Coronary Stents
Allen P. Burke, M.D.
Joseph J. Maleszewski, M.D.
Introduction
Percutaneous balloon angioplasty with stenting has become standard treatment for obstructive coronary artery disease, including patients who present with myocardial infarction. Coronary stenting shows similar efficacy for the treatment of coronary artery disease as open surgical procedures.1,2,3,4 In general, bypass is recommended for multivessel or left main disease, and coronary stenting is feasible for either single or multivessel disease. Stents are currently approved for deployment in stenotic segments. Overlapping stents, bifurcating stents, deployment in ostial or left main disease, and use in acute coronary syndromes are considered investigational (“off-label”). Various acronyms have been used for percutaneous interventions (Table 153.1).
Types of Stents
Stents vary by design, composition, and presence of drug. The composition is generally either stainless steel or cobalt chromium; selfexpanding nitinol (nickel titanium alloy) stents are generally used for peripheral vascular disease.
There are three main types of stents currently seen by pathologists: bare metal stents, first-generation drug-eluting stents, and secondgeneration drug-eluting stents. Drug-eluting stents are coated with an antiproliferative drug embedded in a polymer, which elutes from the stent for several months after implantation and decreases the rate of restenosis. First-generation drug-eluting stents included sirolimuseluting and paclitaxel-eluting stents that are composed of stainless steel
struts measuring 130 to 140 µm thick and are similar in design to their bare metal counterparts. Second-generation drug-eluting stents were developed in part to decrease the risk for late stent thrombosis. In the case of first-generation drug-eluting stents, the rate of late stent thrombosis significantly exceeds that of bare metal stents and necessitates long-term antiplatelet therapy.5 Second-generation stents are made of cobalt-chromium, which allows for thinner struts (80 to 90 µm), more rapid endothelialization, and decreased likelihood of thrombosis.6 There are several available second-generation stents: everolimus-eluting cobalt-chromium stent (Xience V and Promus) and a zotarolimuseluting cobalt-chromium stent (Endeavor and Resolute). Randomized clinical trials have shown a reduction in stent thrombosis, myocardial infarction, and rate of repeat intervention (target lesion revascularization) using these new stents compared to first-generation stents.7
struts measuring 130 to 140 µm thick and are similar in design to their bare metal counterparts. Second-generation drug-eluting stents were developed in part to decrease the risk for late stent thrombosis. In the case of first-generation drug-eluting stents, the rate of late stent thrombosis significantly exceeds that of bare metal stents and necessitates long-term antiplatelet therapy.5 Second-generation stents are made of cobalt-chromium, which allows for thinner struts (80 to 90 µm), more rapid endothelialization, and decreased likelihood of thrombosis.6 There are several available second-generation stents: everolimus-eluting cobalt-chromium stent (Xience V and Promus) and a zotarolimuseluting cobalt-chromium stent (Endeavor and Resolute). Randomized clinical trials have shown a reduction in stent thrombosis, myocardial infarction, and rate of repeat intervention (target lesion revascularization) using these new stents compared to first-generation stents.7
TABLE 153.1 Acronyms Associated with Percutaneous Interventions | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Technical Considerations at Autopsy
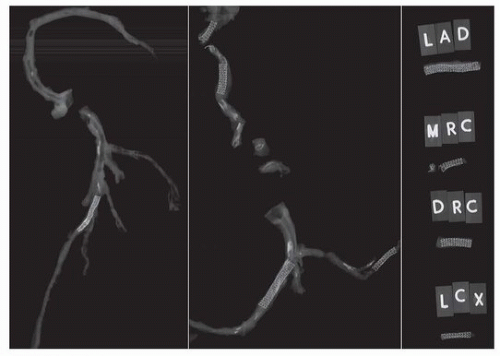
At autopsy, the stented artery is radiographed to determine the location of the stent and degree of intimal calcification and dissected free of the epicardial fat (Fig. 153.1).8 There are three methods of histologic evaluation: removal of stents with diamond scissors, with paraffin embedding; electrolytic dissolution of the stent with paraffin embedding9; and processing in methylmethacrylate and sectioning using special microtomes.10
Paraffin-based methods are preferred for immunohistochemical techniques. Scanning electron microscopy is used in research to examine the extent of endothelialization, although a surrogate for extent of endothelialization is the ratio of uncovered to covered stent struts seen on routine stains.11
In practice, evaluation of the contents of the stent only rarely contributes to the determination of the cause of death.12 However, a registry of stented coronary arteries has led to important discoveries regarding the nature of human restenosis and late stent thrombosis and is available as a resource for pathologists.10
Incidence and Time Course of Restenosis (Neoatherosclerosis)
Autopsy studies that examine stents with various durations of implantation have elucidated the evolution of intimal healing, which, if exaggerated, results in in-stent restenosis, generally caused by neoatherosclerosis or thrombosis.11,13,14,15,16,17,18,19 At autopsy, the rate of restenosis is between 5% and 10%, excluding late stent thrombosis that likely resulted in death.20 No difference was found between the degree of intimal thickening and frequency of neoatherosclerosis between first- and second-generation drug-eluting stents in a different autopsy study.10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree