Congestive Heart Failure with a Biventricular Pacemaker
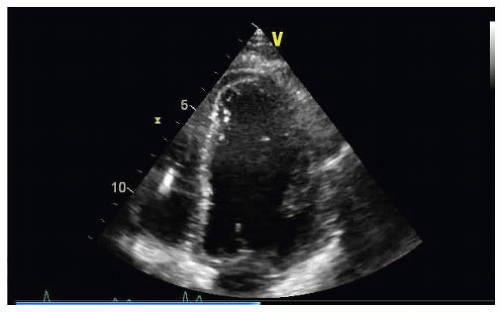
A 65-year-old woman with congestive heart failure and a biventricular pacemaker had two hospitalizations for heart failure in the past 6 months. She has a midpeaking systolic murmur heard best at the base. She has severe emphysema and is very frail.
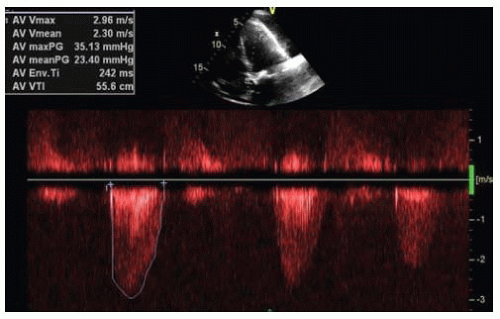
She is referred for evaluation of aortic stenosis and in consideration for percutaneous aortic valve replacement (Figs. 53-1 and 53-2 and Video 53-1).
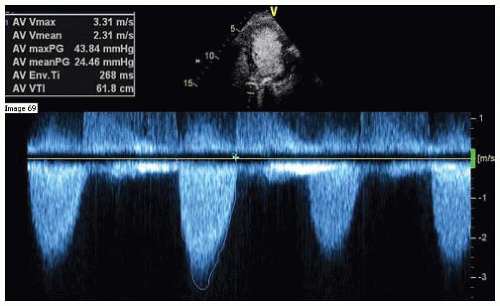
After echocardiogram contrast, the peak velocity increased from 296 cm per second to 331 cm per second, whereas the mean gradient increased from 23 to 24 mm Hg, and the aortic valve area calculates to 0.68 cm2 (Fig. 53-3).
In order to qualify for the percutaneous aortic valve, the peak velocity needs to be ≥ 4 m per second, and the mean aortic valve gradient needs to be ≥ 40 mm Hg.
QUESTION 1. Based on the clinical history and the data shown in Figures 53-1, 53-2 and 53-3 and Video 53-1:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree