Outline the common causes of cough and discuss the underlying mechanism and pathogenesis.
Outline the common causes of cough and discuss the underlying mechanism and pathogenesis.
 Develop a clinically based algorithm for the diagnosis and management of chronic cough relative to disease-specific pathophysiology.
Develop a clinically based algorithm for the diagnosis and management of chronic cough relative to disease-specific pathophysiology.
GENERAL CONSIDERATIONS
 Cough is not common in healthy persons. It plays a major role in maintaining the defense of the airways and in clearing mucus and foreign particles. Cough can also spread disease, signify an underlying serious pathologic condition, affect the quality of life, and interfere with a person’s daily routine or occupation. Chronic cough, defined as cough persistent for three or more weeks, is one of the most troubling symptoms for which a patient seeks medical attention and is a common problem seen in both pulmonary and general medical practice. Referrals of patients with chronic cough account for up to 30% of the outpatient practice of a pulmonologist in the United States.
Cough is not common in healthy persons. It plays a major role in maintaining the defense of the airways and in clearing mucus and foreign particles. Cough can also spread disease, signify an underlying serious pathologic condition, affect the quality of life, and interfere with a person’s daily routine or occupation. Chronic cough, defined as cough persistent for three or more weeks, is one of the most troubling symptoms for which a patient seeks medical attention and is a common problem seen in both pulmonary and general medical practice. Referrals of patients with chronic cough account for up to 30% of the outpatient practice of a pulmonologist in the United States.
ETIOLOGY & PATHOGENESIS
 Acute cough is generally a manifestation of an acute inflammatory or infectious process and may not require any specific investigation. Although it is usually self-limiting, it can be protracted after an acute viral respiratory tract illness and may linger for several weeks. In smokers, bronchial secretions induced by smoking may cause cough. Although most smokers have cough, they often do not complain of it. Almost every pulmonary disorder, either directly or indirectly, can cause cough. Chronic cough may be associated with altered mucus expectoration as in chronic bronchitis or with increased reactivity of airways as in asthma. It can be present with aspiration, as in esophageal dysfunction or neurologic disorders, or associated with signs of local compression, as in lung/bronchogenic cancer, mediastinal tumors, thyroid or vascular enlargement. It is also seen with pulmonary edema or pulmonary fibrosis. It has been observed that in more than 90% of immunocompetent patients complaining of cough with a nonlocalizing chest radiograph, the cause is upper airway cough syndrome (UACS), previously called postnasal drip. Other causes in this category include gastroesophageal reflux disease (GERD), asthma, or chronic bronchitis. Therefore, in nonsmoking patients and in those not taking any medication that can cause cough, such as an angiotensin-converting enzyme (ACE) inhibitor, chronic cough is most likely due to one of these conditions.
Acute cough is generally a manifestation of an acute inflammatory or infectious process and may not require any specific investigation. Although it is usually self-limiting, it can be protracted after an acute viral respiratory tract illness and may linger for several weeks. In smokers, bronchial secretions induced by smoking may cause cough. Although most smokers have cough, they often do not complain of it. Almost every pulmonary disorder, either directly or indirectly, can cause cough. Chronic cough may be associated with altered mucus expectoration as in chronic bronchitis or with increased reactivity of airways as in asthma. It can be present with aspiration, as in esophageal dysfunction or neurologic disorders, or associated with signs of local compression, as in lung/bronchogenic cancer, mediastinal tumors, thyroid or vascular enlargement. It is also seen with pulmonary edema or pulmonary fibrosis. It has been observed that in more than 90% of immunocompetent patients complaining of cough with a nonlocalizing chest radiograph, the cause is upper airway cough syndrome (UACS), previously called postnasal drip. Other causes in this category include gastroesophageal reflux disease (GERD), asthma, or chronic bronchitis. Therefore, in nonsmoking patients and in those not taking any medication that can cause cough, such as an angiotensin-converting enzyme (ACE) inhibitor, chronic cough is most likely due to one of these conditions.
Mechanism
Cough is a complex event that protects against thermal, chemical, or mechanical insult or injury. It is a normal response to inhalational exposure to particulate matter or chemicals and after aspiration. However, it may be the only sign of a number of diseases and disorders, including inflammatory processes, mechanical changes, or chronic inhalation of irritants. The mucus normally produced by the secretory cells of the airways entraps irritant particles and chemical and endogenous debris, with the clearance mechanism being initiated by mucociliary action. A cough dramatically enhances this process by narrowing the airway and increasing the velocity of airflow, resulting in more turbulence and clearance of pollutants in larger airways. Vagal receptors and recurrent laryngeal nerve receptors can induce coughing when stimulated by airways secretion, foreign bodies, or tumors. Sensory nerve receptors such as rapidly adapting receptors (RARs), slowly adapting receptors (SARs), and C-fiber receptors form the conducting pathway in the response of external stimuli causing cough. These stimuli may be external, such as external cigarette smoke, mechanical stimuli, acidic or alkaline, hypo- or hypertonic solutions, or intrinsic, such as bronchoconstriction, pulmonary congestion, atelecasis, or pulmonary/interstitial fibrosis. An abnormal increase in the sensitivity of these cough receptors can cause a lower threshold for coughing, such as seen with cough induced by ACE inhibitors. Diabetic patients with autonomic neuropathy also have an increased cough reflex threshold.
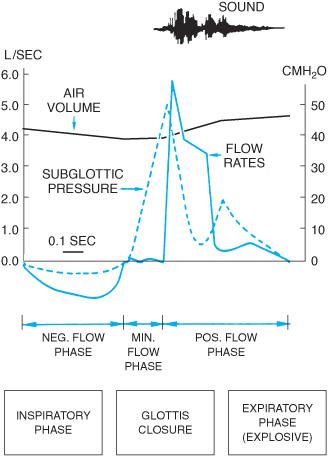
The components of the cough reflex have been well described. They are the (1) receptors, (2) afferent pathways, (3) cough center, (4) efferent pathway, and (5) effectors. The irritant receptors, such as those sending afferent myelinated fibers via the vagus nerve, are primarily in the large airway and on the luminal side of the tracheobronchial tree. Stimulation of the mechanical and chemoreceptors produces cough, airway constriction, and increased mucus secretion. These receptors are also abundant at the bifurcations of bronchi, especially at the carina. The cough reflex (Table 2–1) is initiated by stimulation of sensory nerves beneath and between the epithelium of the larynx and tracheobronchial tree. Involuntary coughing appears to be entirely vagally mediated and can be initiated by irritation of any structure innervated by the vagus nerve or its branches. These structures include the oropharynx, the larynx, the lower respiratory tract, and the esophagus. Afferent impulses travel to the cough center in the brain via various neural pathways. Efferent signals are then transmitted to the glottis, diaphragm, intercostals, and abdominal muscles. This culminates in (1) an inspiratory phase, (2) closure of the glottis, (3) diaphragmatic relaxation, (4) active contraction of the expiratory muscles with intrapleural pressures rising up to 200 mm Hg, and (5) rapid opening of the glottis. The physiologic process of coughing, specifically that which originates from the lower airways (Figure 2–1), starts with rapid inspiration, usually but not necessarily followed by glottal closure for about 200 ms, a rise in pleural and abdominal pressure to 50–100 mm Hg by expiratory muscle contraction, followed by an explosive exhalation. When the glottis suddenly opens, the high pressure gradient between the pleura and the airway produces an explosive release of air accompanied by a sound produced by turbulence. Although expiratory volume is no greater than during forced exhalation, narrowing of the airways caused by the large transpulmonary pressure gradient leads to a high flow velocity. The cough event lasts about 0.5 s, during which up to a liter of air may be expelled. This expulsion is followed by glottic closure and then respiratory muscle relaxation. At times, there is a series of coughs during a single exhalation phase, diminishing in intensity as the residual volume is approached. During cough, dynamic compression of airways occurs initially in segmental or lobar bronchi immediately above the equal pressure point. Maximum flow is determined by the resistance of upstream intrapulmonary airways, by the elastic recoil of the lungs, and by the collapsibility of the airways.
Table 2–1. Components of cough reflex
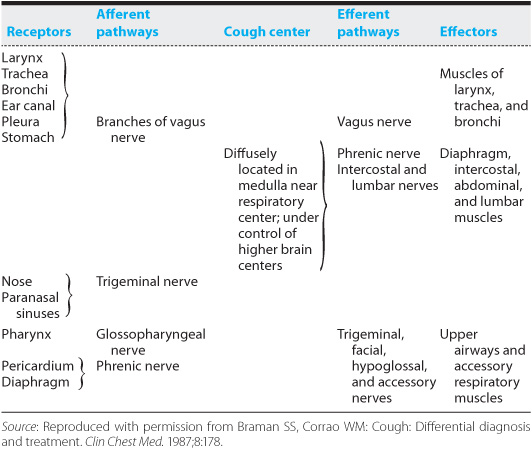
Figure 2–1. Flow and volume changes in cough. (Reproduced with permission from Bianco S, Robuschi M: Mechanics of cough. In: Braga PC, Allegra L, eds. Cough. New York, Raven Press, 1989, pp 29–36.)
Measurement of the effectiveness of coughing is difficult. Furthermore, patients with severe chronic lung disease may generate low linear velocities and thus have ineffectual cough. In chronic bronchitis, cough may account for 50% clearance, thus compensating for any defective mucociliary transport. Clinical studies show that coughing is highly effective in central airways clearance but not in the peripheral airways.
As a defense mechanism, cough helps prevent any foreign material from entering the lower respiratory tract and also clears excessive secretions. The effectiveness of cough depends on the viscosity of the secretions and the linear velocity of air moving through the lumen. Once there is material of sufficient thickness for expulsion from the airways, the effectiveness of cough depends on the high flow rate of air and the small cross-sectional area of the airway in order to achieve a high linear velocity. Therefore, any condition associated with a diminished expiratory flow rate or reduced ability to dynamically compress airways may lead to an ineffective cough. Since expiratory flow rates are directly related to lung volume, failure to take an initial breath and reluctance to give a forceful expiratory effort often lead to an ineffective cough velocity. Unconscious patients who have central nervous system depression may also have decreased cough due to central depression of cough reflexes. Pulmonary disorders may have cough impairment associated with decreased expiratory flow rates or production of overwhelming amounts of secretions. In asthma, both these conditions may cause cough ineffectiveness. Inflammation, edema, smooth muscle contraction, narrowing of airways, increased resistance to inspiratory and expiratory flow rates, and tenacious viscous secretions may partly occlude the lumen. This occlusion, combined with respiratory muscle fatigue, may diminish flow rates.
PATHOPHYSIOLOGY
Causes of chronic cough include a number of clinical conditions, some of which are mentioned in the following section. The disease-specific pathogenesis and pathophysiology are discussed.
Asthma & Cough-Variant Asthma
One of the three most common causes of chronic cough in a nonsmoker is asthma and/or cough-variant asthma. Cough due to asthma is usually accompanied by wheezing and chest tightness. These accompanying symptoms may be absent in cough-variant asthma. Typically, the onset of cough in cough-variant asthma occurs for a few months following an upper respiratory tract infection and persists for several months. These patients may progress to asthma in 30% of cases. This cough is worse at night, and it may also increase after exercise. Overt wheezing is generally undetectable and spirometric test results are normal. Allergy testing may show a positive reaction to ragweed. Exercise testing or methacholine challenge reveals a decrease in flow rates with protracted cough consistent with airway hyperreactivity and asthma. Sputum eosinophilia is frequent with increased submucosal and bronchoalveolar lavage eosinophilia. Exhaled nitric oxide concentration is raised in these conditions. Management of asthma relieves the cough, and response to corticosteroids is generally good. There is no significant correlation between cough sensitivity and bronchial hyperreactivity, even in inflammation or asthma. Asthma stimulates cough through induction of airways secretion, bronchial hyperreactivity, and eosinophilic inflammation. Bronchoconstriction per se may be associated with cough. While histologically those receptors that mediate the cough reflex are indistinguishable from those that mediate bronchoconstriction, recent evidence suggests that the cough receptors are functionally different from other irritant receptors and that cough may occur as a reflex that is independent of bronchoconstriction. Rapid and large lung volume changes can cause cough, as can physiologic effects such as laughter. Stretch receptors innervate slowly adapting fibers and do not cause cough. Bronchoconstriction is believed to be caused by activation of C-fiber and other receptors. The C-fiber receptors are highly sensitive to chemicals such as bradykinin, capsaicin, and hydrogen ions and form a complex unit of cough sensors in the airways. Alteration of local osmolality, such as that caused by an inhalant solution, can result in bronchoconstriction. Cough can also result from excessive respiratory water loss, whereas bronchoconstriction is believed to result from respiratory heat loss. Each can potentiate the other, although neither is dependent on the other for its action. Studies during sleep show that greater stimulation of the larynx is needed to produce cough in the rapid eye movement (REM) stage than in lighter stages of sleep, and in patients with chronic cough, less coughing occurs during REM than during non-REM sleep or waking periods.
Chronic Cough Due to UACS
Cough may be persistent with recurring bouts of bronchorrhea and rhinitis and postviral illnesses. Because of their superficial location, the sensory receptors in the upper airways make them easily susceptible to irritation. These rapidly adapting receptors release mediators and various components of the inflammatory cascade which can cause increased vascular permeability, airway hyperreactivity, and cough. Patients may also complain of a postnasal dripping sensation at the back of the throat. Examination of the pharynx may reveal a granular or cobblestone-like mucosa. Tenderness of the sinus areas may also be present.
GERD With or Without Microaspiration
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree