Coronary Artery Anomalies
“The worst enemy of good is better”
Normal Coronary Artery Anatomy
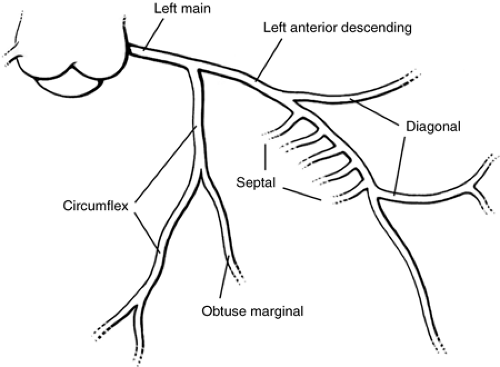
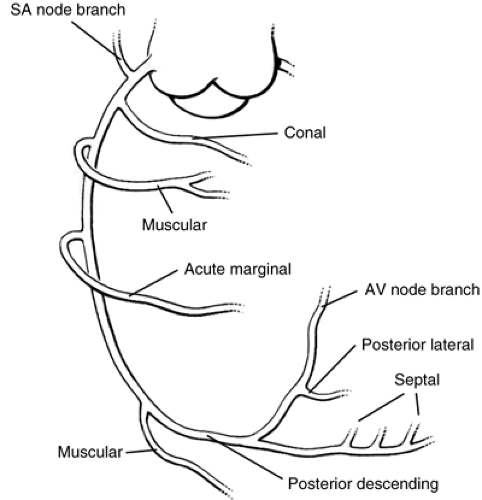
There are two major coronary arteries—left and right. The left main coronary artery divides into the left anterior descending and the circumflex coronary arteries (see Fig. 14-1). Branches of the left anterior descending coronary artery include the left conus, septal, and diagonal arteries. Branches of the circumflex coronary artery may include the sinus node artery, Kugel’s artery, marginal arteries, and the left atrial circumflex artery. Branches of the right coronary artery include the conal branch, the sinus node artery, an atrial branch, the right ventricular muscle branches (including the acute marginal branch), the posterior descending coronary artery, the atrioventricular node artery, and septal branches. The “dominant coronary artery” is the one giving rise to the posterior descending coronary artery. It originates from the right coronary artery in 80% of individuals and from the left coronary artery in 20% (see Fig. 14-2).
Anomalous Origin of the Left Coronary Artery from the Pulmonary Artery
Anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA) may be the most important coronary anomaly that pediatricians and pediatric cardiologists must deal with (see Fig. 14-3). Usually, the anomalous coronary artery arises from the left sinus of the pulmonary artery. A patient with ALCAPA may present with signs and symptoms of myocardial infarction and congestive heart failure in infancy, or the condition may be unassociated with myocardial infarction or symptoms of heart disease until detected serendipitously in adulthood or at autopsy. The age at presentation depends on the amount of collateral circulation between the right and left coronary artery systems. Patients with well-developed collateral connections may not develop myocardial infarction and may do well. Patients with poor collateral circulation can have a myocardial infarction, which is apparent at an early age.
In the immediate newborn period, pulmonary artery resistance and pressure are elevated, flow through the anomalously arising left coronary artery is antegrade from the pulmonary artery, and myocardial perfusion is adequate. As pulmonary artery resistance and pulmonary pressure decrease, antegrade flow of blood from the pulmonary artery through the left
coronary artery decreases. If there is inadequate collateral circulation between the right and left coronary arteries, myocardial infarction will occur. If collateral circulation exists, myocardial infarction may or may not occur, depending on the degree of retrograde flow from the right coronary system through the collateral circulation.
coronary artery decreases. If there is inadequate collateral circulation between the right and left coronary arteries, myocardial infarction will occur. If collateral circulation exists, myocardial infarction may or may not occur, depending on the degree of retrograde flow from the right coronary system through the collateral circulation.
Clinical features of ALCAPA in infancy are similar to those of myocarditis and cardiomyopathy, and the diagnosis of ALCAPA must be considered in the differential diagnoses of
unexplained congestive heart failure and poor left ventricular function, or mitral regurgitation in infancy. In teenagers and adults, the presence of ALCAPA may be suspected if there is unexplained cardiomegaly, mitral insufficiency, or a continuous cardiac murmur. Angina may occur secondary to coronary steal. A carefully performed and accurately interpreted echocardiogram will provide the diagnosis. However, the echocardiographer must be careful not to confuse the transverse sinus with the left coronary artery.
unexplained congestive heart failure and poor left ventricular function, or mitral regurgitation in infancy. In teenagers and adults, the presence of ALCAPA may be suspected if there is unexplained cardiomegaly, mitral insufficiency, or a continuous cardiac murmur. Angina may occur secondary to coronary steal. A carefully performed and accurately interpreted echocardiogram will provide the diagnosis. However, the echocardiographer must be careful not to confuse the transverse sinus with the left coronary artery.
The ideal treatment of ALCAPA is to detect the presence of the anomaly before myocardial infarction occurs and to establish a coronary system that prevents myocardial infarction. All cases in infancy, however, come to medical attention only after myocardial ischemia and infarction have occurred. Infants with ALCAPA and poor left ventricular function (ejection fraction <20%) have a poorer outcome than patients with an ejection fraction >20%.
Attempts to establish a two–coronary-artery system for patients with ALCAPA is indicated when the condition is diagnosed. There are several surgical procedures that have been described to establish the origin of both the coronary arteries from the aorta. It is unclear as to which procedure is superior, and the surgeon should use the technique with which he or she is most comfortable. Patients with ALCAPA and evidence of congestive heart failure benefit from treatment with digitalis and diuretics until surgery can be performed. Infants with evidence of acute myocardial infarction should be treated with oxygen, sedation, rest, and diuretics until surgery can be performed.
Anomalous Origin of the Left Coronary Artery from the Right Sinus of Valsalva
Anomalous origin of the left coronary artery from the right sinus of Valsalva is a rare but important malformation because it is associated with a significant risk of sudden death (see Fig 14.4). Patients in whom the aberrantly arising left coronary artery passes between
the aorta and the pulmonary artery appear to be at the greatest risk for sudden death. Sudden death is presumably due to myocardial ischemia as a result of compression of the left coronary artery between the aorta and the pulmonary artery, an elliptical rather than a circular os of the left coronary artery, and compromise of the lumen of the left coronary artery due to acute angulation near its origin.
the aorta and the pulmonary artery appear to be at the greatest risk for sudden death. Sudden death is presumably due to myocardial ischemia as a result of compression of the left coronary artery between the aorta and the pulmonary artery, an elliptical rather than a circular os of the left coronary artery, and compromise of the lumen of the left coronary artery due to acute angulation near its origin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree