Fig. 34.1
Static balloon dilation of restrictive atrial communication (a) 12 mm balloon inflated at mild pressure delineating the small atrial communication (b) full inflation stretches-tears the septum.
34.8 Stent Implantation in Congenital Heart Defects: Nonrestrictive Technique
A restrictive interatrial communication in patients with univentricular anatomy significantly affects surgical outcomes. In patients with univentricular hearts, wide-open atrial communication leads to lower pulmonary artery pressure, which is one of the most important factors influencing the success of bidirectional Glenn and Fontan operations. In some patients, recurrence of restricted interatrial communication can be observed despite initially successful interventional or surgical creation of unrestrictive interatrial communication. Atrial stent septostomy can provide a reliable long-lasting restrictive or nonrestrictive interatrial communication.
34.8.1 Procedure
After access has been obtained in the left atrium, a wire should be positioned in a pulmonary vein and an appropriate-sized long sheath advanced over the wire with the tip across the atrial septum. Premounted balloon-expandable stents are preferable in this setting although self-expandable stents have been used with success in some patients. The stent diameter will depend on the age and size of the patient and the type of congenital anomaly (especially atrial size), aiming to provide an unrestrictive and potentially durable flow through the interatrial septum for several months. One of the crucial facts is to avoid implanting too long stents due to the risk of atrial erosion, thrombus formation, and obstruction of the pulmonary veins. The stent should be long enough though to allow adequate stabilization within the interatrial septum, minimizing the risks of embolization due to movement during inflation or due to foreshortening after expansion. We advise using the technique of sequential stent flaring to facilitate accurate stent positioning. The stent is advanced through the long sheath into the left atrium. Half of the stent is exposed by pulling back the sheath and the balloon is inflated in the left atrium, expanding the distal half of the stent. Pressure in the balloon is maintained using a stopcock. Next, the entire system is firmly pulled back against the atrial septum. The pressure in the delivery balloon is slightly released, allowing the right atrial portion of the stent to be unsheathed. The balloon is then fully inflated, opening the proximal portion of the stent. The deflated balloon should be removed carefully out of the stent into the long sheath, avoiding stent dislodgment. We advise against crossing the newly implanted stent with a catheter unless certainty of adequate fixation. Gradients and flow across the interatrial septum should be assessed using TTE or TEE (Fig. 34.2). In contrast to conventional balloon atrial septostomy, stent implantation requires anti-aggregation treatment (acetylsalicylic acid 2–5 mg/kg/day) to prevent thrombus formation.
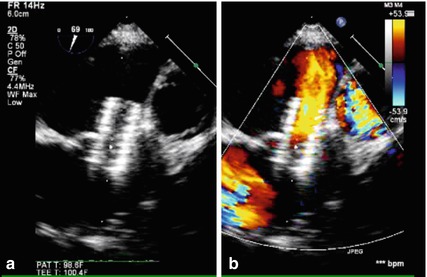
Fig. 34.2
TEE of stent across atrial septum (a) a Genesis 1910 stent is nicely positioned across the atrial septum (b) color flow mapping shows right-to-left shunt across the stent
34.9 Stenting of the Interatrial Septum: Restrictive Technique
34.9.1 Pulmonary Arterial Hypertension
Atrial septostomy for severe pulmonary arterial hypertension (PAH) improves cardiac index and functional class by the creation of a right-to-left atrial shunt and may even improve the survival in some patients. The presence of this iatrogenic shunt decompresses the failing right ventricle and improves left ventricular preload and thus cardiac index. Early series reported a high mortality, largely caused by difficulty in achieving accurate control of the size of the atrial shunt. Improvements in patient selection and septostomy techniques (i.e., sequential balloon dilation) have increased the safety of the procedure; however, a high spontaneous closure rate is observed after balloon dilation, necessitating repeated procedures in an already critically ill patient group. The recent evidence-based treatment guidelines for PAH list the indication for the atrial septostomy procedure as Class 1C, generally limited to specialized centers and reserved for patients with recurrent syncope and those who are refractory to, or intolerant of, medical therapy or as a bridge to transplantation. In contrast with balloon septostomy, restrictive stenting of the interatrial septum with the use of a diabolo-shaped (bow tie or dog bone stent) allows for a predictable and long-lasting interatrial shunt in these patients. The fenestration technique currently used in our unit has been adapted from [3], who described a small mixed series of primary PAH patients and patients with a failing Fontan circulation. A venous sheath up to 12 Fr is placed into the right femoral vein, followed by a puncture of the interatrial septum with a Brockenbrough needle.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


