA) (Guidant Corp., Indianapolis, Indiana) or rotational atherectomy (RA) (Boston Scientific Corp., Natick, Massachusetts); (b) atherotomy devices, which cut (score) the plaque by low-pressure injury, such as the cutting balloon (CB) (Boston Scientific Corp., Natick, Massachusetts) and the FX miniRAIL Balloon (Guidant Corp., Indianapolis, Indiana); (c) laser angioplasty using excimer laser ablation (The Spectranetics Corporation, Colorado Springs, Colorado); and (d) other innovative, newer debulking devices.
remove the plaque, such as directional coronary atherectomy (DCA) (Guidant Corp., Indianapolis, Indiana) or rotational atherectomy (RA) (Boston Scientific Corp., Natick, Massachusetts); (b) atherotomy devices, which cut (score) the plaque by low-pressure injury, such as the cutting balloon (CB) (Boston Scientific Corp., Natick, Massachusetts) and the FX miniRAIL Balloon (Guidant Corp., Indianapolis, Indiana); (c) laser angioplasty using excimer laser ablation (The Spectranetics Corporation, Colorado Springs, Colorado); and (d) other innovative, newer debulking devices.
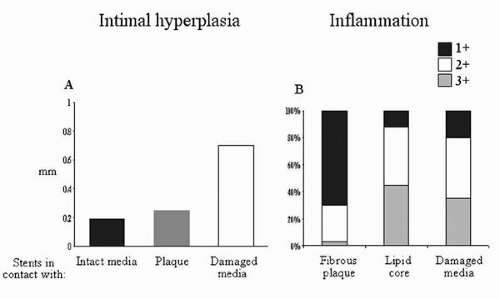 Figure 10.1. (A) Degree of intimal hyperplasia in relation to vessel wall contact with struts. (B) Degree of inflammation related to stent struts contacts. |
Unlike balloon angioplasty (BA) or stenting, which widen the coronary lumen by merely displacing atherosclerotic plaque, atherectomy or atherotomy techniques widen the lumen by actually removing tissue from the vessel wall or by scoring the plaque in a controlled manner. Each ablative device may be distinct in its mechanics of ablating the atheromatous plaque, but shares the common objective of debulking to optimize acute results, minimize intimal injury, facilitate stent delivery, reduce plaque shift, allow optimal and homogenous stent expansion, and reduce restenosis.
DIRECTIONAL CORONARY ATHERECTOMY
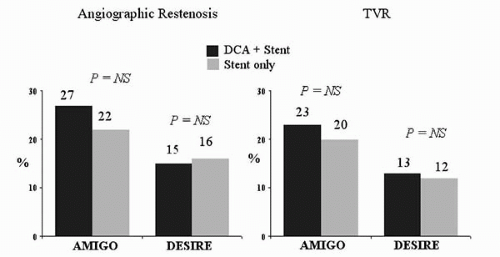
Directional coronary atherectomy (DCA) removes obstructive tissue by a catheter-based excision technique, utilizing a nose cone, a metal cutter and housing, and balloon inflation. This technique was first introduced in 1987, and was approved by the U.S. Food and Drug Administration (FDA) in 1990, following submission of a multicenter registry. DCA is effective in removing fibrotic, noncalcified plaque, particularly in aorto-ostial, branch ostial, bifurcation, and bulky eccentric lesions in proximal large vessels (size ≥3 mm). Stand-alone DCA has been shown to yield better acute and long-term angiographic results than plain BA when optimally performed; however, late restenosis still remains high, because DCA does not eliminate arterial remodeling and chronic recoil. Coronary stents reduce angiographic restenosis by inhibiting acute recoil and chronic arterial remodeling; therefore, the combined approach of debulking followed by stenting had been suggested to overcome the limitations of each device and improve clinical outcomes. Data from several registries suggest the feasibility, safety, and efficacy of performing DCA before stenting and demonstrate low restenosis rates and acceptable acute results in these complex coronary lesions (8, 9, 10, 11). The encouraging results seen in these registries led to two large, prospective, randomized clinical trials comparing DCA before stenting with stenting alone (Fig. 10.2): the Atherectomy before MULTI-LINK Improves Lumen Gain and Clinical Outcomes (AMIGO) trial and the Debulking and Stenting in Restenosis Elimination (DESIRE) trial. Long-term (8-month follow-up) results in the AMIGO trial that randomized 753 patients to either DCA followed by stenting or stenting alone showed no difference in angiographic or clinical restenosis between the two groups (12). The technique of debulking was operator dependent, and optimal debulking (defined as post-DCA diameter stenosis <25%) was achieved in only 26.5%, whereas suboptimal debulking was associated with a significantly higher restenosis rate (32%) compared with optimal debulking (16%). The cumulative major adverse cardiac events (MACE) rate at 30 days postprocedure was slightly higher in the DCA-treated patients. Similar observations also have been made in several IVUS-guided DCA and stenting studies. Therefore, the creation of a large lumen by debulking may be key for reducing the incidence of restenosis. The DESIRE trial randomized 500 patients to IVUS-guided DCA followed by stenting or stenting alone (13). Despite the achievement of a lower loss index at follow-up in the DCA + stent group (0.34 versus 0.41 mm), this trial also failed to show a clinical benefit at 6-month follow-up in this group.
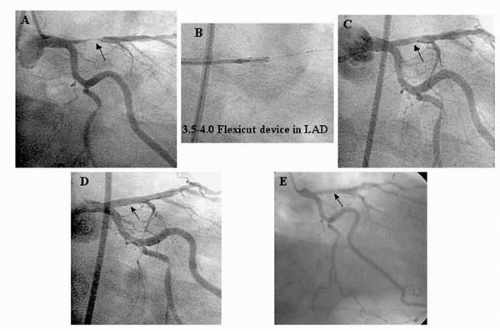
Therefore, based on the available data, DCA presently is limited to noncalcified ostial left anterior descending (LAD) arteries and large bifurcation lesions to provide acceptable acute results by reducing plaque shift and to improve late angiographic outcome in conjunction with stenting (Figs. 10.3 and 10.4). Despite the potential advantages, the use of DCA has been limited for a variety of reasons, including poor tracking in sharply angulated lesions, not feasible for calcified lesions, procedure time, the risk of perforation, and Dotter effect of the bulky device (8).
ROTATIONAL ATHERECTOMY
High-speed rotational atherectomy (RA) has been preferably
employed in the treatment of heavily calcified, ostial, and undilatable coronary artery lesions. With conventional stenting, such lesions usually are associated with lower success and higher complication rates owing to difficulties in stent delivery and expansion. High-pressure noncompliant balloon inflation for predilatation might occasionally succeed but is often insufficient to overcome vessel wall/plaque resistance and may result in acute recoil, arterial dissections, and perforation (14). The technique of RA relies on plaque ablation and pulverization by an abrasive diamond-coated burr rotating at about 150,000 to 160,000 rpm. Rotablation causes differential cutting and selective ablation of inelastic calcified stenosis, and it produces excellent acute procedural results with a relatively low complication rate. The abraded plaque is pulverized into micro particles, 5 to 10 μm in diameter, which are small enough to pass through the coronary microcirculation and ultimately undergo phagocytosis in the liver, spleen, and lung. Despite a high acute procedural success rate in ablating calcified plaque, RA is plagued with high restenosis when it is used as a stand-alone treatment, perhaps due to chronic arterial recoil and remodeling (15). It has been reported that successful RA of severely calcified or nondilatable coronary lesions facilitates stent delivery and expansion and reduces plaque shift, thereby decreasing side-branch closure (16). Several nonrandomized, retrospective studies showed improved procedural success rates and a trend toward lower restenosis in calcified lesions with the use of RA prior to ICS versus ICS alone (15, 16, 17, 18, 19). This led to two randomized trials that examined the effect of debulking with RA prior to ICS versus ICS alone. In the Effects of Debulking on Restenosis (EDRES) trial, 150 patients were randomized to ICS alone versus RA with ICS (20). Although acute gain was the same in both arms, a reduction was observed in 6-month binary angiographic restenosis in the RA + ICS arm. In the larger Stent Implantation Post Rotational Atherectomy (SPORT) trial (Fig. 10.5), 750 patients were randomized to receive either percutaneous transluminal coronary angioplasty (PTCA) or RA prior to ICS (21). The procedural success rate was better in the RA group; however, no differences were observed in angiographic or clinical endpoints between the two groups at 6 to 8 months follow-up. These results may be explained by operator bias in excluding severely calcified lesions for enrollment in the trial. A prospective, randomized trial comparing RA (or PCA) with PTCA before ICS in patients with chronic total occlusion has reported that the strategy of debulking before stenting yielded significantly lower angiographic restenosis rates at follow-up (22). Aggressive RA before ICS might yield superior long-term results, yet it is associated with a higher incidence of periprocedural myocardial infarction (MI) (23).
employed in the treatment of heavily calcified, ostial, and undilatable coronary artery lesions. With conventional stenting, such lesions usually are associated with lower success and higher complication rates owing to difficulties in stent delivery and expansion. High-pressure noncompliant balloon inflation for predilatation might occasionally succeed but is often insufficient to overcome vessel wall/plaque resistance and may result in acute recoil, arterial dissections, and perforation (14). The technique of RA relies on plaque ablation and pulverization by an abrasive diamond-coated burr rotating at about 150,000 to 160,000 rpm. Rotablation causes differential cutting and selective ablation of inelastic calcified stenosis, and it produces excellent acute procedural results with a relatively low complication rate. The abraded plaque is pulverized into micro particles, 5 to 10 μm in diameter, which are small enough to pass through the coronary microcirculation and ultimately undergo phagocytosis in the liver, spleen, and lung. Despite a high acute procedural success rate in ablating calcified plaque, RA is plagued with high restenosis when it is used as a stand-alone treatment, perhaps due to chronic arterial recoil and remodeling (15). It has been reported that successful RA of severely calcified or nondilatable coronary lesions facilitates stent delivery and expansion and reduces plaque shift, thereby decreasing side-branch closure (16). Several nonrandomized, retrospective studies showed improved procedural success rates and a trend toward lower restenosis in calcified lesions with the use of RA prior to ICS versus ICS alone (15, 16, 17, 18, 19). This led to two randomized trials that examined the effect of debulking with RA prior to ICS versus ICS alone. In the Effects of Debulking on Restenosis (EDRES) trial, 150 patients were randomized to ICS alone versus RA with ICS (20). Although acute gain was the same in both arms, a reduction was observed in 6-month binary angiographic restenosis in the RA + ICS arm. In the larger Stent Implantation Post Rotational Atherectomy (SPORT) trial (Fig. 10.5), 750 patients were randomized to receive either percutaneous transluminal coronary angioplasty (PTCA) or RA prior to ICS (21). The procedural success rate was better in the RA group; however, no differences were observed in angiographic or clinical endpoints between the two groups at 6 to 8 months follow-up. These results may be explained by operator bias in excluding severely calcified lesions for enrollment in the trial. A prospective, randomized trial comparing RA (or PCA) with PTCA before ICS in patients with chronic total occlusion has reported that the strategy of debulking before stenting yielded significantly lower angiographic restenosis rates at follow-up (22). Aggressive RA before ICS might yield superior long-term results, yet it is associated with a higher incidence of periprocedural myocardial infarction (MI) (23).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree