Fig. 16.1
Two sets of tissue stabilizers applied to the proximal and distal end of the long arteriotomy
A longitudinal arteriotomy is made on the midportion of the diseased LAD, and the incision is extended proximally and distally. The LAD at the level of the most proximal stenotic lesion should not be opened in order to avoid competitive flow, and the distal incision is extended to the non-diseased segment of the LAD. The LITA is longitudinally incised to match the length of the arteriotomy on the LAD. The LITA is then anastomosed to the LAD with several 7-0 or 8-0 polypropylene running sutures to avoid a purse-string effect. The suture lines are placed on the insides of the plaques so as to exclude atheromatous plaques from the lumen of the coronary artery. Care should be taken not to occlude the ostia of the septal perforators and diagonal branches. The majority of the reconstructed lumen finally consists of intact intima of the LITA.
16.2.2 Long Onlay-Patch Grafting with Endarterectomy
Coronary endarterectomy is indicated when the needle cannot pass through severely calcified plaques or there are soft plaques which can be a cause of distal embolism due to plaque rupture. In addition, the techniques of coronary endarterectomy can be applied to long segmental in-stent restenosis after PCI [7]. We perform coronary endarterectomy under direct vision through a long arteriotomy with onlay-patch grafting using the LITA; we do not perform traction endarterectomy for the LAD [8].
The diseased LAD is incised in its midportion, and the incision is extended proximally and distally. The atheromatous core is carefully dissected from the adventitia using a fine spatula and forceps. All the side branches are directly observed, and their intima is carefully dissected and removed with the atheromatous core (Fig. 16.2). To avoid flow competition between the LITA and the native coronary artery, the most proximal stenotic lesion should not be removed. The distal end of the atheromatous core is sharply divided at the level of intact intima, and the divided intima is then tacked with an 8-0 polypropylene running suture. The surface of the endarterectomized LAD is flushed with saline solution, and the residual intimal flaps or fragments of plaques are completely removed. Thereafter, the skeletonized LITA is incised longitudinally and anastomosed to the LAD with several 8-0 polypropylene running sutures. As in the plaque exclusion technique, care should be taken not to occlude the ostia of the septal perforators and diagonal branches, and the majority of the reconstructed lumen consists of intact intima of the LITA (Fig. 16.3).
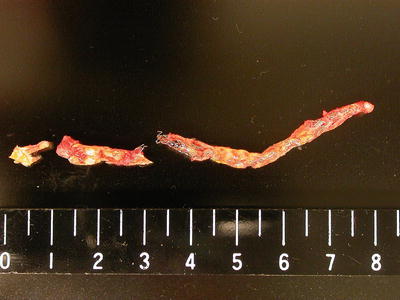
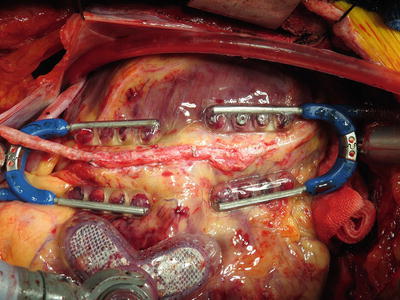
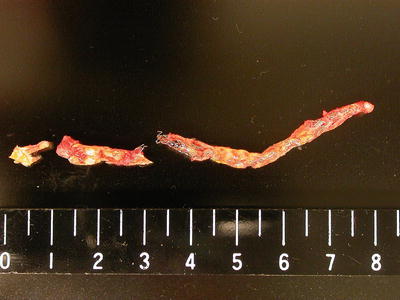
Fig. 16.2
Endarterectomized core (with restenosed coronary stents) demonstrating proper tapering of side branches
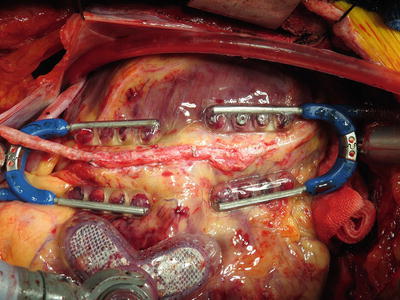
Fig. 16.3
Endarterectomized left anterior descending artery reconstructed using skeletonized left internal thoracic artery graft with an onlay-patch fashion
16.3 Postoperative Management of Coronary Endarterectomy
Unlike conventional distal grafting to the non-diseased segment, long onlay-patch grafting with or without endarterectomy for a diffusely diseased coronary artery requires a direct manipulation of a diseased coronary artery: therefore, there are several pitfalls specific to these procedures. Of those, acute thrombotic occlusion of the endarterectomized vessel is the most disastrous complication after coronary endarterectomy [9]. The lack of endothelium in the endarterectomized vessel leads to the exposure of subendothelial tissue to the bloodstream, which results in the triggering of the coagulation cascade and thrombus formation in the endarterectomized vessel. In order to prevent acute thrombosis after endarterectomy, aggressive anticoagulation treatment in combination with antiplatelet therapy is mandatory. However, to date, there have been no published guidelines or protocols describing optimal antiplatelet or anticoagulation therapy for patients undergoing coronary endarterectomy. In our institute, postoperative anticoagulant and antiplatelet treatment is performed with the following protocol: intravenous infusion of low-molecular-weight heparin (5,000 units/day) is initiated after chest tube output has decreased and continued until warfarin is effective. Low-dose aspirin (100 mg/day), clopidogrel (75 mg/day), and warfarin (maintained with a target international normalized ratio of 2.0) are started after the initiation of oral intake. Warfarin and clopidogrel are discontinued after 3 months and 1 year after surgery, respectively, but aspirin is continued indefinitely.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


