Cystic Mediastinal Mass
Christopher M. Walker, MD
DIFFERENTIAL DIAGNOSIS
Common
Bronchogenic Cyst
Thyroid Goiter
Pericardial Cyst
Less Common
Necrotic Lymph Nodes
Necrotic or Cystic Neoplasms
Rare but Important
Other Foregut Duplication Cysts
Lymphangioma
Pseudocyst from Pancreatitis
Mediastinal Abscess
Lateral Meningocele
Thymic Cyst
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Key diagnostic feature is location and clinical presentation
10% of mediastinal masses in adults and children are cysts
Most mediastinal cysts are congenital in origin
Helpful Clues for Common Diagnoses
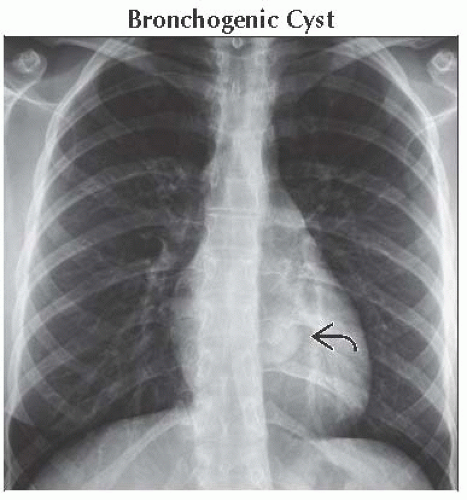
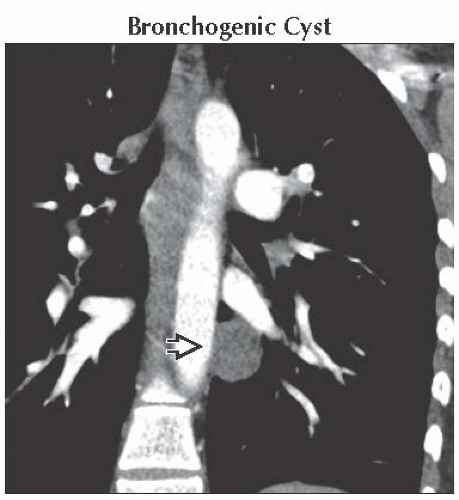
Bronchogenic Cyst
Most common foregut duplication cyst
Occur in middle or posterior mediastinum
Paratracheal or subcarinal in location
Round and smooth in contour
Wall typically thin or imperceptible
Water to soft tissue density
Radiograph shows
Smooth and sharply marginated round mass
May displace bronchi or trachea
Rarely cause collapse of a lobe secondary to mass effect on bronchi
Distinguish from soft tissue neoplasm by
Lack of enhancement
Characterization by MR
May abruptly increase in size secondary to hemorrhage or infection
MR shows
High T1 signal secondary to proteinaceous content
High T2 signal in nearly all cases
Thyroid Goiter
10% of mediastinal masses
Radiograph shows
Leftward tracheal deviation
Mass in superior mediastinum
Noncontrast CT shows
High-attenuation cystic or heterogeneous lesion
Connection to thyroid on sequential images
Coronal images are key to demonstrate connection
Factors that suggest thyroid malignancy
Lymphadenopathy or metastases
Invasion of adjacent structures
Pericardial Cyst
Smooth and well marginated
Most contact diaphragm
Majority right-sided and asymptomatic
Low Hounsfield units by CT
Single layer of mesothelial cells
Helpful Clues for Less Common Diagnoses
Necrotic Lymph Nodes
Rim-enhancing lymph node with central low density indicating necrosis
Infectious causes include tuberculosis and histoplasmosis
Malignant causes include lymphoma or lung cancer
Extrathoracic malignancies, such as head and neck carcinoma, seminoma, or gastric carcinoma
Necrotic or Cystic Neoplasms
Germ cell tumors (teratoma, seminomas, and nonseminomatous tumors)
Teratomas are anterior mediastinal, well defined, cystic in appearance, ± fat and calcification
Seminomas are anterior mediastinal, homogeneous in density, ± low-attenuation areas, in younger men
Nonseminomas are anterior mediastinal, heterogeneous with areas of necrosis or cystic areas
Large thymomas or thymic carcinomas
Helpful Clues for Rare Diagnoses
Other Foregut Duplication Cysts
Esophageal duplication cyst
Similar appearance to bronchogenic cyst
Occur within esophageal wall or contact esophagus
Lined by gastrointestinal mucosa
Neurenteric cyst
Posterior mediastinal mass
Connection to meninges through a vertebral defect
Vertebral anomalies include scoliosis or hemivertebrae
Identical appearance to other duplication cysts
Composed of neural and gastrointestinal components
Lymphangioma
Most common in childhood; extend down from neck
Commonly localized to mediastinum in adults
Unilocular or multilocular ± thin septations
May drape over structures and can grow to large size
MR demonstrates heterogeneously increased T2 signal
Pseudocyst from Pancreatitis
Located in lower mediastinum with access via esophageal or aortic hiatus
Clinical history of pancreatitis ± lesion tracking from abdomen
Mediastinal Abscess
Recent history of median sternotomy, esophageal perforation, or head and neck infection
Typical rim-enhancing lesion with central low density
May demonstrate air bubbles with communication to adjacent infection
Difficult to differentiate from postoperative hematoma/seroma
May require needle aspiration
Postoperative hematoma/seroma should resolve after 2-3 weeks
Lateral Meningocele
Strong association with neurofibromatosis type 1 or connective tissue disorders
Posterior mediastinal cystic mass with extension into spinal canal
Associated scoliosis and interpediculate widening
MR or myelogram are diagnostic by showing connection to spinal canal
Thymic Cyst
Usually incidental; may be unilocular or multilocular
Thin walls
Congenital or acquired secondary to radiotherapy after Hodgkin disease
Fluid density
Occasionally may contain fat or hemorrhage
Image Gallery
 (Left) Esophagram shows external mass effect on the anterior esophagus
 . The underlying mucosa is intact indicating this is an external process. Cross-sectional imaging would need to be performed for further characterization. (Right) Coronal CECT shows a well-circumscribed, low-attenuation mass . The underlying mucosa is intact indicating this is an external process. Cross-sectional imaging would need to be performed for further characterization. (Right) Coronal CECT shows a well-circumscribed, low-attenuation mass  causing compression of the left mainstem bronchus (not shown) with complete collapse of the left lung causing compression of the left mainstem bronchus (not shown) with complete collapse of the left lung  . Note the reduced volume of left hemithorax. . Note the reduced volume of left hemithorax.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|