Conventional coronary angiography (CCA) has considerable limitations regarding visualization of distal vessel segments in chronic total occlusion. We assessed the ability of coronary computed tomographic angiography (CCTA) to predict the success of coronary artery bypass grafting (CABG) to the chronically occluded left anterior descending coronary artery (LAD) incompletely visualized on CCA. Thirty symptomatic patients rejected for CABG on the basis of the CCA findings underwent preoperative CCTA before intended transmyocardial laser revascularization. The LAD was explored operatively in all patients, and CABG to the LAD was attempted if the distal vessel was suitable for anastomosis. The procedural outcome of CABG and the 6-month patency of the left internal mammary artery graft at follow-up CCTA were defined as the primary and secondary end point, respectively. The primary and secondary end points were achieved in 80% and 77% of patients, respectively. We found a significant correlation between the intraoperative and computed tomographic measurement of distal LAD diameter (R = 0.428, p = 0.037). On multivariate analysis, the maximum diameter of the distal LAD by CCTA (odds ratio 8.16, p = 0.043) was the only independent correlate of procedural success of CABG. A cutoff value of 1.5 mm for the mean distal LAD diameter predicted left internal mammary artery graft patency with 100% specificity and 83% sensitivity. Successful CABG resulted in significant improvements in angina class and left ventricular function in LAD segments at 6 months of follow-up. In conclusion, CCTA predicted both the procedural and the intermediate outcome of CABG to chronic LAD occlusion with failed visualization on CCA.
Although conventional coronary angiography (CCA) is an approved method for referral for coronary artery bypass grafting (CABG), it has considerable limitations related to visualization failure of distal vessel segments in coronary occlusions when the vessel is observed intraoperatively. The aim of the present study was to determine the ability of coronary computed tomographic angiography (CCTA) to predict both the procedural and the intermediate-term result of CABG to the chronically occluded left anterior descending coronary artery (LAD) with failed visualization on CCA.
Methods
We included 30 consecutive patients with chronic LAD occlusion who were deferred from CABG owing to failure of visualization of the distal LAD by CCA and were therefore scheduled for transmyocardial laser revascularization (TMLR). LAD occlusion was estimated to be of ≥3-months duration from either a history of myocardial infarction, previous chest pain, or the interval from previous CCA. All patients had effort angina refractory to maximum medical therapy, positive electrocardiographic stress test findings, preserved contractility at rest echocardiography, and/or documented viability of the anterior wall on single photon emission computed tomographic scan. For the specific purpose of the present study, all patients underwent preoperative CCTA and CABG to the LAD with in vivo measurement of the distal LAD diameter was attempted before TMLR. According to the procedural outcome of CABG to the LAD, the patients were assigned to either the CABG or TMLR group. Additionally, follow-up CCTA was performed in the CABG group to assess the patency of the left internal mammary artery to the LAD graft and the changes in left ventricular function ≥6 months after surgery. The procedural success of CABG and intermediate patency of the internal mammary graft were defined as the primary and secondary end point, respectively. The exclusion criteria were a fixed perfusion defect of the anterior wall on a single photon emission computed tomographic scan, an inability to hold a breath for 15 seconds, and a serum creatinine level of >2.0 mg/dl. The institutional ethics committee approved the study, which was in accordance with the second Declaration of Helsinki. All patients provided informed consent.
Coronary angiography was performed using a standard angiography system (Axiom Artis, Siemens, Forchheim, Germany). Standard views with ≥5 different projections for the left coronary artery and 2 projections for the right coronary artery with prolonged cineangiography were obtained. The LAD was judged inoperable by 2 highly experienced cardiac surgeons owing to failure of visualization of the distal vessel by CCA. Similarly, a high SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) score, unfavorable angiographic features of the LAD occlusion site, or a history of failed LAD revascularization resulted in deferral from percutaneous intervention. Coronary angiograms were evaluated retrospectively by a single experienced cardiologist who was unaware of the results of CCTA and the intraoperative findings. The presence of coronary artery disease was assessed according to the 16-segment modified American Heart Association classification. Narrowings of ≥50% luminal obstruction were considered significant, and the SYNTAX score was determined for each patient. Chronic total occlusion was defined as complete coronary occlusion by CCA with no antegrade filling of the distal vessel other than through collaterals. The following characteristics of the LAD occlusion site were reported: presence of multiple occlusion sites, severe tortuosity (≥1 angle ≥90), blunt stump, side branch, heavy calcium (opacifications surrounding the complete lumen of the coronary artery), and antegrade flow by bridging collaterals. Additionally, the presence of a distal LAD intramyocardial course and grading of the coronary collaterals according to the Rentrop criteria (0, no filling of collaterals; 1, filling of collaterals without reaching the epicardial artery; 2, partial filling of the epicardial artery; and 3, complete filling of the epicardial artery) were assessed.
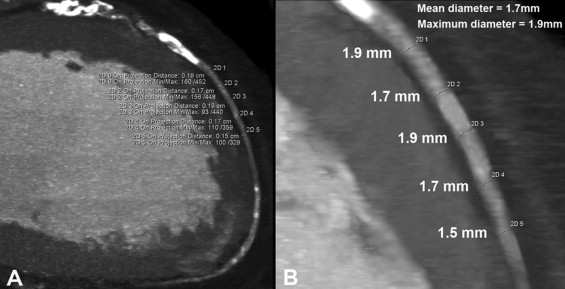
CCTA was acquired using a dual-source computed tomographic scanner (Somatom Definition, Siemens Healthcare, Forchheim, Germany) after sublingual administration of nitrates. An electrocardiogram-gated retrospective protocol was used with 100- to 120-kV tube voltage. For acquisition of the volume data set, 80 to 120 ml of contrast material (Iomeron 400, Bracco Altana Pharma, Konstanz, Germany) was administered. The scanning range of the postoperative CCTA covered the entire course of the left internal mammary graft. The scan data were reconstructed routinely in mid- to end-systole and diastole, and the slice thickness was 0.6 mm. Using the guidelines on quality criteria in computed tomography, the estimated effective radiation dose was 12 and 20 mSv for the preoperative and postoperative computed tomographic scans, respectively. All images were analyzed on a dedicated workstation (Leonardo Workstation, Siemens, Erlangen, Germany) by a single experienced cardiologist unaware of the results of CCA and the surgical procedure. In addition, analysis of the distal LAD diameter was performed by 2 independent observers to assess interobserver variability. The presence of multiple occlusion sites, defined as complete interruption of the contrast opacification separated by contrast-enhanced segments of ≥5 mm, was determined. The following characteristics of the distal LAD were reported: significant coronary artery disease (≥50% luminal obstruction), diffuse disease, any calcium, intramyocardial course (superficial or deep according to the depth of the intramuscular segment of <1 or ≥1 mm, respectively), length of the contrast-enhanced vessel segment, and distal diameters of a vessel lumen. The mean diameter of the distal LAD was calculated as the average of 5 measurements at 0.5-cm intervals at the level of an attempted anastomotic site, and the maximum diameter of the distal LAD was defined as the maximum value of those 5 measurements ( Figure 1 ). The presence of coronary collaterals to the LAD was graded according to the Rentrop criteria, as previously described. The postoperative computed tomographic data sets were assessed for the presence of left internal mammary graft patency, defined as uninterrupted contrast opacification at any graft location with complete filling of the distal LAD. The analysis of preoperative and postoperative left ventricular function was performed using dedicated software (QMass CT, version 6.2, Medis, Leiden, The Netherlands), as previously described. For assessment of regional function, the left ventricle was divided according to the American Heart Association segmentation model, and the myocardial segments (basal anterior, basal anteroseptal, mid anterior, mid anteroseptal, apical anterior and apical septal) in the vascular distribution of the LAD were analyzed.
All cardiac surgeries were performed by the same chief surgeon. The range of the surgical procedure was planned on the basis of the findings from CCA with the intention of complete coronary revascularization. If CABG to LAD was available, the TMLR procedure was abandoned. The chest was opened through a median sternotomy followed by a thorough examination of the anterior aspect of the heart. If a distal LAD was found, the anastomotic site was dissected, and the internal LAD diameter was measured by inserting dilator probes of 1.0 and 1.5 mm distally and proximally to the level of an attempted anastomotic site. On a beating heart, an anastomosis between the left internal mammary artery and the LAD, and revascularization of non-LAD arteries were performed. If the examination failed to reveal a visible or patent distal segment of the LAD, TMLR, using the carbon dioxide Heart Laser System (PLC Medical Systems, Milford, Massachusetts) in target areas of the left ventricular anterior wall, was performed.
Continuous data with a normal distribution are reported as the mean ± SD. A 2-tailed paired-sample t test, Mann-Whitney U test, or Wilcoxon signed-rank test were used to assess the differences between continuous variables. Differences in categorical data were analyzed by the Fisher exact test. The correlation of continuous variables was assessed with the Spearman test. The diagnostic accuracy for the prediction of the study end points was determined by receiver operating curve analysis. Provided that failure of CABG should not improve myocardial perfusion, and according to the intention-to-treat analysis, the TMLR patients were primarily regarded as those with an occluded arterial graft in the secondary end point analysis. All covariates were modeled univariately and multivariately using a single-step procedure in a logistic regression model. The intraclass correlation coefficient for continuous variables was used to assess interobserver variability. Statistical analysis was performed with SPSS, version 15.0 (SPSS, Chicago, Illinois).
Results
From March 2008 to December 2010, 30 patients were enrolled. The baseline clinical and angiographic characteristics are listed in Table 1 . Most patients (77%) presented with Canadian Cardiovascular Society class III to IV angina. In all 16 patients with any left ventricular dysfunction, the viability of the anterior wall was documented with left ventricular ischemia of 13 ± 7% on single photon emission computed tomographic scanning. The LAD characteristics are listed in Table 2 . CCA failed to visualize the distal LAD in 9 patients (30%), and partial filling of the short portion of the distal LAD was seen in 21 patients (70%). By CCTA, some contrast-enhanced segment of the distal LAD (Rentrop ≥2) was visualized in all patients. Compared to CCA, complete filling of the distal LAD (Rentrop 3) was shown more frequently by CCTA (p <0.001). In contrast to CCA, CCTA identified 8 patients with multiple LAD occlusion sites (p = 0.005) and 9 patients with an intramyocardial course of the distal LAD (p = 0.002). The interobserver variability was 0.95 and 0.94 for computed tomographic measurements of the mean and maximum LAD diameters, respectively.
| Variable | Value |
|---|---|
| Age (years) | 65.1 ± 8.1 |
| Men | 21 (70%) |
| Diabetes mellitus | 9 (30%) |
| Hypertension ⁎ | 27 (90%) |
| Hypercholesterolemia † | 22 (73%) |
| Family history of coronary artery disease | 17 (57%) |
| Current smoker | 6 (20%) |
| Peripheral vascular disease | 6 (20%) |
| Previous myocardial infarction | 18 (60%) |
| Previous percutaneous coronary intervention | 14 (47%) |
| Failed percutaneous revascularization of LAD | 8 (27%) |
| Stable angina pectoris | 30 (100%) |
| Canadian Cardiovascular Society angina class | 3.0 ± 0.7 |
| New York Heart Association class | 1.2 ± 0.4 |
| Left ventricular ejection fraction (%) | 49.6 ± 8.9 |
| >50% | 16 (53%) |
| 40–50% | 11 (37%) |
| <40% | 3 (10%) |
| Body mass index (kg/m 2 ) | 29.5 ± 4.1 |
| EuroSCORE (%) | 3.6 ± 3.4 |
| SYNTAX score | 42.6 ± 10 |
| Number of narrowed coronary arteries ‡ | |
| 1 | 1 (3%) |
| 2 | 5 (17%) |
| 3 | 18 (60%) |
| Left main | 6 (20%) |
| Totally occluded major coronary arteries | |
| 1 | 21 (70%) |
| 2 | 8 (27%) |
| 3 | 1 (3%) |
⁎ Defined as history of hypertension (systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg) diagnosed and/or treated with medication or currently treated by diet and/or medication by a physician.
† Included previously documented diagnosis of hypercholesterolemia (serum total cholesterol ≥230 mg/dl or serum triglycerides ≥200 mg/dl) or treatment with lipid-lowering drugs.
‡ Defined as ≥50% luminal obstruction by visual assessment at coronary angiography.
| Angiographic characteristics of LAD | |
| In-stent occlusion | 4 (13%) |
| Multiple occlusion | 0 |
| Severe tortuosity | 2 (7%) |
| Side branch at occlusion | 27 (90%) |
| Blunt stump | 18 (60%) |
| Heavy calcium at occlusion | 12 (40%) |
| Mean Rentrop grade | 1.7 ± 0.5 |
| 0–1 | 9 (30%) |
| 2 | 21 (70%) |
| 3 | 0 |
| Bridging occlusion | 9 (30%) |
| Antegrade collateral filling | 17 (57%) |
| Retrograde collateral filling | 16 (53%) |
| Intramyocardial course | 0 |
| CCTA characteristics of LAD | |
| Multiple occlusion | 8 (27%) |
| Double occlusion | 6 (20%) |
| Triple occlusion | 2 (7%) |
| Occlusion length (mm) | 26.8 ± 22 |
| Calcium at occlusion | 23 (77%) |
| Mean Rentrop grade | 2.9 ± 0.3 |
| 0–1 | 0 |
| 2 | 4 (13%) |
| 3 | 26 (87%) |
| Distal LAD length (mm) | 91.7 ± 24.8 |
| Termination proximal to apex | 4 (13%) |
| Termination distal to apex | 26 (87%) |
| Distal LAD mean diameter (mm) | 1.6 ± 0.2 |
| Distal LAD maximum diameter (mm) | 1.7 ± 0.2 |
| Distal LAD obstructive disease ⁎ | 6 (20%) |
| Distal LAD diffuse disease | 3 (10%) |
| Distal LAD calcium | 17 (57%) |
| Distal LAD intramyocardial course | 9 (30%) |
| Superficial intramyocardial course | 4 (13%) |
| Deep intramyocardial course | 3 (10%) |
⁎ Defined as ≥50% luminal obstruction by visual assessment on coronary computed tomographic angiography.
The primary end point was achieved in 24 patients (80%; Figure 2 ). We found a moderate correlation between the intraoperative and computed tomographic measurement of the mean distal LAD diameter (R = 0.428, p = 0.037) in these patients (CABG group). In the remaining 6 patients (20%), TMLR accompanied by CABG to non-LAD arteries was done (TMLR group; Figure 3 ). The interval between CABG and follow-up CCTA was 18 ± 12 months (range 6 to 34). Follow-up CCTA revealed 1 occluded internal mammary artery graft that was anastomosed to the LAD of 1 mm diameter, as assessed intraoperatively. Thus, the secondary end point was achieved in 23 patients (77%).




