Coronary CTA: Display Techniques and Planes
Karen G. Ordovas
Maria Clara N. Lorca
Charles B. Higgins
INTRODUCTION
Although most of the findings on coronary computed tomography angiography (CTA) can be identified on axial images of the heart, the use of different reformation techniques can be helpful for diagnosis and for determining severity of coronary stenoses (1). In addition, reformations can be very useful when the relationship between the coronary arteries and the adjacent mediastinal structures must be defined.
The acquisition of isotropic or near-isotropic voxels with multidetector CT allows for precise visualization of the images through reformations in innumerable planes (2).
An organized approach for evaluation of coronary imaging studies is essential for optimization of the interpretation sessions. The selection of postprocessing tools should be tailored to each specific case, with the ultimate goal to address the main clinical question. Review of the axial images is very helpful to identify possible coronary lesions and to guide an optimal approach to a time-efficient evaluation of the studies (2). Clinical-based strategies for the postprocessing of cardiac imaging studies will be discussed in this chapter.
SELECTING THE BEST DATASET TO PERFORM THE RECONSTRUCTIONS
When performing postprocessing for visualization of the coronary arteries and cardiac structures, it is important to define what dataset has the least amount of cardiac motion artifact affecting the structures of interest. Prior coronary CTA studies have described that the ideal phase of the cardiac cycle for visualization of the coronary arteries vary. Choi et al. (3) have shown that the best phase for right coronary artery depiction is approximately 40% to 45% of the R-R interval, whereas 70% of the cycle is the ideal phase for the left coronary system. When the heart rate is below 60 to 65 bpm, usually 70% to 75% of the R-R interval provides good image quality for visualization of all the coronary segments. In some cases, particularly when the heart rate is elevated, review of multiple cardiac phases is needed to accomplish interrogation of the entire coronary tree without motion artifacts.
Selection of a specific phase of the R-R interval for imaging reconstruction is also necessary when cardiac valves are being evaluated. For evaluation of valvular stenosis, reformations are ideally obtained throughout the cardiac cycle, but the maximum opening of the valvular orifice will be depicted during end-systole for the aortic valve and end-diastole for the mitral valve.
AN OVERVIEW OF THE MOST COMMON POSTPROCESSING TOOLS AND ITS CLINICAL UTILITIES
MULTIPLANAR RECONSTRUCTION
Multiplanar reconstruction (MPR) is typically used in an interactive way, allowing the imager to navigate through sagittal, coronal, axial, and the several planes oriented to the heart itself rather than the thorax. This technique can be understood as a two-dimensional slab of the three-dimensional dataset. Although this technique provides flexibility for understanding the spatial relationship of the cardiac chamber, great vessels, and other mediastinal structures, it is somewhat limited for evaluation of long and tortuous vascular segments such as the coronary arteries. Short and nontortuous segments of the coronary arteries can be well evaluated with MPR (4).
The most useful applications of MPR are in cases where the relationship of the coronary arteries and the great vessels
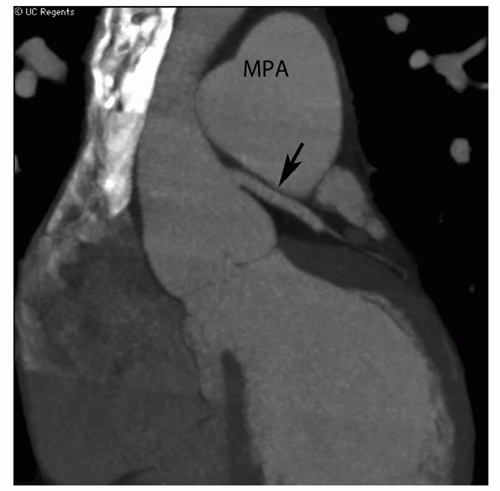
and chest wall structures must be examined. A common clinical indication for coronary CTA is visualization of coronary bypass grafts and its relationship to the sternum in patients undergoing reoperation, with the goal of avoiding graft injury during sternotomy (5). MPR in the sagittal plane can typically depict the relationship of anterior venous grafts or internal mammary grafts to the inner face of the sternum (Fig. 8.1). Another clinical scenario suitable for MPR reformation is the investigation of coronary artery compression by adjacent structures, such as paracardiac masses or dilated pulmonary arteries in patients with pulmonary hypertension (Fig. 8.2).
and chest wall structures must be examined. A common clinical indication for coronary CTA is visualization of coronary bypass grafts and its relationship to the sternum in patients undergoing reoperation, with the goal of avoiding graft injury during sternotomy (5). MPR in the sagittal plane can typically depict the relationship of anterior venous grafts or internal mammary grafts to the inner face of the sternum (Fig. 8.1). Another clinical scenario suitable for MPR reformation is the investigation of coronary artery compression by adjacent structures, such as paracardiac masses or dilated pulmonary arteries in patients with pulmonary hypertension (Fig. 8.2).
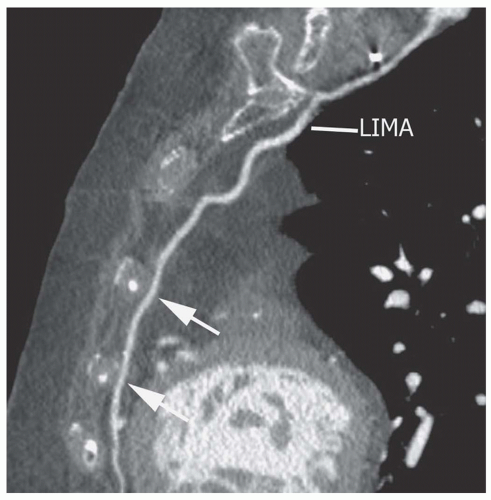 Figure 8.1. Multiplanar reconstruction of a left internal mammary (LIMA) graft (arrows) in a parasagittal plane displays the relationship of the graft with the inner surface of the sternum. |
MPR is the most suitable method for visualization of cardiac anatomy and function. For assessment of regional cardiac contractility, three standard cardiac planes are typically used for MPR reformats. The horizontal long-axis plane, also called four-chamber plane, is aligned to the long axis of the heart, and displays the four cardiac chambers, the mitral and tricuspid valves and the atrial and ventricular septum in alignment. The vertical long-axis plane, also called two-chamber plane, can be obtained from the four-chamber plane by prescribing a plane between the left ventricular apex and the center of the mitral valve. Finally the short-axis plane is prescribed perpendicular to the horizontal long-axis plane (Fig. 8.3).
Most postprocessing softwares offer a tool for automatic depiction of the standard cardiac planes. In retrospectively gated cardiac studies, a cine loop in the standard cardiac planes allows for a comprehensive depiction of global and regional left ventricular wall motion. In addition, volumetric analysis can be performed using the Simpson’s method for quantification of end-diastolic volume, end-systolic volume, and ejection fraction of both ventricles.
MPR is also the best technique for assessment of valvular function. In general, CTA is useful for evaluation of valvular morphology and function, especially when retrospective cardiac gating is obtained and cine loops can be played encompassing the entire cardiac cycle. This approach allows for visualization of leaflet excursion, particularly in the setting of aortic or mitral stenosis. For interrogation of the aortic valve, MPR reformat is obtained aligned parallel to the left ventricular outflow tract and proximal ascending aorta, which allows for visualization of the leaflet thickness and excursion and poststenotic dilatation of the ascending aorta (Fig. 8.4A). An orifice view, which is parallel to and at the level of the valvular annulus, can be useful for measurement of maximum opening at end-systole (Fig. 8.4B). Similarly, MPR in the two-chamber view is optimal for visualization of mitral valve leaflet excursion. Although rarely an indication for cardiac CTA, evaluation of the pulmonary and tricuspid valves can also be obtained by aligning the MPR parallel to the outflow and inflow of the right ventricle respectively.
 Get Clinical Tree app for offline access 
|


