Patients with psoriasis may have an increased risk of cardiovascular disease and myocardial infarction. The aim of this study was to investigate whether psoriasis is associated with an increased prevalence of coronary artery disease (CAD) independent of established cardiovascular risk factors in patients undergoing coronary angiography. A retrospective cohort analysis was performed by linking records of all patients undergoing coronary angiography from 2004 through 2009 with dermatology medical records. From an overall cohort of 9,473 patients, we identified 204 patients (2.2%) with psoriasis before coronary angiography. Patients with psoriasis had higher body mass index (31.3 ± 8.1 vs 29.3 ± 7.1 kg/m 2 , p <0.001) but the prevalence of other risk factors was similar. Median duration of psoriasis before cardiac catheterization was 8 years (interquartile range 2 to 24). Patients with psoriasis were more likely to have CAD (84.3% vs 75.7%, p = 0.005) at coronary angiography. After adjusting for established cardiovascular risk factors, psoriasis was independently associated with presence of angiographically confirmed CAD (adjusted odds ratio 1.8, 95% confidence interval 1.2 to 2.8, p = 0.006). In patients with psoriasis, duration of psoriasis >8 years was also independently associated with angiographically confirmed CAD after adjusting for established cardiovascular risk factors (adjusted odds ratio 3.5, 95% confidence interval 1.3 to 9.6, p = 0.02). In conclusion, patients with psoriasis and especially those with psoriasis for >8 years have a higher prevalence of CAD than patients without psoriasis undergoing coronary angiography.
No study to date has systematically examined the presence of coronary artery disease (CAD) in patients with psoriasis undergoing coronary angiography. In this study we linked cardiac catheterization data with clinical data on patients with psoriasis. By creating this unique database, we were able to examine whether psoriasis is independently associated with angiographically confirmed CAD in patients undergoing coronary angiography.
Methods
We identified all patients who underwent cardiac catheterization at the University of California, Davis from 2004 through 2009. This database contains prospective data entered at the time of cardiac catheterization including patient risk factors, medical history, and quantitative results of coronary angiography. Patients were included if they were ≥18 years of age and had undergone coronary angiography from 2004 through 2009. This study was approved by the University of California, Davis, institutional review board.
To identify psoriatic patients within the catheterization database, we first obtained a list of patients from the University of California, Davis, Medical Center electronic health records with a diagnostic code of psoriasis before 2009. This list was then cross-referenced with the cardiac catheterization database list to identify those patients with possible psoriasis who underwent cardiac catheterization. To confirm the presence of physician-diagnosed psoriasis in these patients and to further identify other patients with psoriasis who may have received care elsewhere, all patients who underwent cardiac catheterization during the study period were then contacted by telephone and asked to complete a brief survey on their psoriasis status. Based on the medical record reviews and telephone surveys, 204 patients had been diagnosed with psoriasis before cardiac catheterization.
Risk factors for CAD, age, self-reported ethnicity, and insurance status were prospectively entered at the time of cardiac catheterization. At the time or coronary angiography, a cardiologist determined the severity of CAD for the left main, left anterior descending, left circumflex, and right coronary arteries. If there were multiple lesions present in a single coronary artery territory, the most severe stenosis was recorded. Any CAD was defined as any stenosis scored visually at the time of coronary angiography. Obstructive CAD was defined as stenosis ≥50% in the left main coronary artery or ≥70% in other coronary territories to reflect the presence of more severe lesions for which percutaneous coronary intervention or coronary artery bypass grafting is usually considered.
Psoriasis disease severity was considered mild if a patient had a history of using only topical medications for treatment of psoriasis and moderate-to-severe if a patient had received phototherapy or systemic medications (including oral and biologic medications). These categories were chosen because they reflect clinically meaningful differences in psoriasis disease severity.
Mean ± SD was used to describe continuous variables and numerical counts (percentages) were used for categorical variables. Univariate analysis using t test or chi-square test was used to identify differences between subjects with or without psoriasis at the time of coronary angiography. A p value <0.05 was considered statistically significant for all analyses.
First, univariate logistic regression was used to determine the unadjusted relation (odds ratio [OR]) between predictor variables and angiographically confirmed CAD. A multivariate logistic regression model was then constructed using angiographically confirmed CAD as the outcome. Known risk factors for CAD (including age, diabetes, BMI, hypertension, hypercholesterolemia, peripheral vascular disease, family history of CAD) were automatically included. Second, a list of possible confounders was generated using a directed acyclic graph. Confounders from this second group were retained if they were found to be associated with the outcome using a p value <0.1 as a cutoff for inclusion. A manual stepwise elimination algorithm was then used. Covariates in the final model included age, ethnicity, gender, body mass index, history of diabetes, cerebrovascular disease, peripheral vascular disease, hypertension, smoking status, previous myocardial infarction, hypercholesterolemia, previous coronary bypass, and family history of CAD. A secondary analysis was also performed in patients with psoriasis to examine the association between moderate-to-severe psoriasis and history of myocardial infarction. Hosmer–Lemeshow goodness-of-fit testing was used to confirm model discrimination for all models. All statistical analysis was performed using STATA 11 (STATA Corp., College Station, Texas).
Results
From a total population of 9,473 patients who underwent coronary angiography, we identified 204 patients (2.2% of overall population) who had psoriasis before coronary angiography ( Table 1 ). Compared to the overall population, patients with psoriasis had a higher body mass index (31.3 ± 8.1 vs 29.3 ± 7.1 kg/m 2 , p <0.001) and were more likely to have a history of hypercholesterolemia (72% vs 66%, p = 0.06). Eighteen percent of patients with psoriasis had previous myocardial infarction and 45% of patients with psoriasis presented with an acute coronary syndrome.
| Variable | Psoriasis | p Value | |
|---|---|---|---|
| Yes (n = 204) | No (n = 9,265) | ||
| Age (years) | 61 ± 13 | 61 ± 12 | 0.9 |
| Men | 120 (59%) | 5,499 (60%) | 0.7 |
| Body mass index (kg/m 2 ) | 31 ± 8 | 29 ± 7 | <0.001 |
| Race/ethnicity | |||
| White | 164 (80%) | 6,227 (67%) | 0.003 |
| Hispanic | 11 (5.4%) | 823 (8.9%) | |
| African-American | 16 (7.8%) | 1,141 (12%) | |
| Asian | 10 (4.9%) | 708 (7.7%) | |
| Other | 3 (1.5%) | 351 (3.8%) | |
| Previous myocardial infarction | 37 (18%) | 1,991 (22%) | 0.2 |
| Hypertension | 158 (78%) | 6,811 (75%) | 0.3 |
| Current or previous smoker | 118 (62%) | 4,962 (58%) | 0.3 |
| Diabetes mellitus | 61 (31%) | 2,826 (32%) | 0.7 |
| Stroke | 27 (13%) | 1,022 (11%) | 0.4 |
| Renal failure | 7 (11%) | 680 (20%) | 0.2 |
| Peripheral vascular disease | 19 (9.5%) | 781 (8.7%) | 0.7 |
| Hypercholesterolemia ⁎ | 145 (72%) | 5,942 (66%) | 0.06 |
| Heart failure | 38 (19%) | 1,818 (20%) | 0.6 |
| Family history of coronary artery disease | 39 (19%) | 1,478 (16%) | 0.3 |
| Previous coronary bypass | 22 (11%) | 1,140 (13%) | 0.5 |
| Presentation symptoms | 0.8 | ||
| Stable angina pectoris | 105 (55%) | 4,760 (55%) | |
| Acute coronary syndrome † | 87 (45%) | 3,820 (45%) | |
⁎ Defined as any history of medical treatment for increased cholesterol levels.
† Defined as presentation with unstable angina or myocardial infarction.
Patients with psoriasis were more likely to have any CAD on coronary angiogram (OR 1.7, p = 0.005; Table 2 ), with a larger percentage of patients having left anterior descending coronary artery disease (78% vs 67%, p = 0.002). After adjusting for established cardiovascular risk factors, psoriasis remained independently associated with presence of any CAD on coronary angiogram (adjusted OR [AOR] 1.8, 95% confidence interval [CI] 1.2 to 2.8, p = 0.006; Table 3 ). The independent association of psoriasis with presence of any CAD remained significant when analysis was limited only to patients presenting with stable angina pectoris (AOR 1.9, 95% CI 1.2 to 3.1, p = 0.005) or to patients without previous myocardial infarction (AOR 1.8, 95% CI 1.1 to 2.8, p = 0.013).
| Variable | Psoriasis | p Value | |
|---|---|---|---|
| Yes (n = 204) | No (n = 9,265) | ||
| Any coronary artery disease | 172 (84%) | 7,020 (76%) | 0.005 |
| Any coronary artery disease >70% | 107 (53%) | 4,735 (51%) | 0.7 |
| Vessel with any coronary artery disease ⁎ | |||
| Left main coronary artery | 54 (27%) | 2,453 (27%) | 1.0 |
| Left anterior descending coronary artery | 158 (78%) | 6,227 (67%) | 0.002 |
| Left circumflex coronary artery | 123 (60%) | 5,240 (57%) | 0.3 |
| Right coronary artery | 123 (60%) | 5,672 (61%) | 0.8 |
| Percutaneous coronary intervention performed | 77 (39%) | 3,306 (37%) | 0.7 |
⁎ Columns add up to >100% because a patient could have stenoses in multiple vessels.
| Predictors | Unadjusted OR (95% CI) | p Value | AOR (95% CI) | p Value |
|---|---|---|---|---|
| Psoriasis | 1.72 (1.17–2.52) | 0.005 | 1.84 (1.19–2.83) | 0.006 |
| Age (years) | 1.06 (1.05–1.06) | <0.001 | 1.05 (1.05–1.06) | <0.001 |
| Male gender | 2.04 (1.87–2.29) | <0.001 | 1.95 (1.77–2.22) | <0.001 |
| Caucasian race | 1.18 (1.07–1.31) | 0.001 | 1.06 (0.94–1.20) | 0.359 |
| Body mass index | 0.98 (0.97–0.99) | <0.001 | 0.98 (0.97–0.99) | <0.001 |
| Diabetes mellitus | 2.01 (1.79–2.25) | <0.001 | 1.63 (1.42–1.88) | <0.001 |
| Cerebrovascular disease | 1.76 (1.48–2.10) | <0.001 | 0.91 (0.74–1.12) | 0.373 |
| Hypertension | 2.77 (2.50–3.07) | <0.001 | 1.55 (1.36–1.77) | <0.001 |
| Peripheral vascular disease | 3.48 (2.70–4.48) | <0.001 | 1.58 (1.19–2.11) | 0.002 |
| Current or former smoker | 1.58 (1.43–1.75) | <0.001 | 1.45 (1.29–1.63) | <0.001 |
| Previous myocardial infarction | 3.91 (3.32–4.61) | <0.001 | 2.19 (1.82–2.64) | <0.001 |
| History of hypercholesterolemia | 3.17 (2.87–3.50) | <0.001 | 1.87 (1.66–2.12) | <0.001 |
| Previous coronary bypass | 5.19 (4.07–6.63) | <0.001 | 1.74 (1.32–2.78) | <0.001 |
| Family history of coronary artery disease | 1.20 (1.05–1.38) | 0.007 | 1.33 (1.14–1.56) | <0.001 |
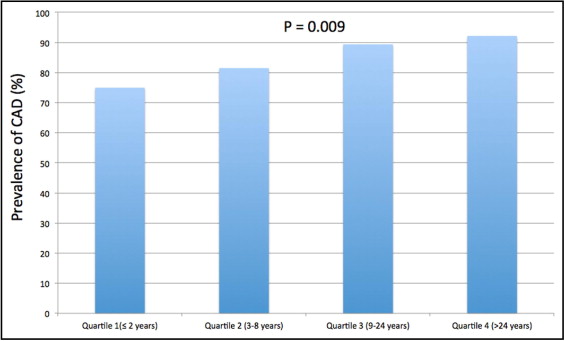
Median duration of psoriasis before cardiac catheterization was 8 years (interquartile range 2 to 24). When patients were divided into quartiles based on duration of psoriasis before cardiac catheterization ( Figure 1 ) , there was a positive association between duration of disease and prevalence of any CAD at coronary angiography (p for trend = 0.009). Patients with psoriasis for >8 years were more likely to have CAD compared to patients who had psoriasis for <8 years (OR 2.7, 95% CI 1.2 to 5.9, p = 0.02). Duration of psoriasis >8 years remained independently associated with any angiographically confirmed CAD after adjusting for age and other established cardiovascular risk factors (AOR 3.4, 95% CI 1.2 to 9.1, p = 0.02).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


