Chapter 18 Cough
The Cough Reflex
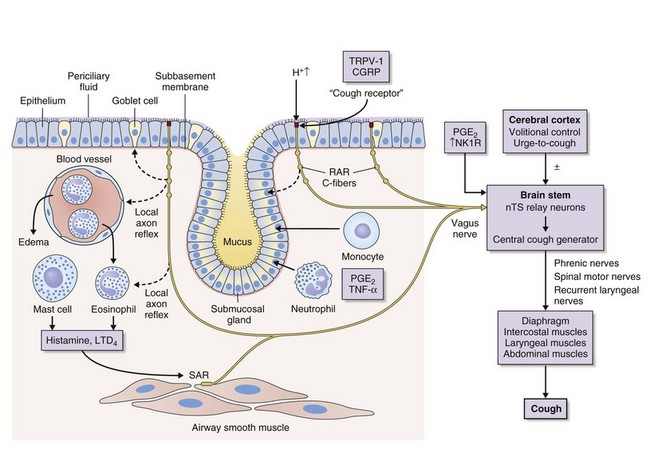
Cough is a reflex that occurs when afferent nerve receptors are stimulated by inhaled, aspirated, or endogenous substances. The most sensitive sites for initiating cough are the larynx, the carina, and the points of bronchial branching. Cough receptors also are present in extrapulmonary structures, including the esophagus, diaphragm, and stomach. A broad group of rapidly adapting “irritant” receptors (RARs) found in the larynx and tracheobronchial tree can be stimulated by a wide range of stimuli, including cigarette smoke, ammonia, ether vapor, acid and alkaline solutions, hypotonic and hypertonic saline, and mechanical stimulation by direct contact, mucus, or dust; all such stimuli can provoke cough. Another closely related fiber is the slowly adapting stretch receptor (SAR), which terminates inspiration and initiates expiration when the lungs are at an adequate level of inflation. SARs also may influence cough. C-fiber receptors, which have thin, nonmyelinated vagal afferent fibers, are found in the laryngeal, bronchial, and alveolar walls. They are relatively insensitive to mechanical stimulation and lung inflation but are exquisitely sensitive to chemicals such as bradykinin, capsaicin, prostaglandins, and acid pH. Stimuli that are known to cause cough in human subjects such as capsaicin, bradykinin, and citric acid activate C-fiber afferents, particularly those located in the bronchi. Afferent nerve fibers pass to a central cough receptor in the medulla, triggering a forced expiratory maneuver against a closed glottis, followed by glottal opening and high-velocity expiration (Figure 18-1).
Differential Diagnosis of Cough
The causes of cough can be conveniently divided into acute and chronic (Box 18-1 and Table 18-1). An acute cough is arbitrarily defined as a cough of less than 3 weeks’ duration. Infectious and allergic conditions are by far the most common etiologic disorders. Most acute coughs related to viral upper respiratory tract infection resolve by 3 weeks, but a small proportion become persistent and require further evaluation.
Most pulmonary conditions implicated in causing chronic cough, such as chronic obstructive pulmonary disease, lung cancer, an inhaled foreign body, pulmonary tuberculosis, sarcoidosis, idiopathic pulmonary fibrosis, and heart failure, will be obvious on clinical assessment, spirometry, and chest radiography. Assessment and management of these conditions are dealt with elsewhere in this book. Thus, a majority of patients referred for investigation of chronic cough are nonsmokers with normal findings on physical examination and chest radiography. Most present with a nonproductive or minimally productive cough, and 60% to 75% are female. A recognized tendency is for cough to manifest initially around the time of menopause. The most common conditions implicated in aggravating or causing chronic cough in these patients are listed in Table 18-1.
Table 18-1 Common Conditions Implicated in Causing Chronic Cough
| Diagnosis | Approximate Incidence (%) |
|---|---|
| Rhinitis | 25-30 |
| Asthma/eosinophilic bronchitis | 20-25 |
| Gastroesophageal reflux | 15-20 |
| Post–viral infection cough | 5-10 |
| Chronic bronchitis | 5-10 |
| Bronchiectasis | 5-10 |
| ACE inhibitor–induced cough | 5-10 |
| Unexplained | 5-20 |
ACE, angiotensin-converting enzyme.
Clinical Assessment
An initial assessment of a patient with chronic cough is directed at finding a specific cause, assessing severity, and initiating trials of treatment. A careful history and physical examination are paramount in the evaluation of a patient with chronic cough (Table 18-2). Details of the factors surrounding the onset of cough and associated symptoms and a careful assessment of the upper airways and the respiratory system are particularly important. Basic initial investigations should include up-to-date chest radiography, spirometry, and tests of bronchodilator reversibility, if appropriate. An abrupt onset of coughing while eating or chewing should raise the possibility of an inhaled foreign body, and the onset of cough shortly after introduction of angiotensin-converting enzyme (ACE) inhibitor therapy suggests ACE inhibitor associated cough. The presence of significant quantities of sputum, hemoptysis, systemic symptoms, prominent breathlessness, wheeze, or abnormal physical signs increases the probability of intrinsic lung disease and should trigger appropriate investigations, which may include a CT scan of the chest and bronchoscopy even in the absence of suggestive findings with more simple investigations. The onset of cough with symptoms suggesting an upper or lower respiratory tract infection raises the possibility of a postinfectious cough; prominent whoops, a very troublesome nocturnal cough, and cough associated with vomiting all are associated with pertussis, a condition that is increasingly recognized in both school-age children and adults. Otherwise, little evidence is available to suggest that information on the timing, nature, complications, and potential aggravating factors is predictive of the underlying cause of the cough.
Table 18-2 Initial Evaluation of the Patient with Chronic Cough
| Evaluation Component | Assessment Factors |
|---|---|
| History | Cough: onset, duration, character, triggers, laryngeal paresthesia |
| Sputum: volume, character | |
| Smoking, occupation | |
| Upper respiratory tract infection | |
| Drug history (ACE inhibitors) | |
| Asthma: breathlessness, wheeze, nocturnal symptoms, atopy | |
| Gastroesophageal reflux: reflux-associated symptoms | |
| Rhinitis: postnasal drip, sinusitis, throat clearing, nasal congestion | |
| Adverse quality of life: musculoskeletal chest pains, incontinence, syncope, social embarrassment, anxiety, disturbed sleep | |
| Snoring | |
| Examination | Clubbing |
| External nasal: polyps | |
| External ears: excessive wax | |
| Oropharyngeal: signs of postnasal drip, tonsillar enlargement | |
| Chest: signs of airflow obstruction, crackles | |
| Investigations | Chest radiograph |
| Spirometry ± bronchodilator reversibility | |
| Serial peak expiratory flow | |
| Complete blood count and eosinophil differential cell count | |
| Optional investigations | Bronchoprovocation challenge test, induced sputum, allergen skin tests |
| Exhaled nitric oxide test | |
| Sinus radiography/sinus CT study | |
| 24-hour esophageal pH and manometry | |
| Chest CT/bronchoscopy in selected patients | |
| Treatment for identified causes | Directed at cause(s) |
ACE, angiotensin-converting enzyme; CT, computed tomography.
Findings on history and physical examination often are unremarkable, in which case the patient evaluation should focus on the recognition of corticosteroid-responsive conditions (i.e., asthma and eosinophilic bronchitis) and extrapulmonary factors that may be aggravating the cough, such as rhinitis and gastroesophageal reflux. One approach to the assessment of patients with chronic cough is outlined in Figure 18-2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree