Fig. 5.1
Schematic showing a left internal mammary artery (LIMA) being readied for anastomoses to the left anterior descending (LAD) artery. The myocardium is being stabilized by a suction based stabilizing device to facilitate the LIMA to LAD anastomosis
Fig. 5.2
Schematic showing the use of the left internal mammary artery as a bypass conduit to the left anterior descending artery as well as the right internal mammary artery to the posterior descending coronary artery. Additionally, an aortocoronary graft to a diagonal coronary artery is shown
Special Considerations in Choice and Technique of OPCAB
There are certain instances when OPCAB should not be the preferred method for revascularization [20]. Particular attention should be paid to the presence of and degree of mitral regurgitation. In the presence of greater than moderate mitral regurgitation, patients should have the mitral valve repaired or replaced [21]. A retrospective study compared 45 OPCAB versus 102 conventional CABG recipients with ejection fractions <30 % and although there were comparable incidence of adverse events, there were fewer grafts performed in the OPCAB group [22]. Similarly, another large study of 355 patients undergoing revascularization with an ejection fraction of ≤30 % showed that the number of grafts in the OPCAB group was 2.8, compared with 3.3 for the on pump group [15]. Once again, the importance of the completeness of revascularization cannot be understated.
A major deterrent to OPCAB surgery is the tolerance of patients to undergo the degree of cardiac manipulation and displacement that is necessary to perform total revascularization. Continual communication between the surgeon, anesthesiologist, nursing staff and perfusionist are vital to ensure smooth conduct and success of the operation. By nature, there will be alterations and swings in hemodynamics as the position of the heart is manipulated; however, careful alterations in position combined with cooperation and active participation of the anesthesiologist can minimize any systemic effect. There are some surgical tenants to adhere to in the performance of OCPAB surgery:
1.
Ensure effective and clear communication with the team of anesthesiologists, nurses and perfusionists as to the planned procedure, vessels to be grafted, alternate conduits and potential exit or bail-out strategies before the procedure.
2.
Try to minimize large manipulation of the heart by lifting the heart. Rather, use deep pericardial stay sutures allowing immediate assessment to whether or not the patient will tolerate off-pump surgery. If not, convert to early on-pump surgery as a strategy.
3.
Decide on the availability and suitability of conduits to be harvested and ensure the LIMA is the first graft for the LAD graft. Thereafter, proceed with a sequence to effect revascularization to the next most ischemic area. If another pedicle graft is used, such as the RIMA, perform this next. If aorto-coronary grafts are planned, try to perform the aortic anastomosis first so that when the distal anastomoses are completed, there is instant revascularization of that territory.
4.
If there are issues with rhythm, use atrial pacing or dual chamber pacing with ventricular pacing wires placed on both ventricles for hemodynamic stability (see Fig. 5.3).
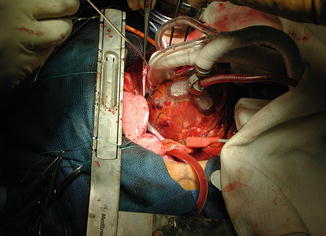
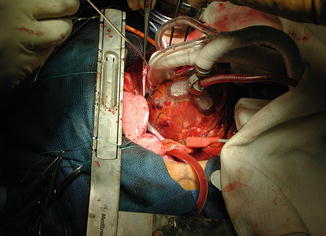
Fig. 5.3
Operative photograph showing facilitation of coronary grafting with heart stabilization with a suction device along with pacing. Note the pacing cable at the bottom of the picture
In patients with severe heart failure particularly with left main coronary disease, a useful technique of positioning the heart is by gently putting a glove filled with warm saline behind the heart positioning the LAD into the center of the surgical field and allowing easier access for grafting. The advantages of grafting the LAD first is establishing coronary flow through the septal perforators into the septum and providing better tolerance of the myocardium to further manipulation. There are certain instances when off-pump surgery may not be possible. These are encountered in patients with very stiff myopathic hearts that do not tolerate manipulation. In these cases, there are two options possible; either leaving the lateral wall revascularization to percutaneous intervention or using pump assisted, beating heart CABG (so called “pump assisted”) method. Discounting the inflammatory cascade from use of cardiopulmonary bypass, this may be the safest approach in sick patients with very low ejection fractions and profound left ventricular dysfunction. Another helpful alternative may be to use intra-aortic balloon counter pulsation to provide circulatory support for tolerance of OPCAB manipulation. In some studies of patients with an EF ≤25 %, one predictive factor of better outcome was pre-operative balloon pump insertion as compared to those who did not receive counter pulsation support. That being said, there is no doubt that the use of positioning and stabilizing devices has made a huge difference in the ability of surgeons to operate on vessels on the lateral and inferior wall (see Figs. 5.4 and 5.5). These suction, traction or pressure-based devices allow for stabilization of regions of the heart to allow for an operation. The most successful of these is the Medtronic Octopus, which is a suction based device initially developed at the University of Utrecht, Netherlands. Most off-pump procedures require a combination of a positioner and a stabilizer for each of the distal coronary anastomoses.
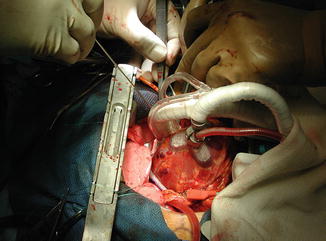
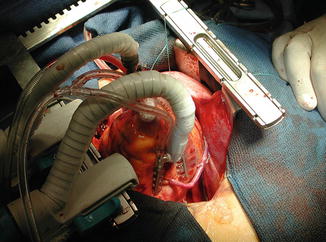
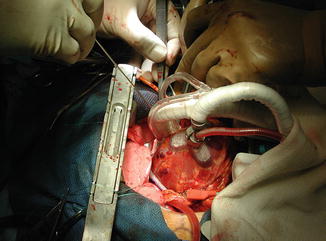
Fig. 5.4
Operative photograph showing an apical positioning device and a stabilizer (both suction based) used to expose the circumflex artery along the lateral wall of the left ventricle
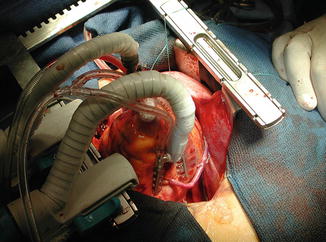
Fig. 5.5
Operative photograph showing a completed distal anastomosis to an artery on the inferolateral wall of the left ventricle
In general the OPCAB sequence of the operation follows a philosophy as outlined in the above tips. The goal should be for complete revascularization. In some instances positioning of the heart can be performed by opening of the pleura and allowing the right heart to be displaced into the right chest. This allows easy access to the circumflex vessels with minimal hemodynamic disturbance. However, this can be of concern if the LIMA has been grafted to the LAD as there may be too much tension to allow distraction of the heart and as such this needs to be considered in the pre-operative graft sequence planning. The proximal anastamoses can be performed to the aorta with a single partial clamp or by avoiding the clamp with the Heart String (which is a clampless way of providing a safe aortotomy) as depicted in Fig. 5.6.
Fig. 5.6
An illustration depicting a single saphenous vein graft to the left anterior descending artery using the proximal anastomotic technique of interrupted U-clips. This can be a particularly useful strategy in re-operative surgery where the proximal anastomosis can be performed without a clamp
In summary, OPCAB revascularization has been shown to be as effective and as safe as conventional coronary arterial bypass in experienced hands [23]. In fact, in patients with multiple risk factors, particularly those with heart failure with a low EF, OPCAB with complete revascularization can be more beneficial. To provide for reproducible and successful outcomes; however, the procedure needs to be performed by an experienced team. There needs to be a vigilant and responsive anesthesia team along with seamless communication between all team members. It is essential for the surgeons to inform the anesthesiologists about the number of grafts required, the sequence of grafting, the nature of the occlusion of the target vessel among other details of the proposed procedure.
Another useful technique, which is less invasive and mostly performed off-pump is the MICS (Minimally Invasive Cardiac Surgery) CABG. This involves a left minithoracotomy, with harvest of the left internal mammary artery through the lateral incision. The completion of the distal anastomoses, especially LIMA to LAD can be performed safely through this incision.
Figure 5.7 shows a LIMA to LAD anastomosis complete through this approach.
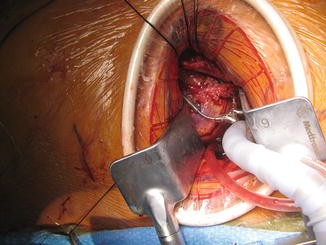
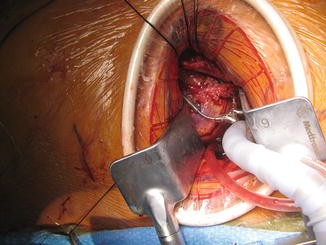
Fig. 5.7
Shows a LIMA to LAD anastomosis complete through this approach
An experience of over 100 patients with this technique in high risk patients over the past 3 years (personal experience of JR), showed satisfactory results with an acceptably low mortality of 2 % and low risk of peri-operative complications. This technique is technically more demanding and needs special equipment such as a specific retractor to facilitate LIMA harvest, custom made partial occluding clamps for the ascending aorta, long single shafted instruments to allow handling of the grafts, etc.
Figure 5.8 shows a trans-thoracic partially occluding Cygnet clamp used on the ascending aorta, in preparation for a proximal anastomosis of a vein graft.