Coronary Artery Disease: Demographics and Incidence
It is widely acknowledged that cardiovascular diseases (CVDs) became the leading cause of mortality and a major cause of morbidity in adults worldwide over the course of the 20th century. Of these diseases, coronary artery or coronary heart disease (CAD) is the single most common cause, accounting for well over 42% of all CVD-related death.1 The World Health Organization (WHO) global burden of disease (GBD) project estimates that >7 million deaths were attributable to CAD in 2004. More than 5.8 million new cases of CAD are added yearly. In order to further define the societal effects, the GBD designed a new measure to capture the effect of years of life lost as a result of both premature death and disability. This metric is termed the disability-adjusted life-year or DALY and reflects a year of healthy life lost to disease. In 2004, CAD accounted for the loss of nearly 62 million DALYs worldwide, making it the fourth leading cause overall, behind lower respiratory infections, diarrheal diseases, and depression (Table 38.1).1
TABLE
38.1 Worldwide Burden of CAD and CVD, 2004
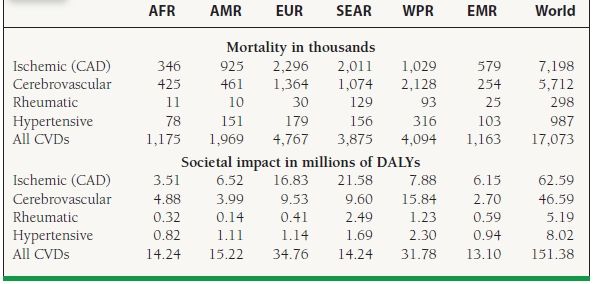
CAD, coronary artery disease; CVD, cardiovascular disease; AFR, Africa; AMR, America; EUR, Europe; SEAR, South East Asia region; WPR, Western Pacific region; EMR, Eastern Mediterranean region; DALY, disability-adjusted life years. Data obtained from the World Health Organization.
Global Temporal Trends in Coronary Artery Disease
Great strides were made in the latter half of the 20th century in the identification and management of traditional risk factors and in the therapeutics and management of acute coronary events, to combat the rising tide of coronary disease. These efforts resulted in dramatic reductions in coronary event rates and CAD-related mortality, mostly in developed countries such as those of Northern Europe. Between the mid-1980s and the mid-1990s, coronary event rates decreased roughly 23% in women and 25% in men, while CAD-related mortality decreased 34% in women and 42% in men. One-third of this reduction in CAD disease burden is attributable to improved therapeutics, whereas two-thirds is attributed to better identification and management of risk factors, leading to a decrease in acute coronary event rates.
Despite these improvements, the trend has been reversed, and we are currently in the midst of a dramatic resurgence in CAD morbidity and mortality. Between 1990 and 2020, worldwide CAD mortality is expected to increase 100% in men and 80% in women. The majority of that increase is expected to occur in the developing world, where rates of CAD mortality are expected to increase 137% in men and 120% in women, whereas in developed countries, the increases are a bit more modest, 48% in men and 29% in women. In terms of DALYs lost, the expected rise is nearly 40%, from 59 to 82 million. The basis for this astounding increase in CAD in the developing world is explained largely by the tightly linked relationship between disease prevalence and various socioeconomic factors. Reductions in mortality from infectious diseases and malnutrition paired with economic prosperity have led to longer life spans worldwide. Along with these changes, modernization and industrialization have led to a decrease in physical activity, increased availability, and consumption of a high-fat, high-calorie diet. These observations, often termed “epidemiological transitions,” occur when a shift occurs in the predominant cause of morbidity and mortality for a given region.2 In the developing world, all of these factors have contributed to rising rates of obesity, diabetes, and lipid disorders that are now well established in the developed, western world.
BURDEN IN THE UNITED STATES
Although the mortality rates from CAD have declined since 1968, it remains the most common manifestation of atherosclerotic CVD and the single most common cause of adult death in the United States, accounting for one of every five, and, in people over the age of 35 years, one of every three (Figs. 38.1 and 38.2; Table 38.2). CVD has accounted for more deaths in the United States than any other major cause every year since 1900 except 1918.3 According to the American Heart Association, 406,351 people died from CAD in 2007, many at the peak of their productive lives. Currently, >16 million people are afflicted with CAD in the United States, with 1.3 million new cases of myocardial infarction (MI), or one every 25 seconds! Of this number, 785,000 represent new cases, whereas 470,000 are recurrent. By comparison, approximately 865,000 people per year suffered a MI from 1987 to 2000, 565,000 per year being new cases. Importantly, 21% of all new MIs in 2007 were symptomatically silent. In terms of societal impact, CAD accounted for the loss of roughly 6.5 million DALYs in 2004, while the estimated average number of years of life lost due to MI is 16.6. It is the leading cause of premature permanent disability, accounting for 19% of Social Security disability outlays.3
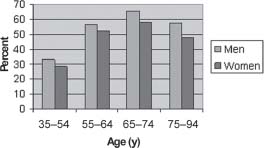
FIGURE 38.1 Proportion of CVD as CAD by age and sex, from Framingham Study, 26-year follow-up. (Reprinted from Lerner DJ, Kannel WB. Patterns of coronary heart disease morbidity and mortality in the sexes: a 26-year follow-up of the Framingham population. Am Heart J. 1986;111(2):383–390, with permission from Elsevier.)
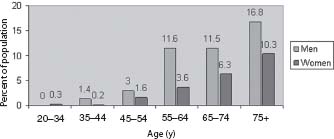
FIGURE 38.2 Prevalence of coronary heart disease by age and sex (National Health and Nutrition Examination Survey: 2005–2008. National Center for Health Statistics and National Heart, Lung, and Blood Institute. *Myocardial infarction diagnosis by expert committee based on review of hospital records.) (From Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123(4):e18–e209, with permission.)
TABLE
38.2 Burden of CAD in the United States, 2008
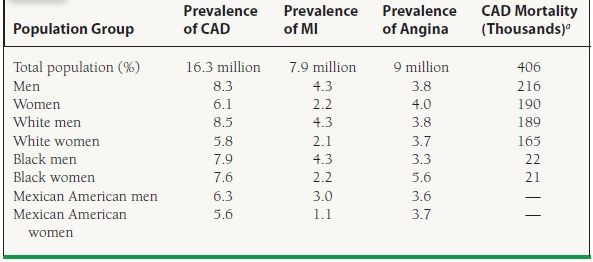
Data are for people age 20 years and older.
aData are for people of all ages.
Roger VL, Go AS, Lloyd-Jones DM, et al.; on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123(4):e18–e209, with permission.
Unrecognized and Silent Myocardial Ischemia and Infarction
The estimated prevalence of asymptomatic significant CAD that is detectable by stress testing or ambulatory ECG is 2% to 4% in the United States.4 Silent ischemia is actually the most common manifestation of clinically significant CAD, even more so than angina. The prevalence of silent myocardial ischemia in men with two or more traditional coronary risk factors (smoking, hyperlipidemia, family history, diabetes, age, hypertension, age >45 years, and obesity) is upwards of 10%. Of these patients, more than half will go on to develop overt clinical manifestations of CAD and come to medical attention. Further, often (75% in one study) these patients have multivessel disease when further investigated. In patients with known coronary disease and stable angina, the prevalence of silent ischemia is estimated to be between 25% and 50%. Additionally, 70% to 80% of ischemic episodes in patients with stable angina are silent. Unrecognized MI has two components, asymptomatic or silent MI (approximately 50%), and that which is associated with such atypical symptoms that infarction is not entertained as part of the differential (approximately 50%). One in three MIs can actually be classified as unrecognized. The long-term morbidity and mortality of silent ischemia and unrecognized MI is similar to that of recognized MI (Figs. 38.3 and 38.4).5
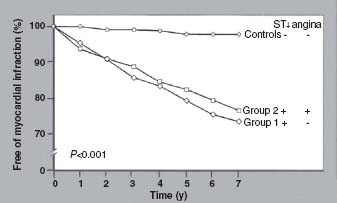
FIGURE 38.3 Outcome of patients with angina (Group 2) or silent ischemia (Group 2) and exercise-induced ST depression in the Coronary Artery Surgery Study (CASS) registry. Controls had no objective evidence of ischemia. (Reprinted from Weiner DA, Ryan TJ, McCabe CH, Ng G. Risk of developing an acute myocardial infarction or sudden cardiac death in patients with exercise induced silent myocardial ischemia: a report from the Coronary Artery Study (CASS) Registry. Am J Cardiol. 1988;62(17):1155–1158, with permission from Elsevier.)
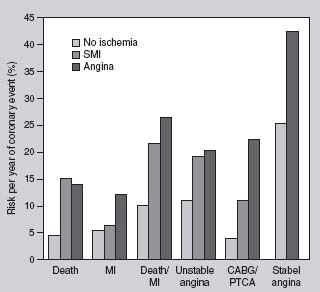
FIGURE 38.4 Long-term outcome of patients post myocardial infarction with angina versus silent ischemia versus no objective ischemia. SMI, silent myocardial ischemia; CABG, coronary artery bypass grafting; PTCA, percutaneous coronary angioplasty; MI, myocardial infarction. (With kind permission from Springer Science+Business Media: Essential Atlas of Heart Diseases, 2005, Braunwald E.)
Diabetic and hypertensive patients seem to be most susceptible to unrecognized MI.
Age and Gender Variation
The average age of a person presenting with a first MI in the United States is 65 years for men and 70 years for women. Figures 38.2 and 38.5 provide a sense of how strongly the prevalence and incidence of CAD is influenced by age and gender. The incidence of serious manifestations of CAD, such as MI or death, more than doubles between the age ranges of 65–74 and >85 for men and nearly quadruples for women. Further, data from the Centers for Disease Control (CDC) demonstrate that 83% of people who die from CAD are 65 years or older. After age 40 years, men have a lifetime risk of developing CAD of 49%, while women have a risk of 32%. After 70 years this risk decreases to 35% for men and 24% for women.6
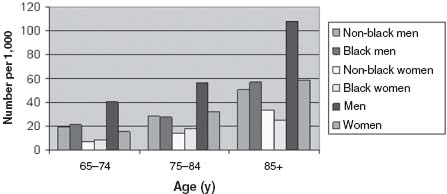
FIGURE 38.5 Incidence of myocardial infarction* by age, race, and sex (Atherosclerosis Risk in Communities Surveillance, 1987–2004). *Myocardial infarction diagnosis by expert committee based on review of hospital records. (From Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123(4):e18–e209, with permission.)
The incidence of any manifestation of CAD in women lags behind that in men by 10 years, whereas the incidence of MI or sudden death lags by 20 years. In fact, excluding people >75 years of age, women are much more likely to present with angina as their first manifestation of CAD, whereas men more often present with MI (Fig. 38.6). In terms of CAD mortality, gender differences narrow significantly with age. Between the ages of 45 and 64 the 1-year mortality following a first MI is 5% for white men, 14% for black men, 9% for white women, and 8% for black women. However, after the age of 65, 30% of women (white or black) will die within 1 year compared to only 25% of men (white or black).3

FIGURE 38.6 First manifestation of CAD in men and women by age. MI, myocardial infarction. (Reprinted from Lerner DJ, Kannel WB. Patterns of coronary heart disease morbidity and mortality in the sexes: a 26-year follow-up of the Framingham population. Am Heart J. 1986;111(2):383–390, with permission from Elsevier.)
Finally, menopause, whether natural or surgical, has a significant influence on the incidence and severity of CAD. Indeed, the incidence of serious manifestations of CAD is rare in premenopausal women but increases more than threefold in age-matched postmenopausal women. Of note, polycystic ovarian disease increases the likelihood of premature CAD in women.3
Racial and Socioeconomic Disparities
CAD is the leading cause of death in the United States for every major ethnic group. The self-reported prevalence of CAD and MI and the CAD mortality rates in various racial and ethnic groups according to the latest AHA update are shown in Table 38.2 and Figure 38.7. The most conspicuous feature of these data is that the CAD mortality rate is highest among blacks overall. Indeed, the mortality rate among black Americans is 1.6 times that of whites, a ratio that has not changed since the 1950s.7 This difference is particularly striking among younger people, aged 35 to 44 years, in whom the mortality among blacks is reported to be 50% higher than among whites. This difference disappears by age 75 years. Additionally, the incidence of CAD is particularly high among South Asians. The mortality rate among East Asians, Hispanics, and Native Americans or Alaskans is not nearly as high as that among whites or blacks. In terms of socioeconomic differences, numerous studies have linked lower income levels, lower educational levels, and other social factors to elevated CAD risk. One recent study showed a 2.5- to 3-fold increased risk in people living in poorer neighborhoods compared with those living in higherincome neighborhoods, even after adjusting for other socioeconomic and traditional risk factors.8
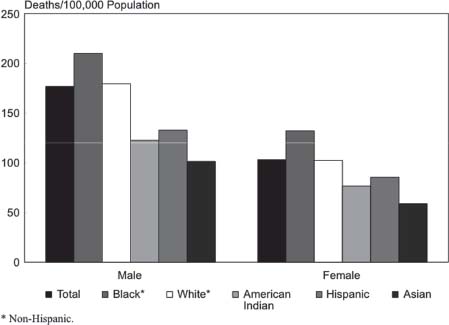
FIGURE 38.7 Age-adjusted death rates for coronary heart disease by race/ethnicity and sex, U.S., 2006. (Morbidity & Mortality: 2009 Chart Book on Cardiovascular, Lung, and Blood Diseases. 2009, National Institutes of Health.)
CAD in the Young
Symptomatic CAD in people under the age of 40 to 45 years is a fairly uncommon problem. In autopsy studies, however, the prevalence of anatomic CAD is roughly 20% in men and 8% in women aged 30 to 34 years.3 This is consistent with the finding of a delay in manifestations of CAD in women versus men and that atherosclerosis, despite its relative rarity in the young, is a process that begins at an early age. People presenting with CAD at a young age tend to have multiple risk factors as well as a significant family history of premature CAD. Tobacco use is very common among this population; however, the prevalence of dyslipidemia is similar to those presenting later in life. Often, this population tends to have some manifestations of the metabolic syndrome, such as low HDL, elevated triglycerides, and glucose intolerance. With the current epidemics of obesity and the metabolic syndrome in the United States, it seems likely that the incidence of symptomatic CAD in young people is either on the rise currently, or soon will be.
Temporal Trends in CAD
Autopsy studies over the past few decades have shown a decreasing prevalence of anatomically significant CAD in people 59 years of age and younger in the United States. From the periods 1979 to 1983 and 1990 to 1994, the prevalence of CAD decreased from 42% to 32% among men and from 29% to 16% among women.9 There was no change in those >60 years of age. Similarly, the incidence of clinically manifested CAD decreased from the 1970s to the 1980s. The National Health and Nutrition Examination Survey (NHANES) tracked two cohorts of patients from 1971 to 1982 and from 1982 to 1992 and found that the prevalence of CAD over these time periods decreased from 133 to 114 cases per 10,000 persons per year of followup. Over a similar time period, the overall incidence of MI remained relatively stable. However, from 2000 to 2008 the incidence of MI decreased from 287 cases per 100,000 person-years to 208 cases per 100,000 person-years, a relative decrease of 24%. This was even more impressive among patients with ST-segment elevation MI (STEMI) where from 1999 to 2008 there was a relative decrease of 62%, from 133 to only 50 cases per 100,000 persons. For non–ST-segment elevation MI (NSTEMI), the incidence actually increased between 1999 and 2004, from 155 to 202 cases per 100,000 persons, likely reflecting the newer and more sensitive troponin assays being widely utilized. Even still, the incidence of NSTEMI has been decreasing since 2004 (Fig. 38.8).10
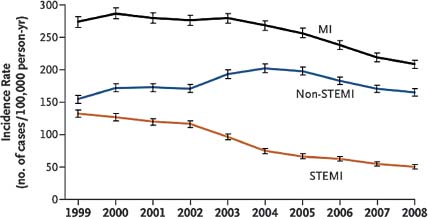
FIGURE 38.8 Age- and sex-adjusted incidence rates of acute myocardial infarction, 1999 to 2008. Bars represent 95% confidence intervals. MI denotes myocardial infarction, and STEMI ST-segment myocardial infarction. (From Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362(23):2155–2165, with permission from the Massachusetts Medical Society.)



