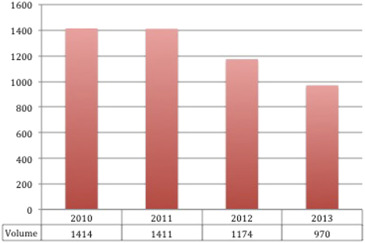
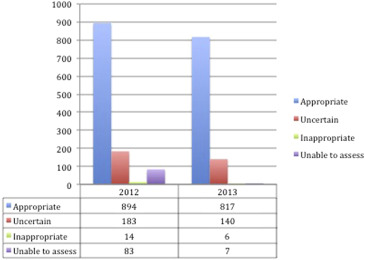
Appropriate use criteria (AUC) for coronary revascularization have been developed to provide a practical standard to assess the quality of patient selection for percutaneous coronary interventions (PCI). However, the economic impact of AUC implementation has yet to be quantified. A peer-reviewed AUC process was implemented at UnityPoint Trinity in February 2012. Volumes of PCI cases were measured in 12-month intervals for 2 years after AUC implementation and compared with volumes from the corresponding 12-month intervals in the 2 years preceding implementation of AUC. Hospital reimbursement was averaged based on each year’s payer mix and reimbursement contracts. In the 2 years preceding AUC implementation, PCI volumes were similar (1,414 in 2010 and 1,411 in 2011). After AUC implementation, volumes of PCI decreased by 17% in both 2012 and 2013. From 2012 to 2013, the relative ratio of elective to acute interventions decreased from 1.36 to 1.02. In the same time frame, the proportion of appropriate PCI significantly increased from 76% to 84% (p <0.001). Total hospital reimbursement for PCI decreased by 36% after AUC implementation. In conclusion, implementation of a peer-reviewed AUC process at the UnityPoint Trinity led to significant cost savings through a large decrease in volume of PCI with concurrent improvement in PCI appropriateness.
In recent years, clinicians and policymakers alike have focused their efforts toward curbing unwarranted costs to the health care system. As the third most expensive procedure for both Medicare and third-party payers, the utilization of coronary interventions has come under increasing scrutiny. Through the collaborative efforts of multiple cardiovascular professional societies, appropriate use criteria (AUC) for percutaneous coronary intervention (PCI) were developed as a practical standard to assess the rational use of coronary revascularization in providing higher quality and potentially more cost-effective care. Although the validity of AUC in improving quality of care for patients with stable coronary artery disease has been established, the economic impact of implementation of AUC has yet to be quantified. We aimed to quantify the economic impact of the AUC by leveraging reimbursement data to longitudinally study the AUC’s effects on volumes of PCI cases at a large community hospital.
Methods
In the AUC, interventions are classified as “appropriate” when the “expected benefits, in terms of survival or health outcomes (symptoms, functional status, and/or quality of life) exceed the expected negative consequences of the procedure.” Interventions classified as “inappropriate” or “rarely appropriate” are considered unlikely to improve health outcomes and may generate unwarranted costs to the health care system. The “uncertain” indication suggests additional factors should be considered or that further research is necessary to define the benefits of treatment.
AUC for coronary revascularization were implemented at the UnityPoint Trinity in February 2012. Volumes of PCI cases were measured in 12-month intervals for 2 years after the implementation of AUC and compared with volumes from the corresponding 12-month intervals in the 2 years preceding implementation of AUC. The relative ratio of acute to elective interventions was also measured. Acute interventions were classified based on 2012 AUC. Over this time period, the number of interventional cardiologists in the hospital did not change, and the total number of patients seen by the cardiologists, in fact, increased.
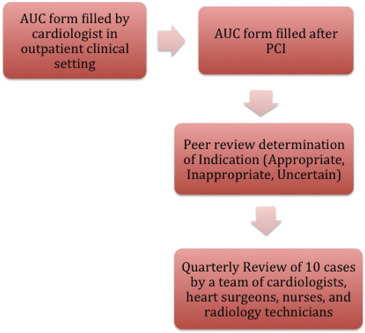
The AUC process implemented at the UnityPoint Trinity begins in the outpatient clinical setting. In the clinic, physicians record the patient’s symptoms, severity of stress test, and antianginal medications on an initial AUC form. The AUC form is transferred to the cardiac catheterization laboratory. After cardiac catheterization, the cardiologist and cardiac staff determine the appropriateness of the intervention and complete the AUC form. If an intervention is performed, the physician fills out another appropriate use form summarizing the procedure. All AUC forms are reviewed monthly by the director of the cardiac catheterization laboratory quality assurance program. Quarterly, 10 cases are peer reviewed ( Figure 1 ).
Hospital reimbursement was averaged based on each year’s payer mix and reimbursement contracts. Reimbursement totals were calculated by multiplying each year’s average hospital reimbursement by the number of procedures performed.
Comparisons of patient characteristics were performed using t test for continuous variables and chi-square test for categorical variables. All analyses were performed using STATA, version 14.0 (StataCorp LP, College Station, Texas), and evaluated at the significance level of 0.05.
Results
In the 2 years preceding implementation of the AUC, the volumes of PCI were similar. After implementation of AUC, the number of PCI decreased to 1,174 (−17%) in 2012 and further to 970 (−17%) in 2013 ( Figure 2 ). Little change in patient demographics and characteristics was observed from 2010 to 2013 ( Table 1 ). The relative ratio of elective to acute interventions decreased from 1.36 to 1.02 after implementation of AUC ( Table 2 , Figure 3 ). The total number of patients seen increased from 75,467 in the 2 years preceding implementation to 91,466 in the 2 years after AUC implementation.
| Variable | Before AUC Implementation (n=2825) | After AUC Implementation (n=2144) | P-value |
|---|---|---|---|
| Men | 57% | 60% | 0.03 |
| Women | 43% | 40% | |
| Age (Years) | |||
| Mean ± SD | 65 ±10 | 65 ±10 | 0.999 |
| Median | 66 | 66 | |
| Medicare Age | 53% | 53% | 0.986 |
| White | 94% | 94% | 0.960 |
| Black | 5% | 5% | |
| Other | 1% | 1% | |
| Non-ST-segment elevation myocardial infarction | 11% | 18% | <0.001 |
| ST-segment elevation myocardial infarction | 5% | 8% | <0.001 |
| Body mass index >30kg/m 2 | 49% | 50% | 0.481 |
| Prior myocardial infarction ( >7 days) | 15% | 17% | 0.060 |
| Prior percutaneous coronary intervention | 33% | 31% | 0.135 |
| Diabetes mellitus | 31% | 32% | 0.452 |
| Current/recent smoker | 22% | 23% | 0.403 |
| Hypertension | 82% | 83% | 0.359 |
| Dyslipidemia | 82% | 73% | <0.001 |
| Prior coronary bypass | 9% | 15% | <0.001 |
| Peripheral arterial disease | 15% | 11% | <0.001 |
| Insurance Payers | |||
| Private | 76% | 82% | <0.001 |
| Medicare | 49% | 51% | 0.165 |
| Medicaid | 7% | 9% | 0.010 |
| None | 2% | 5% | <0.001 |
| 2012 | 2013 | P-value | |
|---|---|---|---|
| Total | 1174 | 970 | |
| Acute | 445 (41%) | 406 (48%) | <0.001 |
| Elective | 607 (59%) | 417 (52%) | |
| Appropriate | 894 (76%) | 817 (84%) | <0.001 |
| Uncertain | 183 (16%) | 140 (14%) | |
| Inappropriate | 14 (1%) | 6 (1%) | |
| Inadequate Assessment | 83 (7%) | 7 (1%) |
| 2011 | 2012 | 2013 | |
|---|---|---|---|
| Average Percutaneous Coronary Intervention Reimbursement | $14,730 | $13,130 | $13,644 |
| Volume of Percutaneous Coronary Interventions | 1,411 | 1,174 | 970 |
| Total Percutaneous Coronary Interventions Reimbursement | $20,784,030 | $15,414,620 | $13,234,680 |
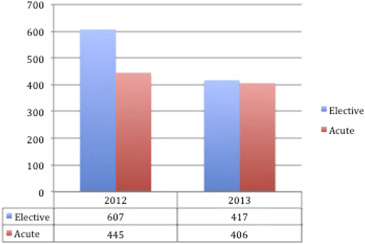
In 2012, the first year after implementation of AUC, 894 interventions (76%) were “appropriate,” 183 interventions (16%) were “uncertain,” 14 interventions (1%) were “inappropriate,” and 83 interventions (7%) were unable to be classified by AUC. In 2013, 817 interventions (84%) were “appropriate,” 140 interventions (14%) were “uncertain,” 6 interventions (1%) were “inappropriate,” and 7 interventions (1%) were unable to be classified by AUC ( Table 2 , Figure 4 ).
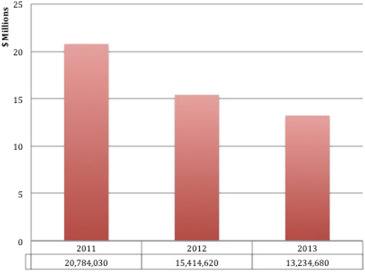
After implementation of the AUC, total hospital reimbursement decreased for PCI cases. Total hospital reimbursement for coronary interventions decreased by 26% from 2011 to 2012 and decreased by a further 14% in 2013. Average hospital reimbursement for interventions decreased by 11% from 2011 to 2012 and slightly increased by 2% from 2012 to 2013 ( Table 3 , Figure 5 ).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


