Chapter 15 Congenital Heart Disease in Adults
Since the first surgical ligation of a patent ductus arteriosus by Gross in 1938, enormous advances have been made in the repair and palliation of congenital heart disease. Excluding bicuspid aortic valve, approximately 0.9% of infants are born with congenital heart disease; the incidences of the major types of defect are listed in Table 15-1. As a result of improvements in medical and surgical treatment, the population of adults with congenital heart disease has grown such that it now exceeds the population of children with congenital heart disease in many parts of the developed world.1,2
Table 15-1 Incidence of Congenital Heart Disease
| Lesion | Incidence/1000 Live Births |
|---|---|
| Ventricular septal defect | 3.57±2.9 |
| Patent ductus arteriosus | 0.80±1.4 |
| Atrial septal defect | 0.94±1.0 |
| Atrioventricular septal defects | 0.35±0.16 |
| Pulmonary stenosis | 0.73±0.73 |
| Aortic stenosis | 0.40±0.54 |
| Coarctation of the aorta | 0.41±0.25 |
| Tetralogy of Fallot | 0.42±0.19 |
| d-Transposition of the heart arteries | 0.32±0.12 |
| Hypoplastic right heart | 0.22±0.20 |
| Tricuspid atresia | 0.08±0.05 |
| Ebstein anomaly | 0.11±0.14 |
| Pulmonary atresia | 0.13±0.12 |
| Hypoplastic left heart | 0.27±0.22 |
| Truncus arteriosus | 0.11±0.07 |
| Double-outlet right ventricle | 0.16±0.10 |
| Bicuspid aortic valve | 13.56±13.05 |
| All congenital heart disease (excluding bicuspid aortic valve) | 9.60±7.40 |
Adapted from Hoffman JI, Kaplan S: The incidence of congenital heart disease. J Am Coll Cardiol 39:1890-1900, 2002.
CLASSIFICATION OF CONGENITAL HEART DISEASE
Surgically corrected or palliated congenital heart disease may be classified on the basis of whether there is a two-ventricle or a single-ventricle circulation (Table 15-2). With a two-ventricle circulation, the right ventricle is usually the pulmonary pump and the left ventricle the systemic pump, but in certain situations (e.g., atrial baffle repairs for transposition of the great arteries), the right ventricle is the systemic pump. For some defects a two-ventricle repair is not possible, and a staged palliation is performed; it results in a functionally single-ventricle circulation. The final stage of palliation is a Fontan-type operation, as explained later.
Table 15-2 Congenital Cardiac Defects in Which a Functionally Normal Circulation May Be Obtained vs. Defects Managed by Fontan-type Palliation
| Biventricular Repair |
| Ventricular septal defect |
| Atrial septal defect |
| Atrioventricular canal defect |
| Tetralogy of Fallot |
| Transposition of the great arteries |
| Truncus arteriosis |
| Anomalous pulmonary venous drainage |
| Valvular/subvalvular/supravalvular aortic stenosis |
| Interrupted aortic arch |
| Coarctation of the aorta |
| Ebstein anomaly of the tricuspid valve |
| Fontan Operation |
| Tricuspid atresia |
| Hypoplastic left heart |
| Pulmonary atresia with intact ventricular septum |
| Double-outlet left ventricle |
| Heterotaxy syndromes |
Multisystem Disease
Children who have undergone repair or palliation for congenital heart disease have, on average, lower IQs than their peers and are more likely to have developmental disabilities.3,4 Many adults with congenital heart disease were cyanotic for long periods of time during their childhoods; they may have experienced periods of circulatory compromise and may have undergone cardiopulmonary bypass during the formative years of that technology. In addition, some patients have syndromes in which congenital heart disease and mental disability are associated (e.g., Down syndrome). Anxiety and depression are also relatively common and may be exacerbated by admission to the ICU.
Cyanotic Heart Disease
The presence of right-to-left intracardiac shunting increases the risk for cerebral embolic events. Until recently, it was accepted that polycythemia itself was a risk factor for stroke. This belief led to the widespread use of phlebotomy to control hematocrit, typically to less than 55%. More recently, the detrimental effects of phlebotomy on oxygen delivery and iron stores have been appreciated,5 and many centers now reserve phlebotomy for patients with symptomatic polycythemia. The increased red cell turnover associated with polycythemia predisposes to the development of gallstones and gout. The risk for gout is increased by concomitant renal dysfunction and the use of diuretics.
General Perioperative Considerations
Most surgeries performed for congenital heart disease in adults are reoperations, and in many cases cardiopulmonary bypass times are long. Conduits from previous operations may be located directly behind the sternum and can be damaged during sternotomy. Postoperative problems involving excessive bleeding, coagulopathy, myocardial stunning, and pulmonary hypertension are not uncommon. Chronic volume and pressure overload of the cardiac chambers, along with scarring from previous surgeries, predispose to the development of ventricular dysfunction and arrhythmias. Poor nutritional state, chronic hypoxemia, and low cardiac output contribute to poor wound healing and the occurrence of nosocomial infection. Adults with congenital heart disease are at increased risk for developing endocarditis (see Table 10-7) and require antibiotic prophylaxis prior to certain invasive procedures (see Endocarditis Prophylaxis in Chapter 10). If these patients become febrile it is essential to draw blood cultures prior to commencing antibiotic treatment.
SPECIFIC CONGENITAL HEART DISEASES
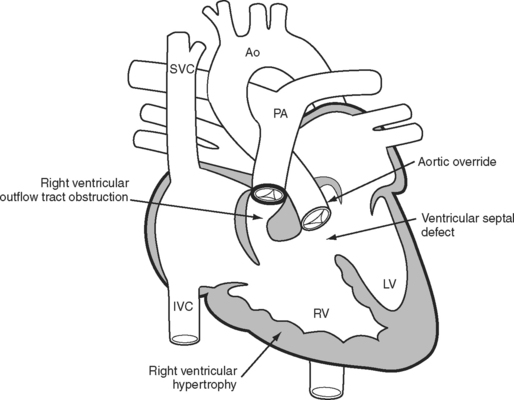
Tetralogy of Fallot
The essence of the tetralogy of Fallot (Fig. 15-1) is anterior displacement of the conal septum. This results in obstruction of the right ventricular outflow tract (RVOT) and a ventricular septal defect (VSD) and causes the aorta to override the crest of the ventricular septum. RVOT obstruction and right ventricular volume loading cause right ventricular hypertrophy, which is the fourth feature of the tetralogy. RVOT obstruction in the presence of a VSD causes a variable degree of right-to-left shunting and hypoxemia. Patients usually present in infancy with a murmur. If right ventricular outflow obstruction is severe, patients become cyanotic and may experience hypercyanotic “spells.”
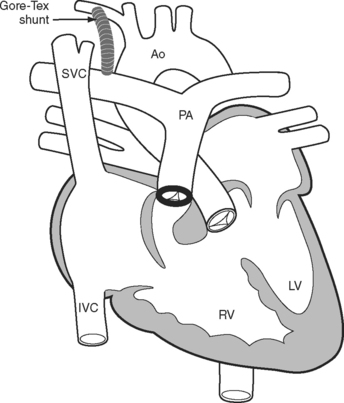
A tetralogy of Fallot was first palliated in 1944 by the classical Blalock-Taussig shunt. In this procedure, the subclavian artery is transected and anastomosed directly onto the pulmonary artery. Additional palliative strategies have included the Waterston and Potts shunts, in which the aorta (ascending or descending, respectively) is anastomosed side-to-side to a branch pulmonary artery. A modified version of the Blalock-Taussig shunt, in which a tube graft is used to connect the right subclavian artery to the right pulmonary artery (Fig. 15-2), is still performed to palliate lesions in which pulmonary blood flow is inadequate.
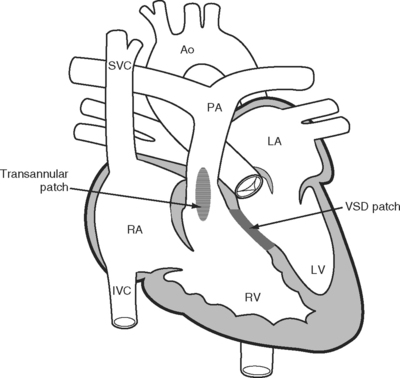
In the 1950s a more complete repair of the tetralogy of Fallot was developed. Repair involves patch closure of the VSD and reconstruction of the obstructed RVOT (Fig. 15-3); the latter is commonly achieved by placing a patch across the annulus of the pulmonary valve, rendering it incompetent. Patients usually undergo surgical correction in early childhood; depending on institutional practice and the presence and severity of cyanosis, it may have been preceded by a Blalock-Taussig shunt in infancy. Long-term survival rates are excellent. However, free pulmonary regurgitation causes right ventricular overload, which can eventually lead to right ventricular failure and ventricular arrhythmias. Patients who have undergone repair of a tetralogy of Fallot are at increased risk for sudden death, and those with ventricular tachyarrhythmias should be considered for internal cardiac defibrillators. Pulmonary valve replacement can prevent these problems, although there is disagreement about the optimal timing of surgery. Most centers use a combination of symptoms, measured exercise tolerance, and quantitative assessment of right ventricular function (usually by means of a magnetic resonance imaging scan) to establish the need for pulmonary valve replacement.