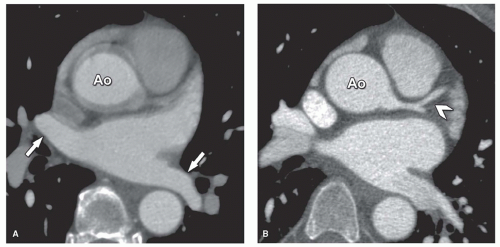
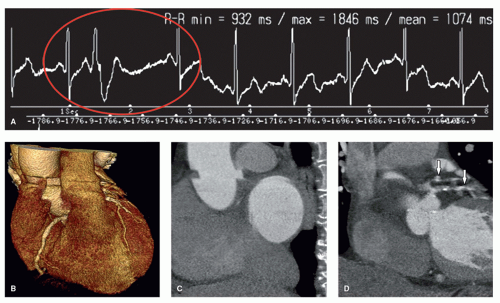
coronary CT angiography are CT-dependent technical limitations in spatial and temporal resolution. Partial volume effect and beam hardening cause blooming artifacts especially in the presence of severe calcifications that hamper evaluation of the coronary artery lumen. Motion artifacts can be caused by postural motion (e.g., if the patient cannot hold the breath), by high heart rates that result in too short coronary rest-phase for motionless imaging, and by arrhythmia (causing reconstruction artifacts, Fig. 25.5) (16,17). The problems of arrhythmia can be overcome by fast coverage of the entire cardiac volume within a single heartbeat (Fig. 25.6). Arrhythmia rejection performed prospectively by the CT scanner is helpful to improve image quality while reducing effective dose as compared to retrospective gating techniques. Improving the coverage of coronary CT angiography and single heartbeat scanning can be done using either 320-row volume or fast dual-source CT (Fig. 25.7).
Table 25.1 Diagnostic Accuracy of Coronary CT Angiography on the Per-Patient Level | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
64-row cardiac CT. Bolus tracking is most often used for initiating the scan after contrast agent injection (Fig. 25.8) (11). Alternatively, test bolus injection can be used to identify the optimal scan point but requires a slightly higher contrast agent volume (i.e., that of the test bolus itself). Bolus tracking is performed during the actual scan and thus has less variability. By using single-beat cardiac CT, the contrast agent volume can be further reduced in comparison to multi-beat 64-row CT. Further reductions in contrast agent volume can be achieved using fast bolus tracking approaches available with single-beat imaging.
The flow and contrast agent amount is adjusted to the individual patient weight to unify image quality.
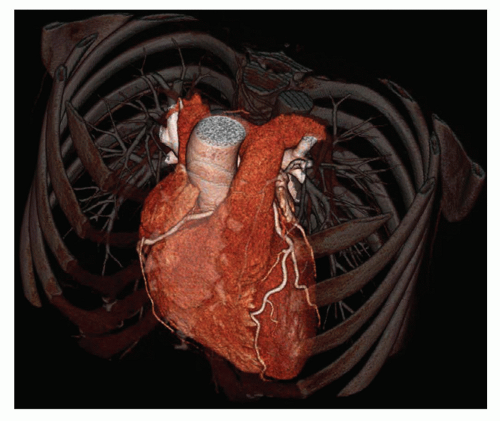
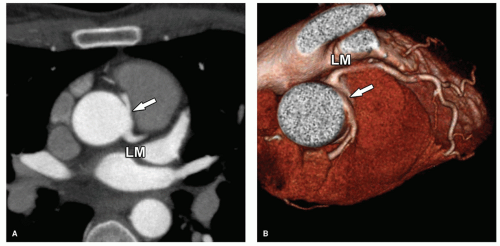
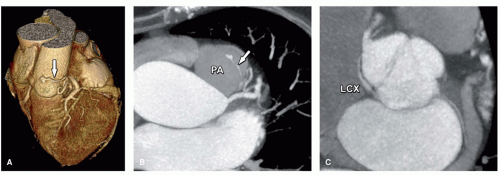
 Figure 25.6. Successful arrhythmia rejection with 320-row CT (arrow, A) in a 49-year-old female patient with suspected coronary artery disease and irregular heart rate. Issues in patients with irregular heart rates shown in Figure 25.5 can be overcome using single-beat scanning of the entire heart with prospective triggering and arrhythmia rejection that allows for sharp imaging of the coronary arteries (B-D
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|