8
Day-care and schools
Apart from homes, schools and day-care facilities are the most important indoor environments for children. Since (primary) school attendance is mandatory for children all over the world, schools – including their teachers and other employees are probably the largest work places. Even in 1880, Professor Heyman in Sweden observed the importance of the school environment. Observing that childrens’ health improved after the school term had ended in the summer, he concluded that ‘poor school room air’ affected school children negatively.
The school environment, including its buildings, varies considerably between and within countries and communities. For example, different climates may induce different environmental problems; high temperature may be a major problem in tropical countries, while the opposite may be relevant in countries with a cold climate. Outdoor pollutants, such as exhaust from traffic, may also be an indoor problem at schools. Furthermore, specific exposures occur in handicraft instruction and vocational schools.
Asthma and other allergic diseases are by far the most common chronic noninfectious diseases among children and young adults. The worldwide prevalences of asthma, rhino-conjuntivitis and eczema among school children vary considerably. According to phase III of the International Study of Asthma and Allergy (ISAAC) performed in 2002-2003, the prevalence of asthma symptoms was highest and more than 20% in several countries in Latin and South America, in Australia, New Zealand and the UK.
The reason for the increase in the prevalence of asthma and allergic diseases reported during the last five decades is unclear, but is probably related to changes in environmental and lifestyle factors. The indoor climate alone is probably not responsible for the prevalence increase, but is important at least in impairing those already diseased. Most studies of indoor environment have focused on homes, and generally the school environment and its relation to respiratory diseases have not been extensively studied. Most studies of the school environment have been performed in Scandinavia, the USA and China.
Several factors in the indoor environment of schools may cause respiratory symptoms, aggravate asthma and allergic diseases or facilitate the spread of infectious diseases. As in other buildings, high radon levels in school buildings may contribute to lung cancer. Thus, the school environment is of particular interest for many children and adults. This chapter summarizes the current knowledge about the school and daycare environment in relation to respiratory diseases.
Most of the critical exposures – such as damp, molds and bacteria, radon and environmental tobacco smoke – in premises for schools and day-care are not specific for these environments. However, for some factors, like dust, pet allergens and ventilation, the problem may be greater or different in schools and day-care compared with in homes.
Well-balanced ventilation is fundamental in maintaining thermal comfort and high indoor air quality. The primary role of ventilation is to remove airborne pollutants and supply the building with clean air. Thus, the outdoor air quality is important for the indoor environment. The levels of most indoor pollutants are dependent on the amount of outdoor air supply. Recommendations of ventilation rate for school buildings differ between countries; for example it is around 8 l/s per person in Sweden and USA, and 3 l/s per person in Japan.
Low classroom ventilation will result in elevated levels of carbon dioxide (CO2); indeed CO2 concentrations may be used as an indirect measure of ventilation rate, the correlation between the two being almost linear. In Sweden it is recommended that the level of CO2 not should exceed 1000 ppm; the corresponding value in Germany is 1500 ppm. Most schools worldwide do not have any mechanical ventilation, although it is common for instance in Scandinavian countries. Measurements of CO2 concentrations in schools have shown different levels. High concentrations have been found in schools in the UK (2100-5000 ppm), while lower levels were found in Denmark (500-1500 ppm). Generally, schools with natural ventilation have the higher levels. Ventilation by open windows during breaks is thus important. However, mechanical ventilation does not guarantee adequate ventilation. A study from Hong Kong found elevated levels of CO2 even in schools with air-conditioning or ceiling fans, indicating inadequate ventilation.
Indoor humidity is dependent on outdoor humidity, room ventilation, possible vapour built into the construction materials and emission from humans and their activities. Increased humidity may induce growth of molds and mites and increase emissions of volatile organic compounds (VOC). However, generally the total levels of VOC and mites are lower in schools than in offices and homes. Further, it has been shown that increased humidity may cause accumulation of indoor pet allergens.
Higher concentrations of airborne and settled microorganisms have been found in schools compared with offices. Concentrations in indoor air reflect the concentration of microorganisms in outdoor air, possible indoor sources and the effectiveness of the air filtration system. The proportion of Mycelia sterilia has been shown to be higher in schools than in homes, but the reason for this is not known. Actinomycetes species are common in buildings with dampness problems, but another major source of airborne bacteria is the occupants themselves.
The concentration of settled dust is often higher in classrooms than in work places for adults. Higher concentrations have been found in rooms with textile carpets compared with rooms with smooth floors, and levels of dust are increased by the quantity of open shelves or other storage in the room. It is probable that most dust comes from indoor sources as the concentrations of particles, both less than 2.5 μm and less than 10 μm, are higher in classrooms than outdoors. Because of the childrens’ or students’ activities in classrooms and day-care facilities, the level of airborne particles is high. The correlation between the indoor and outdoor concentrations has been shown to be modest, apart from ultrafine particles which are primarily of outdoor origin. Better cleaning of classrooms and adequate ventilation reduces the amount of dust.
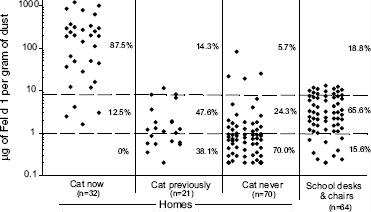
Despite pets being prohibited in most schools and day-care centers, allergens from cats and dogs are ubiquitous and found frequently in relatively high concentrations in schools worldwide. Pet allergens are transferred on the clothes and hair of pet owners from their homes to schools. The concentration of pet allergens in the classroom correlates well with the total number of pet owners in the class, and the concentrations are higher in classrooms with textile carpets than in rooms with smooth floors. The textiles act as reservoirs for allergens and dust. However, allergens from cats and dogs are easily found also in dust from smooth floors and desks. In total, the level of cat allergens is higher in schools than in homes without cats, but lower than in homes with cats (Figure 8.1). Cat allergen can be carried by very small particles, and these small particles can remain airborne for long time periods even if there is no air disturbance. Thus, the activities in a classroom will result in high concentrations of cat allergens in the air during the whole day.
Figure 8.1 Concentration of Fel d 1 in the dust from homes with and without cats as well as from school desks and chair samples in northern Sweden. Dashed lines represent the cut-offs between low and moderate (1 μg/g), and moderate and high (8 μg/g) allergen concentrations, respectively. Percentages indicate how many of the samples fall into each category. Reproduced with permission from the author: Perzanowski, M.S., Molecular epidemiology of allergen exposure, sensitization and asthma in school children. Umea University Medical Dissertation, Umea, Sweden, 2003; ISBN 91-7305-376-7
Earlier studies regarding allergen exposures did not usually focus on pet allergens. A study from the USA reported lower allergen levels in schools compared with in homes but focussed on mite, pollen and molds. In Norway and the Netherlands, mite allergen levels in schools were found to be low, compared with in homes. Generally mite allergen can be found in textiles and not in dust from smooth floors. This was confirmed by a study performed in Sweden where no mite allergens were found in dust from the floor from schools and day-care centers, while low levels of mite allergens could be detected in textiles.
A comparison between Northern Sweden and Virginia in the USA showed differences in allergen exposures at schools. In both Sweden and Virginia significant levels of cat and dog allergens were found. However, the levels of cat allergen were higher in Virginia while the levels of dog allergens were higher in Sweden. While no mite allergen was found in Sweden, mite allergens were detected in schools in Virginia, although the levels were lower than found in homes in Virginia. In China and Korea only low levels of furry pet allergen were found, probably reflecting a low prevalence of pet keeping at home. However, pet keeping is increasing in these countries and allergen exposures in schools may be an increasing problem in many parts of the world.
Apart from allergens from domestic pets, allergens from more undesirable animals may also be present in school buildings, especially those from cockroaches but also from rats and mice. In inner-city schools in the USA, concentrations of cockroach allergens are similar to those found in local homes
Food allergens may also be present in schools. In many countries children bring their own packed meal which may be eaten in special areas or in the classroom. Allergens from eggs and fish have been shown to be present in Norwegian classrooms at levels only slightly lower than in homes. One American study investigated the presence of peanut allergens at school, but found no airborne peanut allergen (Ara h 1), nor was it found on desks. However, it is obvious that peanut allergens may occur, at least on surfaces due to contamination by hands. It is probable that methods for measuring environmental peanut allergens need to be improved.
8.2.6 Environmental tobacco smoke
Throughout the world, there are initiatives to introduce policies to reduce smoking in public places, and in a large number of countries smoking is prohibited in schools and day-care facilities in front of the children. However, smoking may still be allowed in certain areas, and include smoking by both pupils and employees. Thus, exposure to environmental tobacco smoke (ETS), or ‘second hand smoking’, still occurs in schools in many countries.
Common methods to estimate exposure to ETS are to measure nicotine in room air or cotinine (a nicotine metabolite) in saliva, blood or urine. Nicotine has been detected in the air of most schools, including those where smoking is prohibited, but the mean concentrations are lower than in most other public environments. A survey in Latin America found nicotine levels that ranged from <0.01-0.2 μg/m3; the concentration tended to be related to the prevalence of smoking in the country. In Western Europe, median nicotine concentration in schools varied from 0.01 μg/m3 in Sweden to 1 μg/m3 in Austria. This may be compared with nicotine levels in homes of daily smokers, which usually range from 0.1 to 10 μg/m3, with a mean around 1 μg/m3.
An American prospective study followed infants during their first two years and measured cotinine in urine repeatedly. As expected, the strongest predictor of cotinine levels was having smoking parents. However, a significant and substantial contribution was also found from attending day-care away from home and frequency of smoking among day-care employees. In many infants, exposure to ETS from adults other than the parents resulted in cotinine levels that were higher than levels previously regarded as typical in children of smoking parents.
The main source of excess levels of radon in buildings is entry of radon from soil through cracks in the floor. This flow arises because buildings are often at a slightly negative pressure in respect to their surroundings. Basement or ground floor rooms are chiefly affected. Some building materials, such as certain types of lightweight concrete, may also be a significant source of indoor radon.
Many countries have target values for indoor radon concentrations. Several European countries have the same target value for domestic dwellings and workplaces. A common value is 400 Bq/m3. In other countries, there is a lower target value for schools than other types of workplaces. In several countries, including the USA, the target value for schools is 150 Bq/m3, but in other countries it is 200, 400 or even 1000 Bq/m3
Surveys of radon levels in schools have been conducted in different countries. In Ireland, 23% of schools had at least one room with an indoor concentration exceeding 200 Bq/m3. In Iran 15% of surveyed schools exceeded 400 Bq/m3 and in the USA 3% of schools had at least one room exceeding 150 Bq/m3. In day-care centers, the geometric mean was 44 Bq/m3 in Norway and 48 Bq/m3 in Slovenia. Recent data from Sweden indicate that 5% of schools and day-care centers have rooms with concentrations higher than 200 Bq/m3. Thus, in many countries there are schools and day-care centers with excessive radon levels.
8.2.8 Exposures in handicraft instruction and vocational schools
In addition to the general exposures in day-care and schools described above, students and employees in handicraft teaching and vocational schools are exposed to the same agents as those working in the professions taught, and their health may be affected in a similar way. Examples are schools of agriculture, veterinary science, technical arts, woodwork, needlework, cosmetics and hair styling, textiles, baking and food preparation. Each of these is associated with specific respiratory hazards.
8.3 Diseases associated with exposures in the school environment
Asthma is a common disease among children and all children have to attend school for several years. Despite this, it has been difficult to explore the effect of the school environment on the development of asthma and allergic diseases. The reasons are several. First, the incidence of asthma in early school age is around 1/100/year. This means that it is necessary to study large cohorts including several schools prospectively for several years. Secondly, as no school is exactly like another, objective exposure measurements are needed from all studied schools, which is costly. Furthermore, the home environment may be a confounding factor and should also be studied in the same manner. Thus, data regarding the school environment and development of allergic diseases are scarce.
Regarding the environmental effects on subjects who already have developed asthma or other allergic diseases, the knowledge is somewhat better. Studies on school attendance give a uniform picture showing that subjects with asthma have more sick-leave from school compared with children without asthma. Further, children with asthma reported increased symptoms when attending school, and complaints were significantly related to the severity of the disease. Thus improvement of the school environment is important.
Other respiratory diseases such as extrinsic allergic alveolitis (EEA) and pulmonary fibrosis may be related to exposures in vocational schools. However, these are mainly work-related problems and are described fully in Part III – the work environment.
Because of the relatively high person density, viral infections are common in day-care and schools, and epidemics of common colds and respiratory infections easily start. Good hygiene practices are essential. From other indoor environments, it has been shown that a low building ventilation rate may affect the spread of infectious disease, but there are few studies from schools investigating this factor.
Among school employees, reduced nasal patency and an inflammatory biomarker response of the nasal mucosa have been related to low air exchange rate and old mechanical ventilation systems. An intervention study showed that pupils attending schools that got a new ventilation system had fewer asthmatic symptoms than pupils in other schools. The main cause is that poor ventilation in schools results in accumulation of several pollutants, both chemical and biological, in the air. These pollutants may induce respiratory or other allergic symptoms. It is known that VOC emitted from building materials and building occupants are often increased in indoor environments and particularly if the ventilation is poor. These substances have been associated with sensory irritation in the eyes and the nose. Recent studies from both schools and homes indicate that increased levels of VOC may also be associated with lower respiratory symptoms. Furthermore, poor design and maintenance of the ventilation system may result in microbial growth in filters and ducts that affects indoor air quality and health.
High concentrations of CO2 have been related to tiredness, but there is no evidence that everyday levels of CO2, per se, have any impact on respiratory health. However, an American study found a 10-20% increase in student absence due to illness per 1000 ppm increase of concentration of CO2 in the classroom. Apart from installing a more effective ventilation system, a warning device showing when the CO2 level is too high with consequent advice to improve airing by opening windows has been shown to improve indoor air quality.
While a cold winter climate may aggravate asthma symptoms, there is no evidence that average indoor temperatures have any impact on respiratory health, although they may present a comfort problem. Because of low ventilation rates and high person densities, schoolroom temperatures are often relatively high, at least during sunny periods.
8.6.1 Indoor humidity, dampness and molds
Damp in the home has been identified as a risk factor for respiratory symptoms and asthma among both children and adults in several studies in different parts of the world, but the explanation is still unclear. It may be due to mold exposure, increased occurrence of dust mites, or emissions of chemical substances.
Studies performed in schools show that attendance at a school with mold growth or problems with damp is related to an increased risk of respiratory symptoms, asthma medication use and asthma. A study from Denmark found that mold in dust was related to an increased prevalence of eye irritation, throat irritation and headache. Further, after remediation of a mold-damaged school, bronchitis and episodes of respiratory infections decreased among teachers.
Subjects with asthma often report increased symptoms when exposed to dust. Dust contains a large number of different particles, including biological compounds such as allergens. A Danish study found that the inflammatory potential of the dust was related to its content of organic compounds, and dust collected from schools with more health complaints had a higher inflammatory potential than dust from other schools.
Studies of respiratory health effects due to dust in the school are scarce, but children with asthma showed increased respiratory obstruction if they slept in a dusty room at home. The level of inflammatory markers in nasal lavage fluid was higher among school employees working in schools with increased levels of settled dust, and the prevalence of asthma among the children was higher. In contrast, studies from the Netherlands failed to show any correlation between the presence of textile carpets in schools (which may indicate higher dust levels) and expiratory peak flow variability among children with asthma. However, in a study among staff in schools and kindergartens, 50% of the employees complained of dust in the air.
Avoidance of pets is an established and effective strategy to prevent allergic symptoms among subjects with a known allergy to pets. Nevertheless, in schools and day-care centers, children with pet allergy are often exposed to allergen levels that are high enough to evoke allergic symptoms such as asthma, rhino-conjuntivitis and eczema. Furthermore, levels may also be high enough to induce allergic sensitization among children. Most sensitized children have never lived in a home with a cat or dog, and schools and day-care centers are probably a major site of allergen exposure.
Few studies report the clinical effects of allergen exposures at schools. However, pupils with asthma and furry pet allergy had impaired lung function and more respiratory symptoms in the first week of the school term, but only if they attended a class with many cat owners. Similarly, pupils with asthma and allergy to furry pets had increased bronchial hyperresponsiveness after exposure to the school environment.
8.6.4 Environmental tobacco smoke
The adverse health effects from exposure to ETS in both adults and children are well-known. Major effects in children include an increased prevalence of lower respiratory tract illness and asthma. Thus, introducing and effectively implementing policies against smoking in schools and day-care centers should be important measures, besides others, in reducing the negative health effects of smoking.
Radon in buildings contributes to an excess risk of lung cancer. The risk is supposed to have a linear dose-response relation with no threshold. Several attempts have been made to calculate the radiation dose due to indoor exposure to radon, particularly in homes. The population’s mean annual effective dose typically is lower than 1 mSv; however, the range is very wide. Only a few studies have calculated the contribution from school attendance to this dose. An Irish study found that the mean radon concentration in schools was similar to that in domestic dwellings (93 and 89 Bq/m3, respectively) and calculated an annual effective dose of 0.3mSv from exposure in schools. A Greek study calculated an annual effective dose of 0.1 mSv for students and 0.2 mSv for teachers, based on a mean radon concentration of 35 Bq/m3.
For risk management, and as no safe threshold level is shown, reducing the mean population dose as well as that in high-exposure individuals is equally important. A British study estimated the cost-effectiveness of radon remediation programs in different kinds of buildings and concluded that it is most cost-effective to conduct such programs in schools with high levels. Because of the high person density in schools, the cost per reduced Man-Sievert is much lower in schools than in homes.
8.7 Diagnosis and management issues
For clinicians it is important to keep in mind that a patient’s reported symptoms may be related to the school environment. A detailed medical history is important in order to make a correct diagnosis. The next step is to consider which situations or environments could be the triggering factors. Skin prick testing or measurement of specific IgE are helpful in considering problems that may have an allergic mechanism. Serial peak expiratory flow measurements in subjects with asthma symptoms before and during attendance at school may be useful. Peak flow measurements are also helpful in judging the effectiveness of any intervention actions at school. Cooperation with the school’s health care providers is important. In addition, normal medical treatment following standard guidelines must be advised. Among schoolchildren, anaphylactic shock or similar severe reactions are primarily food-related. It has been shown that the outcome of such a reaction is worse if the onset is in school, probably because of substandard and/or delayed care in the school setting. Thus education of pupils and school employees should be improved regarding the signs, symptoms, and measures to take.
8.7.1 Intervention trials at schools and day-care centers
Allergen and dust intervention
In some countries, schools may offer extra cleaning of classrooms for severely allergic children; however, this intervention has not been adequately evaluated. Although in office environments, intervention studies have shown positive effects of cleaning, very few intervention studies have been performed in schools and day-care centers; most report only changes in exposures, while the health effects are less studied.
Studies from Sweden showed that the level of pet allergens at day-care centers could be reduced by intervention measures. In one of the studies, allergen levels were measured before and after extensive renovation, including installation of a new ventilation system. Old textiles including mattresses, pillowcases, curtains and sofas were removed and exchanged with new material. The cleaning routines were changed and the families and the school employees had to avoid direct and indirect contact with pets. Immediately after the renovation, the level of cat and dog allergen decreased dramatically, and the levels were still lower than before the intervention after one year. Another study compared the levels of pet allergens in ‘allergen avoidance’ and conventional day-care centers and found reduced levels of pet allergens in the former. Of importance in both these studies is that none of the families or the staff in the intervention centers were cat or dog owners.
Another study evaluated the intervention effect on cat allergen levels with no restrictions regarding contacts with pets; several other actions were taken, including removal of upholstery and plants, replacement of bookshelves with cupboards and changes of the cleaning routines. Serial measurements of allergens were performed before and after these intervention measures. The study concluded that the allergen avoidance measures used did not reduce the levels of airborne cat allergens. However, the intervention was only partially successful in reducing the amount of dust-collecting fittings, and there was no increased cleaning of furniture (which has been shown to be correlated to the level of airborne particulates). An Australian intervention study aimed at creating a ‘low allergen school’ by limiting the amount of dust-collecting fittings, increasing air exchange and using a central vacuum cleaner demonstrated a cat allergen level that was about one-third of levels in control schools.
The level of pet allergens in a classroom correlates strongly with the number of pet owners. Further, by introducing school uniforms and a ban on pet owning, the level of airborne cat allergen at schools can be reduced. Intervention studies including either or both of these factors typically have reduced allergen levels in school by around 90%, while other interventions have resulted in lower reductions, if any.
In summary, the clinical effects of increased regular cleaning of classrooms are unclear. Intervention studies on exposure conclude that reducing incoming allergens is the most effective measure to reduce the allergen level in the school environment. This can be achieved by reducing the number of children and school employees who have pets at home or by the use of special school clothes that are not in use at home.
Hygiene intervention
A study in Finland investigated the effect of increased hygiene at day-care centers. The intervention lasted for 15 months and included several steps; the most important was increased hand hygiene by the use of an alcohol-based hand rub. Both the children and the personnel in the intervention centers had significantly fewer respiratory infections compared with the control centers, and the use of antimicrobials among the children decreased by 24%. A 12 year follow-up survey of the children who had participated in the study concluded, however, that that the decrease in infections did not affect the development of asthma or other allergic diseases in any direction.
Despite it being well-known that the environment in schools and day-care centers is not optimal, and that many children with allergic symptoms experience increased symptoms daily at their work place, the school, few studies have evaluated the health impact of the indoor environment at school.
Today there is an increasing interest in the school environment in relation to health with an increasing number of national and international studies and campaigns. For instance, the US Environmental Protection Agency has developed an ‘Indoor Air Quality Tools for Schools’ program and the European Union is supporting research on ‘Health Effects of the School Environment’. A Swedish national position paper on how schools should deal with asthma and allergies was published in 2002. It stated that schools should bear the responsibility for their students’ health and substances that trigger allergic reactions and respiratory irritation should be kept to a minimum. Furthermore, the students should not exhibit symptoms, nor need to increase their medicines due to conditions at schools.
In order to obtain an environment in schools and day-care centers that do not contribute to respiratory disease and are safe for those already affected, these recommendations are given:
Keep the building ‘healthy’:
- fulfil ventilation standards;
- maintain the building adequately;
- prevent problems with damp and repair damage;
- reduce high radon levels;
- design the building and its fittings so that it is easily cleaned;
- keep a high standard of cleaning, including textiles.
Take care of one another:
- avoid smoking;
- avoid strong scents and spray products;
- do not keep allergenic plants indoors;
- discuss how to reduce the entry of pet allergens.
Further reading
Allerman, L., Meyer, H.W., Poulsen, O.M., Nielsen, J.B., Gyntelberg, F. (2003) Inflammatory potential of dust from schools and building related symptoms. Occup. Environ. Med. 60(9): e5.
Belanger, E., Kielb, C., Lin, S. (2006) Asthma hospitalization rates among children, and school building conditions, by New York State school districts, 1991-2001. J. Sch. Health 76(9): 408-413.
Dunder, T., Tapiainen, T., Pokka, T., Uhari, M. (2007) Infections in child day care centers and later development of asthma, allergic rhinitis, and atopic dermatitis: prospective follow-up survey 12 years after controlled randomized hygiene intervention. Arch. Pediatr. Adolesc. Med. 161: 972-977.
Godwin, C., Batterman, S. (2007) Indoor air in Michigan schools. Indoor Air 17: 109-121.
Karlsson, A.S., Andersson, B., Renström, A., Svedmyr, J., Larsson, K., Borres, M.P. (2004) Airborne cat allergen reduction in classrooms that use special school clothing or ban pet ownership. J. Allergy Clin. Immunol. 113: 1172-1177.
Lee, S.C., Chang, M. (2000) Indoor and outdoor air quality investigation at schools in Hong Kong. Chemosphere 41: 109-113.
Meyer, H.W., Wurtz, H., Suadicani, P., Valbjorn, O., Sigsgaard, T., Gyntelberg, F. Members of a Working Group under the Danish Mould in Buildings Program (DAMIB) (2004). Molds in floor dust and building-related symptoms in adolescent school children. Indoor Air 14: 65-72.
Mi, Y.H., Norbäck, D., Tao, J., Mi, Y.L., Ferm, M. (2006) Current asthma and respiratory symptoms among pupils in Shanghai, China: influence of building ventilation, nitrogen dioxide, ozone, and formaldehyde in classrooms. Indoor Air 16: 454-464.
Nebot, M., Lopez, M.J., Gorini, G., Neuberger, M., Axelsson, S., Pilali, M., Fonseca, C., Abdennbi, K., Hackshaw, A., Moshammer, H., Laurent, A.M., Salles, J., Georgouli, M., Fondelli, M.C., Serrahima, E., Centrich, F., Hammond, S.K. (2005) Environmental tobacco smoke exposure in public places of European cities. Tobacco Control 14: 60-63.
Perzanowski, M.S., Rönmark, E., Nold, B., Lundbäck, B., Platts-Mills, T.A. (1999) Relevance of allergens from cats and dogs to asthma in the northernmost province of Sweden: schools as a major site of exposure. J. Allergy Clin. Immunol. 103: 1018-1024.
Rönmark, E., Perzanowski, M., Platts-Mills, T., Lundbäck, B. (2002) Incidence rates and risk factors for asthma among school children: a 2-year follow-up report from the obstructive lung disease in Northern Sweden (OLIN) studies. Respir. Med. 96: 1006-1013.
Smedje, G., Norbäck, D. (2001) Irritants and allergens at school in relation to furnishings and cleaning. Indoor Air 11: 127-133.
Synnott, H., Hanley, O., Fenton, D., Colgan, P.A. (2006) Radon in Irish schools: the results of a national survey. J. Radiol. Protect. 26: 85-96.
Zhang, G., Spickett, J., Rumchey, K., Lee, A.H., Stick, S. (2006) Indoor environmental quality in a ‘low allergen’ school and three standard primary schools in Western Australia. Indoor Air 16(1): 74-80.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


