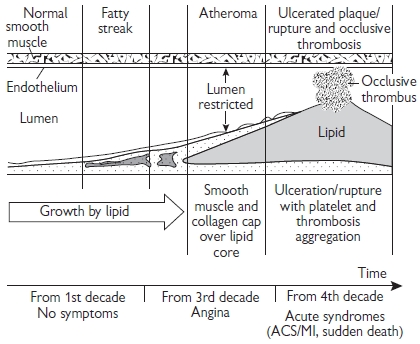
Atherosclerosis is a disease of the large and medium-sized arteries. The term atherosclerosis is derived from Latin and means gruel-like (‘athero’) hardening (‘sclerosis’) of the arteries. The disease is characterized by a gradual build up of fatty plaques within the arterial wall, which eventually results in a significant reduction of the vessel lumen, impairing blood flow to the distal tissues. These plaques may also cause acute coronary syndromes by becoming unstable and triggering coronary thrombosis.
Pathophysiology
The atherogenic process is characterized by:
• dysfunction of the endothelial lining of the vessel
• inflammation of the vascular wall
• build up of lipids, cholesterol, and inflammatory cells in the vessel wall
• accumulation of cellular debris within the intima and subintimal layers of the vessel.
These processes result in plaque formation, and remodelling of the arterial wall. The underlying mechanisms are uncertain, but the most widely accepted theory is the ‘response-to-injury’ hypothesis defined by Ross in the 1970s.
Endothelial dysfunction
The initiating trigger of this disease process appears to be injury of arterial endothelial cells from exposure to stimuli including:
• tobacco toxins
• oxidized low-density lipoprotein (LDL)
• advanced glycation end-products
• elevated homocysteine
• infectious agents.
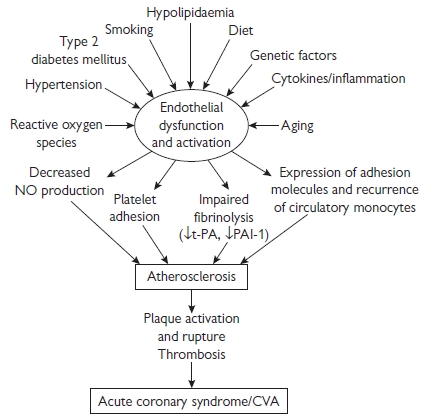
Endothelial cell injury initiates a cascade of events resulting in cellular dysfunction (see Fig. 5.1). The hallmark of endothelial dysfunction is a change in the balance of production of endothelium-derived vasoactive molecules:
• reduced bioavailability of endothelial nitric oxide (NO), an important vasodilator, anti-thrombotic, and antiproliferative agent
• increased generation of potent vasoconstrictor agents endothelin-1 and angiotensin-II, promoting cell migration and growth
• dysfunctional endothelial cells express adhesion molecules and secrete chemokines, promoting cell migration and adhesion
• local thrombotic balance is altered as levels of plasminogen activator inhibitor (PAI) and tissue factor are increased
• tissue plasminogen activator (t-PA) and thrombomodulin are reduced
• low NO release results in increased platelet activation and adhesion.
Endothelial dysfunction creates a local milieu, which facilitates the initiation and development of the atherogenic process (see Fig. 5.2).
• Circulating leucocytes, predominantly monocytes, are attracted and bind to activated endothelial cells, followed by migration into the subendothelial layer, where they transform into macrophages.
• They act as local ‘scavenger’ cells with the capacity to take up modified LDL cholesterol (LDL-C), ultimately becoming the characteristic ‘foam cells’ of established atherosclerosis.
• The earliest lesions are known as ‘fatty streaks’, which consist predominantly of lipid-accumulating macrophages and foam cells.
• These lesions may develop into fibrous plaques, as a consequence of further lipid accumulation accompanied by local migration, proliferation, and fibrous transformation of smooth muscle cells.
• These cells are responsible for the deposition of extracellular connective tissue matrix, leading to formation of a fibrous cap, which overlies a central core, consisting of foam cells, extracellular lipid, necrotic cellular debris, and a mixture of other inflammatory cells including T-lymphocytes.
• This process is facilitated by ongoing endothelial dysfunction, together with local generation of powerful mitogens such as platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), and insulin-like growth factor (IGF) from endothelial cells, macrophages, and activated platelets.
• Further growth of the plaque initially causes outward remodelling of the vessel wall, minimizing the impact on the cross-sectional area of the lumen and the vessel’s ability to deliver blood.
• Progressive plaque accumulation results in luminal narrowing, and ultimately vessel obstruction.
Lesion initiation and progression tends to occur more predictably at certain locations of the vascular system.
• Blood flow through arteries causes local generation of fluid ‘shear-stress’, which influences the biology of the underlying endothelial cells.
• High laminar shear (from blood flowing quickly through a straight vessel) favours the generation of NO, which helps maintain the functional integrity of the vessel.
• In contrast, low shear, or ‘differential’ shear caused by turbulent flow, causes dysfunction of the underlying endothelial cells, which facilitates initiation and progression of atheroma.
• This helps explain why plaques are found more commonly at sites of vessel branching or curvature, which experience more dramatic and abrupt changes and irregularities of direction and velocity of blood flow.
• These shear-stress-mediated effects are most marked in vessels that carry a high (basal) blood flow, such as the coronary, carotid, renal, and ilio-femoral arteries, in which the majority of clinically important atherosclerotic lesions develop.
Cardiovascular disease is the most common cause of death in the UK, responsible for 238 000 deaths in 2002 or 39% of all deaths. Coronary artery disease (CAD) results in over 117 000 deaths a year in the UK. Advances in prevention and treatment of this disease have led to a fall in the death rate since the late 1970s, but the UK incidence of CAD remains amongst the highest in the world. The cost of health care alone is estimated at over £1.7 billion a year, and the total economic cost is far greater.
Regional variation
There is considerable variation in mortality from CAD across the UK. Death rates are higher in Scotland than the South of England, in manual workers than in non-manual workers, and in certain ethnic groups. There are several important risk factors that are associated with CAD and other atherosclerotic disease (see Risk factors for coronary artery disease, p. 220), which together account for the majority of the CAD burden in the UK. Although identification and treatment of individuals with these risk factors has the potential to reduce significantly the burden of CAD, the incidence of and death rate from MI remain high.
The vulnerable plaque
Erosion or denudation of the endothelial layer, or rupture of the overlying fibrous cap of the plaque may expose the highly thrombogenic lipid-rich core of the plaque to circulating blood.
• Collagen, tissue factor, and other factors activate platelets and trigger the coagulation cascade.
• This leads to acute thrombosis, which may rapidly occlude the vessel.
• This results in MI of this vascular territory, usually characterized by ST-segment elevation on the electrocardiogram (ECG).
• Coronary thrombosis is a dynamic process in vivo, and may be reversed, at least in part, by activation of t-PA and proteins C and S of the intrinsic antithrombotic/fibrinolytic system.
• Acute, subtotal occlusion of the vessel typically causes acute symptomatic deterioration and non-ST-segment elevation MI (NSTEMI) or unstable angina.
• Atheromatous plaques that have a thin fibrous cap and a large necrotic lipid core, and contain a high proportion of inflammatory cells and mediators, and are particularly predisposed to destabilization or rupture, with consequent thrombosis.
• Conversely, plaques with a smaller lipid pool, thicker fibrous caps, and less inflammatory activity are more stable and less prone to rupture.
• Several studies have shown that well over half of all MIs are caused by acute destabilization of plaques that were previously not obstructing flow in the vessel, suggesting that the likelihood of an acute coronary event is more closely related to the stability of the plaque rather than the severity of the stenosis.
Identification and treatment of risk factors is essential for the prevention of atherosclerotic disease in both individuals and society. When multiple risk factors such as dyslipidaemia, high blood pressure, and smoking co-exist, the cardiovascular risk is greatly increased, suggesting a synergistic interaction between these factors.
Global risk assessment
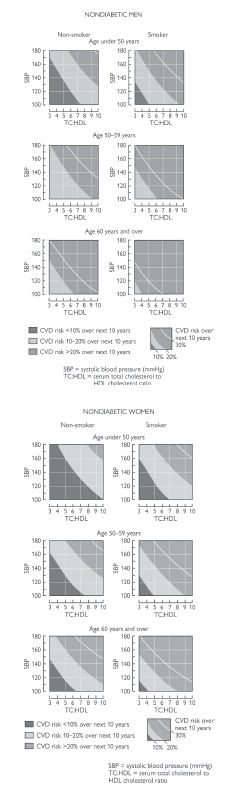
Risk-assessment scoring systems are derived from large prospective population cohorts, most commonly the Framingham study. These systems allow calculation of the ‘absolute risk’ of having a cardiovascular event (i.e. the probability of having a heart attack or stroke) within the next 10 years. Current UK practice recommends use of the Joint British Societies risk-assessment tables (see Fig. 5.3) or a computer program. Other commonly used methods include:
• the Framingham risk-scoring system
• the Sheffield tables
• the European SCORE charts.
Subjects with stable angina have a 10-year event rate of approximately 20%; therefore, subjects without clinical disease that have a predicted 10-year likelihood of suffering a cardiovascular event of ≥20% are considered to be at ‘high risk’ and are candidates for aggressive risk-factor management.
Individuals with low-intermediate risk —scoring systems typically underestimate the true risk in:
• young subjects with multiple risk factors
• subjects with a family history of premature cardiovascular disease
• certain ethnic groups including individuals of South Asian racial origin living in the UK.
Identification of subjects with intermediate (10–20%) conventional risk scores that are actually at ‘high’ risk remains a major challenge, as these individuals are also likely to benefit from preventive therapy.
Adjunctive risk-assessment techniques may improve risk-assessment accuracy but are not currently used in routine clinical practice:
• C-reactive protein (CRP) levels
• ultrasound assessment of carotid arterial intima–media thickness
• detection of coronary artery calcification with computed tomography (CT) scanning.
• Calculation of risk is unnecessary in subjects who already have clinical atherosclerotic disease, as secondary prevention measures are mandatory in these individuals.
• Similarly, risk calculation is not required for subjects with diabetes mellitus, whose risk approaches that of subjects with established atherosclerosis.
Age
The UK population is aging:
• between 1971 and 2002, the percentage of older people (aged 65 years and over) in the UK, increased from 13% to 16%, and is projected to rise to 23% in the next 25 years
• aging is a major risk factor for atherosclerotic disease, due to the degenerative process associated with aging per se, together with the cumulative impact of the worsening risk-factor profile that develops with increasing age
• by the age of 70 years, 15% of men and 9% of women have symptomatic CAD, increasing to 20% by the age of 80 years
• Over 40 000 premature (<75 years) deaths are caused by CAD, 22% of premature deaths in men and 13% of those in women
• 45% of MI occurs in people under 65 years of age but is more likely to be fatal in older individuals, with 80% of deaths due to MI seen in those aged over 65 years.
Gender, menopausal status, and hormone replacement therapy (HRT)
• CAD is more common in men than women and the onset tends to be earlier in men.
• The incidence of coronary heart disease (CHD) in women increases rapidly at menopause, and is similar to that seen in men in the population over 65 years.
• Although less common, the disease remains one of the biggest killers of women; for example, the age-adjusted mortality rates from heart disease are four to six times higher than their mortality rates from breast cancer.
• Female sex hormones probably contribute to the lower risk of atherosclerotic disease in premenopausal women.
• The risk of ischaemic heart disease is reduced by up to 40% in women using HRT. HRT users are typically healthier than non-users, suggesting that these results could be explained by selection bias.
• Several large, randomized controlled trials of HRT in postmenopausal women (WHI (Women’s Health Initiative), HERS (Heart and Estrogen/Progestin Study)/HERS II, ESPRIT (Estrogen in the Prevention of Reinfarction Trial), ERA (Estrogen Replacement and Atherosclerosis)) with and without atherosclerosis have now clearly shown that HRT does not reduce the risk of cardiovascular events.
• HRT may, in fact, even lead to a small but statistically significant increase in morbidity and mortality from cardiovascular and other diseases including gynaecologic malignancy.
• HRT should not be recommended for primary or secondary prevention of atherosclerotic disease in postmenopausal women.
• CAD is a multifactorial, polygenic disorder, caused by interactions between lifestyle, the environment, and the effects of variations in the genetic sequence of a number of genes.
• The family history is considered to be significant when atherosclerotic disease presents in a first-degree male relative before the age of 55 years, or before 65 years in a female relative.
• A positive family history is associated with a 75% increase in risk in men, and an 84% increase in women. The risk is more than doubled if both parents are affected.
Risk factors for coronary artery disease
|
• Increasing age
• Male sex
• Family history
• Ethnic origin |
• Smoking
• High blood pressure
• Dyslipidaemia
• Diabetes mellitus
• Obesity and the metabolic syndrome
• Psychological stress
• High-calorie high-fat diet
• Physical inactivity |
Emerging risk factors
• Inflammation
• Fibrinogen, and other factors involved in thromboregulation
• Homocysteine
• Oxidative stress
• Asymmetric dimethylarginine
Ethnic origin
• Age-standardized mortality from CAD is around 50% higher in individuals of South Asian racial origin living in the UK compared to white individuals.
• Although an increased prevalence of risk factors explains much of this risk (high triglycerides, low high-density lipoprotein (HDL), insulin resistance, and reduced physical activity), genetic factors are thought to contribute significantly.
• The observed incidence of CAD is lower in black individuals of West Indian and African origin in the UK, although the incidence of stroke is greater than in the Caucasian population.
Psychological stress
• The burden of risk attributable to psychological stress is more difficult to quantify.
• Increased work stress, lack of social support, hostile personality type, anxiety, and depression are most consistently associated with increased atherosclerosis risk.
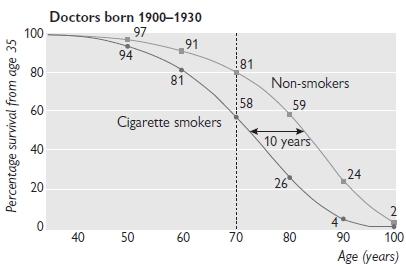
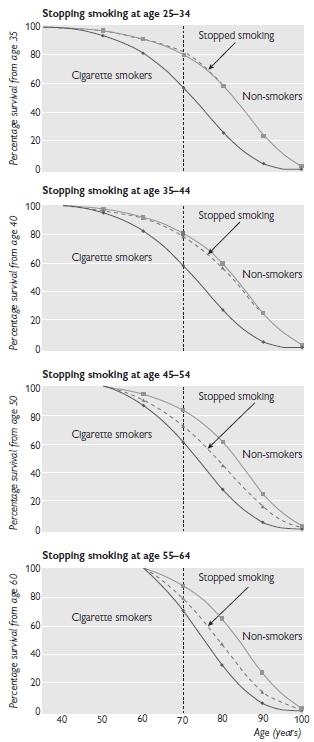
• Smoking increases the risk of CAD by approximately 50%, with mortality from any cardiovascular disease around 60% higher in smokers (and 85% higher in heavy smokers) compared to non-smokers.
• In the UK today, around 13 million adults (28% of men and 26% of women) smoke cigarettes.
• Although the number of smokers has declined substantially over the past 50 years, this trend has slowed down in the young, and the number of teenage girls that smoke has recently increased.
• Over 30 000 cardiovascular deaths per year (14% in men and 12% in women, with an even higher proportion of premature deaths) are attributable to smoking.
• Second-hand smoke (smoke that has been exhaled by a smoker) can also increase the risk of CAD by around 25%.
• Stopping smoking carries almost immediate benefit, and although the long-term benefits are greatest in those who stop smoking before the age of 40 years, stopping in middle age is also beneficial. For example, in those aged 30–59 years who stop smoking after a MI, the 5-year mortality is 10%, compared with 14% in those who continue to smoke.
• Individuals at increased risk of atherosclerosis should be advised to stop smoking. See
Figs. 5.4. and
5.5.
• Evidence now exists that focused psychosocial support, nicotine replacement, and pharmacological therapy are effective in helping individuals stop smoking. These services are delivered in an integrated fashion by smoking-cessation clinics, which can deliver a fourfold increase in the likelihood that a smoker will quit, vs. use of willpower alone.
• Obesity increases the risk of CAD: 25–49% of CAD in developed countries is attributable to increased body mass index (BMI).
• Overweight is defined as a BMI between 25 and 30 kg/m2, and obesity as a BMI ≥30 kg/m2.
• The prevalence of obesity is increasing rapidly worldwide. In the UK, adult obesity has increased by over 50% in less than 10 years.
• Of particular concern is the dramatic increase in the prevalence of obesity in children, which has almost doubled in the UK in less than 10 years. This trend is likely to exacerbate the problem in adulthood, and undo many of the other recent improvements in cardiovascular health.
• Central obesity, in which excess fat is concentrated mainly in the abdomen, can be identified by a high waist-to-hip ratio, and confers a particularly high relative risk of CAD if the waist circumference is >102 cm (40 in.) in men and >88 cm (35 in.) in women.
• Associated metabolic abnormalities of central obesity include high triglycerides, low HDL, high blood pressure, low-grade systemic inflammation, insulin resistance, and type 2 diabetes mellitus.
• Overweight and obese individuals also tend to be less physically active and eat lower-quality diets, which contributes further to their atherogenic risk.
• Diet and exercise should be considered as the first line of intervention in these individuals, together with careful surveillance for and aggressive treatment of diabetes, high blood pressure, and dyslipidaemia when present.
Inflammation
• Atherosclerosis involves an ongoing inflammatory process from the time of lesion initiation, through progression and at the time of acute thrombotic complication.
• This links risk factors and the disease mechanism in a way that is directly applicable to human patients.
• Large studies have shown that low-grade elevation in markers of inflammation, most notably CRP, predicts outcomes from atherosclerotic disease and may add to prognostic information provided by traditional risk factors.
• A CRP level below 1 mg/L is associated with low risk, 1–3 mg/L reflects intermediate risk, and a level above 3 mg/L is associated with a high long-term risk of vascular events.
• Certain treatments that reduce coronary risk also limit inflammation, such as statins and aspirin, which may contribute to their clinical benefits.
• The incremental value of CRP as a marker of risk and target of therapy in global risk management is currently a controversial topic that requires clarification by prospective randomized trials.
Homocysteine
• The genetic disease homocystinuria is associated with aggressive, premature atherosclerosis.
• Vascular inflammation and oxidative stress appear to be the responsible mechanisms.
• Dietary supplementation with folic acid, alone or in combination with vitamins B6 and B12, can reduce levels of homocysteine and improve aspects of vascular biology in vivo as well as in vitro.
• Until results of large, outcome-driven, randomized clinical trials are available, folate ± B6/B12 supplementation cannot be routinely recommended for prevention of atherosclerotic disease.
Antioxidant vitamins
Despite excellent epidemiologic and mechanistic evidence that increased oxidative stress is associated with vascular injury, inflammation, and increased risk of cardiovascular morbidity and mortality, it is disappointing that large randomized controlled trials (HOPE (Heart Outcomes Prevention Evaluation), HPS (Heart Protection Study) and GISSI-P (Gruppo Italiano per lo studio della Sopravvivenza nee’infarto Miocardio)) showed that supplementation with the antioxidant vitamin E (supplemented with vitamins A and C in HPS) had no effect on cardiovascular outcome. Currently, antioxidant vitamin supplementation should not be routinely recommended for prevention of atherosclerotic disease.
Dietary measures
Dietary modification can reduce the risk of cardiovascular disease:
• total fat intake should be reduced to below 30% of total calorie intake
• intake of saturated fat and foods high in ‘trans’ fatty acids should be limited, and replaced with monounsaturated fat (canola and olive oil)
• dietary salt intake should be reduced
• intake of fresh fruits and vegetables should be increased (≥5 portions per day)
• fish consumption, especially oily fish, should be encouraged, with evidence suggesting that at least one fish meal, and ideally 2–3 per week can reduce the incidence of heart attack and stroke.
Physical activity
• The contribution of physical inactivity to CAD deaths is difficult to quantify; however, people who are physically active appear to have a lower risk of CAD.
• This is mediated, at least in part by weight loss, a reduction in blood pressure, and improvement of the lipid profile (particularly increased HDL).
• Regular, aerobic exercise of moderate intensity should be undertaken ≥3 times per week for at least 30 minutes, but greater frequency and duration of exercise is associated with increasing benefits.
Alcohol
Moderate alcohol consumption (one or two drinks per day) is associated with a reduced risk of CAD, whereas higher levels of alcohol intake (in excess of 21 units/week for men or more than 14 units/week) in women, particularly in ‘binges’, is associated with an increased risk of CHD.
Definition
A continuous relationship exists between increasing blood pressure and cardiovascular risk; therefore, it is impossible to define hypertension precisely. For practical purposes, levels of blood pressure above which the risk increases significantly, and treatment can provide a clear-cut benefit, are used as a working definition of hypertension (see Table 5.1). The average of two readings at each of a number of visits should be used to define the blood pressure.
Table 5.1 Blood pressure (BP) classification
|
Optimal BP |
<120 |
<80 |
Normal BP |
<130 |
<85 |
High–normal BP |
130–139 |
85–89 |
Grade 1 hypertension |
140–159 |
90–99 |
Grade 2 hypertension |
160–179 |
100–109 |
Grade 3 hypertension |
≥180 |
≥110 |
Adapted from British Hypertension Society (2004).  http://www.bhsoc.org
http://www.bhsoc.org
Causes of hypertension
The majority of subjects (>95%) have essential (primary) hypertension, in which an underlying cause for the hypertension is not found.
There are many causes of secondary hypertension (see Table 5.1).
Symptoms and signs
Hypertension is usually asymptomatic, although a patient will occasionally complain of headache. A history of cardiac or neurologic symptoms should always be sought. The cardiovascular system should be examined in detail, and fundoscopy should be performed to look for retinopathy (see Table 5.1).
Clinical signs of an underlying cause (radiofemoral delay or weak femoral pulses, renal enlargement or bruit, or cushingoid features) and evidence of end-organ damage (heart failure, retinopathy, aortic aneurysm, carotid or femoral bruit) should be sought.
Malignant hypertension is diagnosed when severe hypertension (systolic blood pressure (SBP)>200 mmHg ± diastolic blood pressure (DBP)>130 mmHg) is identified, together with grade III–IV retinopathy.
• The patient often has a headache and occasionally visual disturbance.
• Proteinuria and haematuria are often present.
• This is a medical emergency requiring immediate treatment to prevent rapid progression to renal failure, heart failure, and/or stroke.
• Untreated, the 1-year mortality is approximately 90%.
Investigation
Important investigations in all patients presenting with hypertension are:
• ECG
• fasting glucose
• full lipid profile (total, HDL and LDL cholesterol and triglycerides)
• urea and electrolytes (U&E)
• urinalysis for blood and protein
If secondary hypertension is suspected, further investigation should focus on the possible underlying cause (e.g. urinary cortisol, plasma renin-aldosterone levels, renal ultrasound, magnetic resonance angiography (MRA) of renal arteries, MAG3 renogram, and 24-hour urinary catecholamines or vanillyl mandelic acid (VMA)).
Secondary hypertension (<5%)
Renal disease
• Diabetic nephropathy, renovascular disease, glomerulonephritis, vasculitides, chronic pyelonephritis, polycystic kidneys
Endocrine disease
• Conn’s and Cushing’s syndromes, glucocorticoid-remediable hypertension, phaeochromocytoma, acromegaly, hyperparathyroidism
Other
• Aortic coarctation, pregnancy-induced hypertension and pre-eclampsia, obesity, excessive dietary salt or licquorice intake, drugs (non-steroidal anti-inflammatory drugs (NSAIDs), sympathomimetics, illicit stimulants, e.g. amphetamine, MDMA (‘ecstasy’), and cocaine
Grading of hypertensive retinopathy
I. Tortuous arteries, with thickened bright walls (‘silver wiring’)
II. Arteriovenous nipping (narrowing in a vein where crossed by an artery)
III. Flame haemorrhages and cotton wool spots (small retinal bleeds and exudates)
IV. Papilloedema
When to treat
• Patients with malignant hypertension or with persistent BP>160/100 mmHg after lifestyle measures
• Subjects with BP>140/90 mmHg after lifestyle measures who have evidence of end-organ damage (left ventricular hypertrophy (LVH) on ECG, proteinuria or retinopathy) or a calculated 10-year risk of a cardiovascular event ≥20%
• Subjects who have clinical evidence of CAD, peripheral or cerebrovascular disease if BP>140/90 mmHg.
Blood pressure targets
• Most patients should have their BP lowered to a target of <140/85 mmHg.
• Patients with diabetes, have been shown to benefit from more aggressive BP reduction (UKPDS (UK Prospective Diabetes Study) and HOT (Hypertension Optimal Treatment) studies), and a target of <130/80 mmHg is more appropriate.
Lifestyle measures
• Minimize dietary salt intake (<100 mmol/day)
• Reduce alcohol to <21 units (men) and <14 units (women) per week
• Take regular aerobic exercise if not contraindicated (at least 30 min, 3x/week)
• Achieve and maintain healthy BMI (20–25 kg/m2)
• Consume at least 5 portions/day of fresh fruit and vegetables
• Stop smoking, and reduce dietary fat content, especially saturated and trans-fatty acids.
Uptake of these lifestyle measures is often difficult to sustain, and implementation is most successful in a multidisciplinary professional setting when supported by clear written information, including individualized strategies and goals.
Choice of drug therapy
Large meta-analyses of studies of BP-lowering therapy have clearly shown that the degree of blood pressure lowering is the best determinant of risk reduction. Comparative studies, such as ALL-HAT (Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack), have typically shown that there is little evidence favouring one class of drug over another with respect to overall cardiovascular outcome.
• Thiazide diuretics are effective and cheap and widely recommended as first-line antihypertensive therapy.
• Although calcium-channel blockers may be less protective than other agents against the development of heart failure, their safety and effectiveness in preventing atherosclerotic events is now confirmed, despite previous concerns.
Compelling indications for specific class of antihypertensive agents
See Table 5.2.
Table 5.2 Indications for antihypertensive drugs
|
Alpha-blocker |
Benign prostatic hypertrophy |
Angiotensin-converting enzyme inhibitors (ACE-Is)/ARBs |
Heart failure/LV-dysfunction
Established CAD
Type 1 diabetic nephropathy, secondary stroke prevention
ACE-I intolerant (ARB indicated)
Type 2 diabetic nephropathy
Hypertension + LVH |
Beta-blockers |
MI
Angina
Heart failure |
Calcium-channel blockers |
Elderly
Systolic hypertension
Angina |
Thiazide diuretics |
Elderly
Heart failure
Systolic hypertension |
Adapted from British Hypertension Society (2004).  http://www.bhsoc.org
http://www.bhsoc.org
Most hypertensive individuals require more than one drug to control their blood pressure. Combining drugs at an earlier stage in the up-titration of therapy often results in better control with fewer side-effects than maximizing the dose of individual agents.
The that helps guide appropriate combination of antihypertensive drugs in clinical practice (see Table 5.3).
Table 5.3 Combining antihypertensive drugs: (The BHS A-B-C-D principle)
|
STEP 1 |
A or B |
C or D |
STEP 2 |
A + C or D |
|
STEP 3 |
A (or B) + C + D |
|
STEP 4 |
Add B-blocker/spironolactone/or other diuretic |
|
• This is based on the A-B-C-D principle (A = ACE-I or ARB, B = β-blocker, C = calcium-channel antagonist, D = diuretic).
• A or B are effective first-line drugs in the young, who typically have high-renin hypertension that responds well to these drug classes.
• C or D are more effective first-line agents in the elderly and black individuals, who typically have lower levels of renin and are less responsive to these agents.
• Drugs can be substituted or added in a stepwise fashion according to the response, until BP is controlled.
• Care should be taken if prescribing B + D together, as this combination may slightly increase the incidence of type 2 diabetes. ACE-I and ARB therapy can both reduce risk of developing this condition.
Other therapy
• The lipid-lowering arm of the ASCOT (Anglo-Scandinavian Cardiac Outcomes Trial) study was terminated early due to a sizeable reduction in major vascular events seen in patients with hypertension and ‘average’ cholesterol levels treated with atorvastatin 10 mg daily for less than 4 years.
• Aspirin 75 mg daily is recommended in hypertensive patients with evidence of clinical atherosclerotic disease or ≥20% 10-year cardiovascular event risk, after adequate BP control is achieved (<150/90 mmHg).
• Statin therapy should be initiated in these high-risk individuals, regardless of baseline cholesterol levels.
• Target lipid levels are total cholesterol (TC)<4.0 mmol/L, LDL-C<2.0 mmol/L, or a >25% or >30% reduction in TC or LDL-C respectively, whichever is the greater.
Adapted from British Hypertension Society (2004).  www.bhs.co.uk
www.bhs.co.uk
Other drugs to consider include hydralazine, α-methyl dopa, clonidine, moxonidine, and minoxidil, but it is advisable that use of these drugs is supervised by a specialist.
Dyslipidaemia and risk of atherosclerosis
Numerous epidemiologic studies have confirmed that a direct relationship exists between cholesterol level and risk of CAD, even with the normal range of cholesterol. Increasing LDL-C levels appears to be the main driver of this pathologic relationship, but other atherogenic lipoprotein particles including very low-density lipoprotein (VLDL), chylomicron remnants, and lipoprotein(a) (Lp(a)) also appear to play an important role. LDL, particularly modified LDL, is recognized by the scavenger receptor on the surface of macrophages in the arterial wall, which take up these cholesterol-rich particles and eventually become the foam cells that form the lipid-rich core of atherosclerotic plaques. Increasing levels of HDL, involved in reverse cholesterol transport from the peripheries to the liver, protect against the development of atherosclerosis. Increased triglyceride levels are now also established as an independent risk factor for CAD. Emerging studies suggest that, in addition to the circulating lipid concentrations, the nature of the lipoprotein particles plays an important part in their atherogenic risk. For example, small dense LDL particles, as seen in subjects with diabetes, are more readily taken up by macrophages and appear to be more atherogenic than larger less-dense LDL.
Lipids and risk assessment
It is critical to consider the lipid profile in the context of the other risk factors present in the individual, by calculating 10-year cardiovascular risk. Although only TC and HDL-C are considered in most risk models, the levels of LDL and cholesterol and triglycerides should also be considered in the overall picture. Although blood should ideally be drawn for lipid analysis after a 12-hour fast, TC and HDL-C levels are only minimally affected by eating and are still valid in a non-fasting sample, unlike triglycerides and calculated LDL-C.
Measure a fasting lipid profile if the patient:
• is over 50 years of age
• has clinical atherosclerotic disease
• has ≥other risk factors for atherosclerosis
• has clinical signs of hyperlipidaemia (xanthomata, xanthelasmata, or corneal arcus at age <50 years)
• has a family history of premature CAD or hyperlipidaemia.
Most subjects at increased global risk of CAD have cholesterol levels between 4.0 and 6.5 mmol/dL, but a significant proportion of individuals have primary or secondary dyslipidaemic syndromes with characteristic abnormalities in the lipoprotein profile.
Normal ranges for plasma lipid levels
Total cholesterol |
4.0–6.5 mmol/L |
(150–250 mg/dL) |
LDL cholesterol |
<4.1 mmol/L |
(<160 mg/dL) |
HDL cholesterol |
0.8–2.0 mmol/L |
(30–75 mg/dL) |
Triglycerides |
0.8–2.0 mmol/L |
(70–175 mg/dL) |
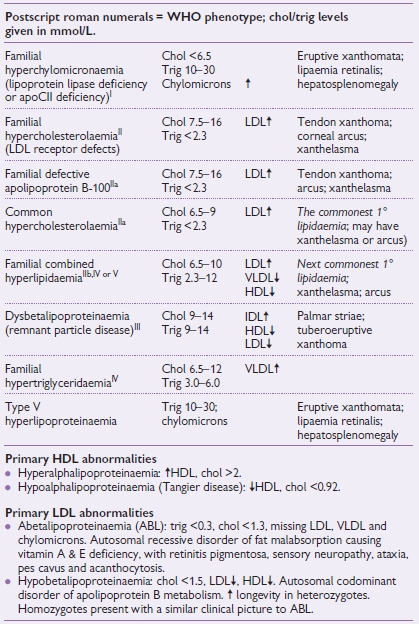
Table 5.4 Primary hyperlipidaemias
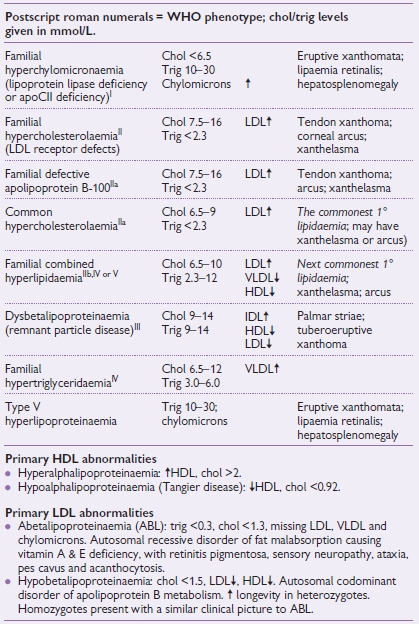
Chol = cholesterol; Trig = triglyceride.
Reproduced from Longmore M, Wilkinson I, Davidson E et al (2010). Oxford handbook of clinical medicine, 8th ed (2010). with permission from Oxford University Press. WHO = World Health Organization.
• Type II diabetes and obesity
b
• Cholestasis
• Alcohol abuse
• Drugs:
• anti-retroviral protease inhibitors
• thiazides
• oral contraceptive pill
• isotretinoin
• steroids
aCholesterol elevation.
bMinor elevation in cholesterol, but greater increases in atherogenic VLDL, chylomicron remnants, and triglycerides, as well as a fall in HDL.
Statins
(e.g. atorvastatin, fluvastatin, pravastatin, rosuvastatin, simvastatin)
Statins reduce cholesterol levels by inhibiting HMG-CoA-reductase, the rate-limiting enzyme in cholesterol synthesis. They also:
• increase clearance of circulating LDL by upregulating LDL-receptor expression.
• are extremely effective at lowering cholesterol levels; for example, the most potent statins, atorvastatin and rosuvastatin can more than halve LDL-C levels at higher doses.
• increase HDL and decrease triglyceride levels.
A significant evidence base has been built up over the past decade that strongly supports the widespread use of statins in primary and secondary prevention, and confirmed their safety.
• Data from large randomized clinical trials have shown a consistent reduction (around 25–30%) in the relative risk of major cardiovascular events with the use of atorvastatin, pravastatin, and simvastatin in both the primary (ASCOT, WOSCOPS (West of Scotalnd Coronary Prevention Study), HPS, CARDS (Collaborative Atorvastatin Diabetes Study)) and secondary prevention settings (MIRACL (Myocardial Ischemia Reduction with Acute Cholesterol Lowering), CARE (Cholesterol and recurrent Events), LIPID (Long-term Intervention with Pravastatin in Ischaemic Disease), 4S (Scandinavian Simvastatin Survival Study), HPS).
• In the first outcome study comparing two statins, the PROVE-IT (Pravastatin or Atorvastatin Evaluation and Infection Therapy) study showed that high-dose atorvastatin (80 mg) was more effective than pravastatin (40 mg) at preventing further major cardiovascular events during the first 2–3 years after presentation with an acute coronary syndrome.
• Typically, recommended evidence-based doses are simvastatin 40 mg nocte, pravastatin 40 mg od, and atorvastatin 10–80 mg od. Statins should not be prescribed to individuals with porphyria or severe liver or muscle disease, and caution is advised with their use in milder liver dysfunction, renal impairment, and in combination with fibrates.
Fibrates
(e.g. bezafibrate, ciprofibrate, fenofibrate, gemfibrozil)
• Fibrates improve the lipid profile by activating peroxisome proliferator-activated receptor alpha (PPAR-α), resulting in a mild lowering of TC and LDL-C.
• They also cause a significant reduction in triglycerides and increase in HDL.
• Subjects with combined hyperlipidaemia, or other reasons for a low HDL and/or high triglycerides, respond well to fibrates.
• The VA-HIT (Department of Veterans Affairs High-density Lipoprotein Cholesterol Intervention Trial) study showed that gemfibrozil (600 mmg bd) reduced major cardiovascular events in subjects with average cholesterol and low HDL (<1.0 mmol/L) levels.
• For the majority of patients, fibrates are typically recommended as second-line agents in patients who are intolerant of statins, particularly if they have low HDL or high triglycerides.
• The likelihood of liver or muscle side-effects is increased if a fibrate and statin are used in combination, and careful monitoring is recommended.
• The risk is lower if the statin is combined with fenofibrate than with other fibrates.
Anion-exchange resins
The agents colestyramine (4–8 g tds) and colestipol (5–10 g tds) bind bile salts in the small bowel. This inhibits their reabsorption, resulting in upregulation of the LDL receptor on hepatocytes and increased plasma cholesterol clearance. Although these drugs effectively lower cholesterol levels, most subjects experience intolerable gastrointestinal (GI) side-effects, limiting their widespread use. These drugs are generally recommended as second- or third-line therapy in subjects with hypercholesterolaemia.
Inhibitors of intestinal cholesterol absorption
The novel agent ezetimibe (10 mg od) binds to an intestinal cholesterol transport protein, which inhibits absorption. LDL-C is reduced by 15–20%. Ezetimibe is most effectively employed together with statin therapy in those patients who do not achieve cholesterol targets at higher statin doses, and is effective as monotherapy in those who are intolerant of statins.
Dietary plant stanols (3 g/day) can reduce LDL-C by up to 15%.
Nicotinic acid
Nicotinic acid (100–1000 mg tds, or 375–2000 mg modified-release (MR) preparation (Niaspan®) od) reduces hepatic VLDL synthesis and inhibits fatty acid release from adipocytes. HDL levels are significantly increased, and reduced hepatic synthesis results in a small reduction in LDL. Although particularly beneficial in mixed dyslipidaemias, use of the short-acting formulation has been limited by a high incidence of intolerable GI side-effects and facial flushing. The MR formulation is considerably more tolerable, and ongoing outcome studies should confirm the place of this agent in the preventive armamentarium.
Fish oils
Marine oil supplements containing high concentrations of omega-3 fatty acids are indicated for the treatment of severe hypertriglyceridaemia (Omacor® 4 capsules/day, Maxepa® 10 capsules/day). Omacor® (1 mg od, GISSI-P study) has a licence for secondary prevention post-MI, but the benefits observed with this dose do not seem to be due to lipid-lowering effects. An extensive clinical trial programme spanning a wide range of primary and secondary prevention settings should clarify the wider role of this drug in CAD prevention.
Therapeutic lifestyle changes (TLCs) are the first step in the treatment of dyslipidaemia. Moderate weight reduction (10% of body weight) improves the lipid profile and cardiovascular (CV) risk. The composition of the optimal diet is controversial.
General dietary recommendations include:
• reduced cholesterol and saturated fats (especially trans-fats)
• increased plant stanols, sterols, and soluble fibre
• adoption of Mediterranean diet.
Exercise should also be taken regularly.
Statin therapy should be initiated in all patients with established clinical atherosclerotic disease, including:
• CAD
• cerebrovascular disease
• renovascular disease
• peripheral arterial disease.
Current UK, European, and US guidelines also recommend statin therapy in subjects with:
• diabetes (CARDS, and subgroup analyses of HPS, ASCOT, and other major trials).
• CAD equivalent 10-year CV risk of ≥20%.
Although all of these patients should receive statins (unless contraindicated) regardless of their cholesterol level (HPS, ASCOT, CARDS), it is still important to measure lipid levels to ensure that subjects are responding appropriately to therapy and achieving targets for cholesterol <4.0 mmol/L and LDL <2.0 mmol/L. These targets are based on observations from clinical trials and cohort studies suggesting that ‘lower is better’ when it comes to cholesterol!
There is less outcome-based evidence informing us when to initiate drug therapy for isolated dyslipidaemia in the absence of other risk factors.
• Younger subjects without a family history of CAD or other risk factors should be considered for drug treatment if LDL-C>5.0 mmol/L (or total >7.0 mmol/L).
• Primary and familial hyperlipidaemias should be treated aggressively, particularly if there is a family history of premature CAD.
Approximately 2 million people in the UK currently suffer from diabetes mellitus (DM), the vast majority of whom have type 2 diabetes (>90%). Although diabetes is more common in older individuals, the incidence is increasing at a dramatic rate in all age groups, especially young adults, driven by the obesity ‘epidemic’. The prevalence of type 2 DM is also greater in black and South Asian individuals in the UK. Macrovascular disease is the most common cause of death in DM (>75%).
Mechanisms responsible for increased CV risk in DM
A complex mix of risk factors is typically present in patients with diabetes including:
• low HDL
• high triglycerides (VLDL and remnant particles)
• increased small, dense LDL
• moderate hypertension
• low-grade inflammation
• a procoagulant state (increased PAI-1, and platelet activation)
• increased oxidative stress
• increased levels of harmful advanced glycation end-products.
Conventional risk factors only account for a relatively small proportion (≈25%) of the increased risk observed in diabetes. Not only are subjects with diabetes more likely to suffer a major vascular event, they are also more likely to die from this event than if they did not have diabetes.
The atherosclerotic process tends to be more diffuse in individuals with diabetes, often affecting multiple vascular territories, making percutaneous and surgical revascularization more technically challenging and risky.
• Outcome is better when patients with diabetes and multivessel coronary disease undergo coronary artery bypass graft (CABG), rather than percutaneous revascularization (RITA (Radiofrequency Interstitial Tumour Ablation), BARI (Bypass Angioplasty Revascularization Investigation)).
• Data from large studies suggest that the outcome after percutaneous coronary intervention (PCI) in patients with diabetes is improved by use of drug-eluting stents as well as abciximab, a platelet glycoprotein (GP)IIb/IIIa antagonist.
• Visceral neuropathy is responsible for silent myocardial ischaemia, and reduced heart rate variability.
• Diabetic nephropathy further contributes to cardiac risk by increasing BP and causing deterioration in the lipid profile.
Blood glucose should be aggressively controlled by means of diet and exercise coupled with appropriate intensity of hypoglycaemic drug therapy.
• Target glycosylated haemoglobin (HbA1c) is ≥7%.
• Intense blood sugar control is better at reducing progression of microvascular disease and neuropathy than prevention of macrovascular events (UKPDS study).
• Aggressive blood pressure (UKPDS, HOT studies) and lipid management (CARDS, ASCOT, HPS) has a greater impact on prevention of CAD and stroke than tight glucose control, and reduces progression of nephropathy.
CV risk in diabetes is similar to that seen in patients with established CAD, at least after the disease has been present for several years. Because of their rapid progression of arterial disease, it is recommended that patients with diabetes receive aggressive preventive therapy with statins, aspirin, and inhibition of the renin-angiotensin system (see Table 5.5).
Table 5.5 Therapeutic recommendations for CV prevention in diabetes
|
Aggressive lifestyle ± oral hypoglycaemic therapy |
HbA1c ≤7% |
Statin therapy (regardless of baseline lipid levels) |
Cholesterol <4.0 mmol/L, or ↓>25% LDL <2.0 mmol/L, or ↓>30% |
Aggressive blood pressure control |
<130/<80 mmHg |
ACE-I or ARB in most, especially if there is evidence of nephropathy.
The metabolic syndrome is a term describing a frequently observed cluster of adverse factors within an individual.
• It is characterized by:
 http://www.bhsoc.org
http://www.bhsoc.org http://www.bhsoc.org
http://www.bhsoc.org www.bhs.co.uk
www.bhs.co.uk