23 Congenital Complete Heart Block
I. CASE
A. Fetal echocardiography findings
1. The fetal echo reveals situs solitus of the atria, levocardia, and left aortic arch.
2. The ventricular rate is 58 bpm and the atrial rate is 150 to 160 bpm, showing complete atrioventricular (AV) dissociation (congenital complete heart block [CCHB]).
3. The intracardiac anatomy is normal, with normal cardiac axis and position and equal-sized ventricles but mildly increased heart size (cardiothoracic ratio = 0.37).
4. There is no evidence of endocardial fibroelastosis (echogenic walls of one or more of the cardiac chambers).
5. The ductal and aortic arches are of similar size, and both arches have antegrade flow.
6. The pulmonary venous flow pattern is normal.
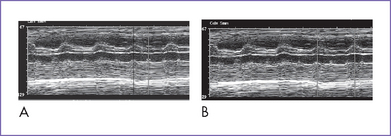
7. M-mode echocardiography confirmed the presence of atrial contractions that are at a normal rate and unrelated to a much slower ventricular rate (Fig. 23-1).
8. There is no evidence of valvar regurgitation (AV or semilunar). However, there is occasional intermittent tricuspid valve regurgitation related to the AV sequence. There is also a very low velocity diastolic regurgitation, which is normal in complete heart block (CHB).
9. The right ventricle (RV) and left ventricle (LV) Tei indices (myocardial performance index) are normal.
10. There is no evidence of heart failure.
11. The pulsatility index on the umbilical arterial Doppler (1.3) and middle cerebral artery Doppler (1.9) are normal.
D. Fetal management and counseling
1. Amniocentesis is not offered because the risk from amniocentesis is higher than the risk of abnormal karyotype in isolated CCHB.
a. Fetal drug therapy has been mainly directed toward three different features of the disease entity.
3. Follow-up included serial antenatal studies at 1- to 2-week intervals.
b. Fetus’s follow-up: A fetal ECG and general fetal surveillance should be provided every 1 to 2 weeks. The following should be serially evaluated:
E. Delivery
1. In isolated CHB, delivery should be near term (36 to 38 weeks) in a tertiary care center given the risk of hydrops fetalis and fetal demise from more severe bradycardia.
2. Premature delivery should normally be planned (for maternal or fetal indications) so that preparations can be made for care of the baby and mother.
F. Follow-up
1. Before the widespread application of pacemakers, infant mortality in isolated CCHB was estimated to be 8% to 16%.
2. The majority of newborns with isolated CCHB are hemodynamically stable.
3. Permanent pacing is required in a minority because of:
c. Mean heart rate less than 55 bpm.
d. LV dilation and mitral regurgitation.
2. Many asymptomatic patients reach adult life without pacing, but the risk of sudden death is 5% during adult life. For this reason, dual-chamber pacemaker implantation is increasingly advocated routinely in adolescence.
3. Following pacemaker implantation, the prognosis is good, with almost normal exercise tolerance in the majority.
4. Immune-positive patients can develop cardiomyopathy, requiring transplantation.
5. Rarely, LV function deteriorates in spite of adequate pacing. This could be explained by an accompanying myocarditis from the original insult, leading to cardiac dysfunction.
6. Pacemaker checks should be every 6 months in the first year and yearly thereafter.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree