What can you say about endocarditis in the setting of a PDA?
A.Vegetation is likely, and it will be seen on the pulmonary valve atresia (PA) end of the ductus arteriosus
B. Vegetation is likely, and it will be seen on the aortic end of the ductus
C. Vegetation is unlikely, but if present would be seen on the PA end of PDA
D. Vegetation is likely, and location is 50/50 on the PA end versus the aortic end
E. Vegetation is unlikely, but would be seen on the aortic end of the duct
21. Which of the following events is most responsible for early, functional closure of the ductus arteriosus?
A. Hemorrhage and necrosis in the subintimal region
B. Medial smooth muscle cell migration in the wall of the ductus
C. Equalization of pulmonary and systemic vascular resistance
D. Infolding of the endothelium
E. Thinning of the intimal layer
22. What is the theoretical benefit of ibuprofen over indomethacin for closure of PDA in premature infants?
A. Decreased risk of intraventricular hemorrhage
B. Decreased risk of pulmonary hypertension
C. Decreased risk of GI bleeding
D. Greater rate of ductal closure
E. Less effect on cerebral blood flow
23. A 2-week-old infant is found to have anomalous left coronary artery from the pulmonary artery (ALCAPA). Surgical correction is planned. What preoperative comorbidity has been found to be a risk factor for mortality and for late re-operation?
A. Mitral insufficiency
B. Tricuspid insufficiency
C. Aortic valve insufficiency
D. Pulmonary valve insufficiency
E. Patent foramen ovale
24. You examine a 17-year-old male with a 2-year history of progressive dyspnea on exertion and 2 months of orthopnea. Vital signs: pulse 80, BP 118/44, respiratory rate 24. Physical examination reveals a lift along the left sternal border and a continuous murmur with maximal intensity in the third to fourth intercostal space near the right sternal edge. On the basis of the available information, of the following diagnoses, which is most likely?
A. Sinus of Valsalva fistula from the aorta to the right atrium
B. Sinus of Valsalva fistula from the aorta to the left atrium
C. ALCAPA
D. Patent ductus arteriosus
E. Severe isolated aortic regurgitation
25. A 3-week-old infant has had several episodes of acute onset of agitation and crying. During these episodes, the baby is inconsolable. On examination, there is a high-frequency systolic murmur audible at the apex with radiation to the left axilla. Which of the following coronary artery anomalies most likely would be responsible for these symptoms?
A. Anomalous origin of right coronary artery from left sinus of Valsalva
B. Anomalous origin of left main coronary artery from right sinus of Valsalva
C. Anomalous origin of left coronary artery from the pulmonary artery
D. Anomalous origin of left anterior descending artery from the right main coronary artery
E. Origin of left circumflex coronary artery from right main coronary artery
26. Which of the following is true regarding aneurysms of the sinus of Valsalva?
A. The most common location is the noncoronary sinus
B. Men are as likely as women to develop a coronary sinus aneurysm
C. Concomitant VSD is seen up to 50% of the time
D. The most common site of rupture is into the left atrium
E. Most VSDs seen with coronary sinus aneurysms are paramembranous
27. A neonate presents at birth with high-output cardiac failure secondary a cerebral arteriovenous malformation (AVM). If left untreated, what is the risk of mortality during the first week of life?
A. <10%
B. 15%
C. 30%
D. 50%
E. 90%
28. Which of the following is true regarding pulmonary AVMs and hereditary hemorrhagic telangiectasia (HHT)?
A. Pulmonary AVMs in the setting of HHT tend to shrink as the patient grows older
B. In patients with pulmonary AVMs, cardiac output typically is twice that of normal patients
C.If there are multiple pulmonary AVMs, there is a >80% chance of the patient having HHT
D. Pulmonary AVMs have a different morphology in patients with and without HHT
E. Pulmonary AVMs are a rare cause of mortality in HHT
29. Which of the following statements is correct regarding transcatheter embolization of pulmonary AVMs?
A. To avoid device embolization, liquid adhesive is more effective than coil device closure
B. Embolization effectively prevent strokes and transient ischemic attacks, but not brain abscesses
C. Embolization effectively prevents brain abscess but does not prevent strokes
D. The goals of therapy are to occlude afferent arteries <3 mm in diameter and to decrease systemic arterial oxygen tension to <50 mm Hg
E. Embolization provides persistent relief of desaturation but not of orthodeoxia
30. Which of the following measurements has the best potential to distinguish a large AVM from a large PDA in a young infant?
A. Pulse pressure as determined by sphygmomanometry
B. Cardiothoracic ratio on plain chest x-ray
C. Systemic vein oxygen saturation measurements obtained during cardiac catheterization
D. QRS axis on electrocardiogram
E. Liver span by physical examination
31. An 11-year-old boy is evaluated for swallowing difficulty and moderate exercise intolerance. A barium esophagram shows evidence of anterior indentation, and pulmonary function testing shows evidence of obstruction. What is the most likely diagnosis?
A. Retroesophageal left subclavian artery
B. Pulmonary artery sling
C. Tracheo-esophageal fistula
D. Innominate artery compression of the trachea
E. Retroesophageal fistula of Phillips
32. A CT scan is done to assess a neck mass in a 3-year-old patient. This patient has no trouble swallowing and has no history of respiratory problems. The scan incidentally showed a right aortic arch with mirror image branching. What additional testing is warranted?
A. Barium swallow
B. Echocardiography
C. Bronchoscopy
D. Surgical referral
E. No further action needed
33. Which of the following typically results in a vascular ring?
A. Right aortic arch with retroesophageal innominate artery, left patent ductus arteriosus
B. Right aortic arch, retroesophageal left subclavian artery, no patent ductus arteriosus
C. Right aortic arch with mirror-image branching, left patent ductus arteriosus
D. Left aortic arch with cervical origin of right subclavian artery
E. Left aortic arch with retroesophageal right subclavian artery
34. An infant presents in acute cardiovascular collapse on day 3 of life. Physical examination reveals absence of all limb pulses with strong carotid pulses bilaterally. Echocardiogram is most likely to reveal which of the following?
A. Critical aortic stenosis
B. Interruption of the aortic arch, type A, with anomalous subclavian artery
C. Interruption type B
D. Interruption type B with anomalous subclavian artery
E. Right aortic arch with retroesophageal diverticulum of Kommerell
35. A 5-month-old girl presents with stridor and wheezing since birth. She has been treated with albuterol and inhaled steroids without any improvement. Her parents have noticed that she has been coughing and gagging since starting baby foods 2 weeks prior. Which of the following diagnoses is most likely?
A. Right aortic arch with retroesophageal diverticulum of Kommerell
B. Left aortic arch with retroesophageal diverticulum of Kommerell
C. Right aortic arch with retroesophageal left subclavian artery
D. Left aortic arch with retroesophageal right subclavian artery
E. Right aortic arch with retroesophageal innominate artery
36. Which of the following statements is true regarding anomalies of pulmonary venous return?
A. An untreated infant born with total anomalous pulmonary venous connection (TAPVC) has a 50% chance of surviving until the age of 1 year
B. The cardiothymic silhouette tends to be shifted leftward in Scimitar syndrome
C. Patients with cor triatriatum have enlargement of the right atrium and right ventricle
D.Normal p-wave size (<2.5 mm) on ECG effectively rules out cor triatriatum
E. Ventricular arrhythmias are common following TAPVC repair
37. A 3-year-old asymptomatic boy has a 2/6 systolic ejection murmur at the left upper sternal border and fixed splitting of S2. An echocardiogram reveals a sinus venosus ASD. This defect results from which of the following?
A. Deficiency of the septum primum
B. Deficiency of the septum secundum
C. Excessive resorption of the septum primum
D. Anomalous insertion of the superior pulmonary vein
E. Deficiency of the common wall of the superior vena cava and the pulmonary vein
38. What is the catheter course in Figure 2.2.?
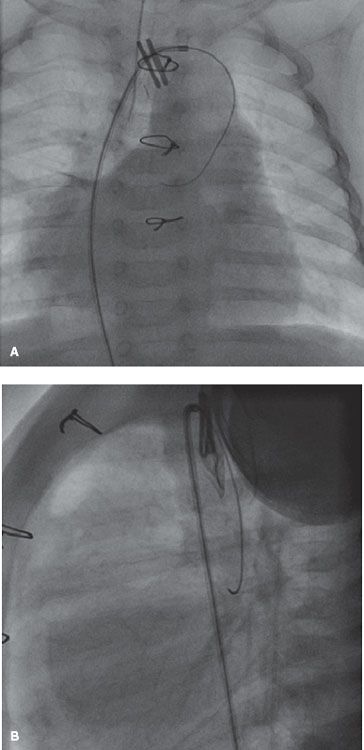
A. Aorta → right aortic arch → innominate artery → BT shunt → RPA
B. Aorta → right aortic arch → right sinus of Valsalva
C. Scimitar vein → right SVC → innominate vein → left SVC → coronary sinus
D. IVC → right atrium → SVC → innominate vein → left SVC → coronary sinus
E. IVC → right atrium → SVC → innominate vein → vertical vein → anomalous pulmonary venous confluence
39. A newborn is diagnosed with infradiaphragmatic TAPVC to the portal vein. Echocardiography demonstrates high-velocity, continuous, nonphasic venous flow in the anomalous vein. PGE1 has been started. The cardiorespiratory and metabolic states have been optimized. What is the best immediate plan of action?
A. Supportive therapy for 24 to 48 hours to allow PA pressures to fall before operation
B. Bedside balloon atrial septostomy
C. Cardiac catheterization to determine pulmonary vascular resistance (PVR) and to perform blade atrial septostomy if needed
D. Balloon dilation +/− stent placement in anomalous pulmonary vein
E. Immediate corrective surgery
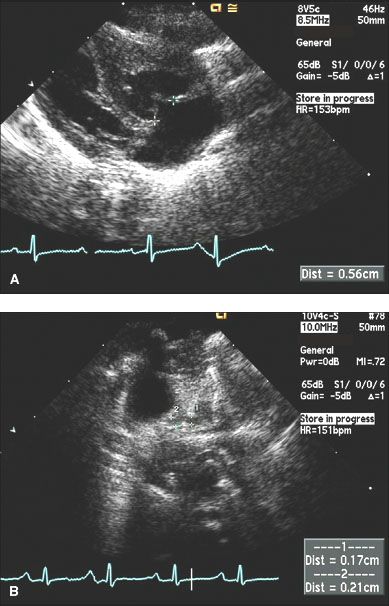
40. A 19-year-old female presents with a several month history of worsening breathlessness. Past medical history is significant for five episodes of pneumonia over her lifetime. Chronic medications include inhaled fluticasone, budesonide, and montelukast. She carries a rescue inhaler of albuterol. Physical examination reveals a RV heave, loud P2, and pulmonary systolic ejection click. There is a soft, blowing systolic murmur along the left sternal border. Echocardiography reveals the following (see Fig 2.3.):
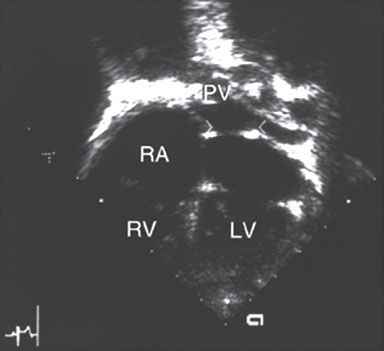
What is the most correct statement about this condition?
A. Surgical correction is universally futile
B. Medical management offers a better chance of 20-year survival than operative correction
C. Peri-operative risk is low
D. In patients who survive operative correction, prognosis is excellent
E. Atrial fibrillation is common
41. Which of the following is correct regarding anomalous drainage of the left pulmonary veins to the left innominate vein (LIV)?
A. The left lung drains typically by a left SVC
B. A primum ASD is common
C. The vertical vein represents a persistent embryological connection between the splanchnic plexus of the lung buds and the cardinal veins
D. This is a normal variant and found in 0.5% of the general population
E. This condition has never been described
42. A 3-year-old child has complex single ventricle, bilateral superior vena cava, and interrupted IVC with azygous continuation to the right SVC. At operation, he has construction of bilateral bidirectional superior vena caval-pulmonary anastomoses. Two months postoperatively his systemic arterial blood oxygen saturation is 87%, and he is doing well. Six months postoperatively his saturation is 82%, and he is doing well. Two years postoperatively his saturation is 75%, and he is a bit more fatigued. Which of the following is/are a contributing factor to his progressive desaturation unique to the operation he had?
A. Increased coronary sinus drainage
B. Increased pulmonary arteriolar resistance
C. Erythrocytosis
D. Pulmonary AV fistulae
E. Decreased chest wall compliance
43. An 8-year-old female with palpitations has an echocardiogram that demonstrates an outpouching originating in the coronary sinus that has a distinct neck and extends behind the LV. What is the most likely source of her palpitations?
A. RVOT-origin ventricular tachycardia
B. Accessory pathway-mediated SVT
C. AV nodal reentry tachycardia
D. Torsades de pointes
E. Brugada syndrome
44. A 14-day-old infant presents with irritability. He has been eating poorly due to tachypnea (RR = 80s) and he is 15% below his birthweight of 3216 g. Physical examination reveals tachypnea and a loud systolic murmur over his entire precordium. There is a soft low-pitched diastolic murmur at the apex. Distal pulses are slightly diminished. An ABG demonstrates pH = 7.27, pCO2 = 31, HCO3 =16 on room air. Echocardiogram reveals tricuspid atresia, d-TGA, and a moderately restrictive VSD. His aortic arch is moderately hypoplastic, though there is no evidence of a coarctation. Of the following procedures, what is the best initial surgical palliation option?
A.Modified Blalock–Taussig (BT) shunt only
B. PA banding only
C. Bidirectional cavopulmonary anastomosis
D. Anastomosis between MPA and ascending aorta [Damus–Kaye–Stansel (DKS)]
E. VSD closure + patch enlargement of LVOT (modified Konno)
45. Which of the following features would help distinguish Uhl anomaly from Ebstein’s anomaly?
A. The presence of significant cyanosis on physical exam
B. Large P-waves and diminished right ventricular voltages on ECG
C. Very thin, dysfunctional RV on echocardiography
D. Similar pressure wave contours in the RA, RV, and PA during cardiac catheterization
E. Ventricular endocardial potentials recorded past the expected anatomic tricuspid valve annulus during electrophysiologic assessment
46. An 11-year-old male with a history of pulmonary stenosis presents for evaluation. His blood pressure at rest is 100/70 mm Hg. Echocardiography reveals normal inspiratory collapse of his IVC. The following Doppler-derived velocities are obtained (at rest):
Tricuspid regurgitation (CW) = 3.5 m/s
Infundibulum (PW) = 2 m/s
RVOT (CW) = 4 m/s
Assume RA pressure is 6 mm Hg. Using traditionally accepted Doppler-derived criteria to determine severity, what degree of pulmonary stenosis is present in this patient?
A. Trivial
B. Mild
C. Moderate
D. Severe
E. Not enough information provided
The following clinical scenario pertains to the next two questions:
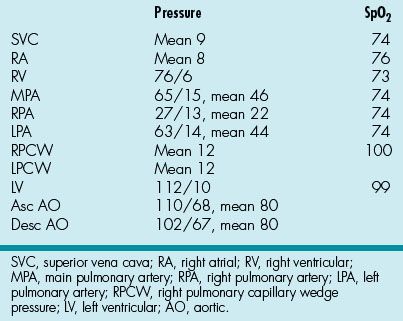
A 1-day-old term newborn is admitted to the NICU with cyanosis and a murmur. He is diagnosed with critical pulmonary stenosis and a moderate PDA. Percutaneous pulmonary valvotomy is performed. Cardiac hemodynamics obtained during the catheterization are shown in Table 2.1
Table 2.1 Cardiac Hemodynamics Obtained during Catheterization
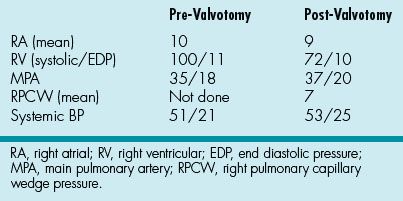
That night, the baby continues to have low oxygen saturations in the mid-80s despite being mechanically ventilated and on PGE1. On examination, there is a grade 4/6 late-peaking harsh systolic murmur at the left upper sternal border, which is increased in intensity from his admission exam, and a new, soft diastolic murmur. Blood pressure is 52/24. Blood gas reveals a base deficit of −2.
47. Which of the following would be the next best step?
A. Urgent repeat percutaneous valvotomy
B. Urgent open pulmonary valvotomy
C. STAT echocardiogram
D. Increase the PGE dosage
E. Continued close observation
48. Which of the following is the most likely underlying cause of his desaturation?
A. Pulmonary valve stenosis
B. Infundibular obstruction
C. Right to left shunting across the PDA
D. Undiagnosed VSD
E. Severe pulmonary regurgitation
49. You are performing an echocardiogram on an asymptomatic 4-month-old girl referred for a murmur. You note discrete stenosis of the proximal LPA, measuring 2 mm. The distal LPA is 6 mm. The RPA is 8 mm. The pulmonary valve and MPA are normal. There are no atrial or VSDs. Peak velocity across the LPA stenosis is 2.0 m/s. RVSP is estimated to be 25 mm Hg. There is mild RV hypertrophy. Which of the following statements is true?
A. The degree of LPA stenosis is mild
B. RVSP is likely underestimated considering the degree of LPA narrowing
C. Invasive pressure measurements would be likely to show an MPA to LPA gradient that is much higher than that estimated by Doppler flow velocity.
D. If angioplasty is performed, a 6- to 8-mm balloon should be used
E. The risk of re-stenosis after angioplasty is approximately 3% to 5%
50. A newborn infant is cyanotic, and echocardiography reveals pulmonary artery atresia with intact ventricular septum. The right ventricle is bipartite and quite small. The baby is receiving PGE-1. Which of the following is the next step in the management of this patient?
A. Balloon atrial septostomy
B. Surgical outflow tract reconstruction
C. Cardiac catheterization and angiography
D. Cardiac CT scan
E. Cardiac MRI
51. Which of the following anatomical substrates most likely predicts a successful decompression of the RV using radiofrequency ablation and balloon pulmonary valvotomy in patients with pulmonary atresia with intact ventricular septum?
A. Unipartite RV
B. Muscular pulmonary atresia
C. RV-dependent coronary circulation
D. Severe tricuspid stenosis
E.Tricuspid valve Z score = −2
52. The angiogram demonstrated in Figure 2.4. is performed in a 9-month-old boy with pulmonary atresia and intact ventricular septum.
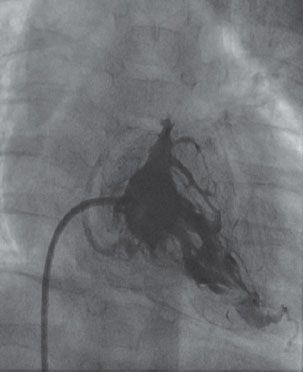
Which of the following operations is best for this patient?
A. Bidirectional Glenn alone
B. RV to PA conduit with a bidirectional Glenn
C. RV to PA conduit alone
D. Pulmonary valvotomy alone
E. Pulmonary valvotomy with a bidirectional Glenn
53. For the above patient, a takedown of his BT shunt is performed along with the placement of an RV to PA conduit. That evening he develops congestive heart failure (CHF). Which of the following ECG findings would you most likely see in this patient at this time?
A. Complete heart block
B. Left bundle branch block
C. ST segment elevation in I, aVL
D. ST segment elevation in II, III, aVF
E. Increased voltages in V1, V2, V3
54. You are seeing a 4-day-old infant with cyanosis. Echocardiography reveals PA with intact ventricular septum. There is significant subpulmonary (infundibular) obstruction. The RV appears tripartite but severely hypoplastic. By echocardiography, there is no evidence of RV-dependent coronaries. You are planning eventual biventricular repair beginning with a surgical pulmonary valvuloplasty and RVOT patch enlargement. What is the next step in surgical planning?
A. Go to surgery without further testing
B. Cardiac catheterization with hemodynamic study only
C. Catheterization with hemodynamic assessment and RV angiography
D. MRI with RV volume quantification
E. Biopsy of myocardium to evaluate for spongy myocardium and/or endocardial sclerosis
55. A newborn is found to have cyanosis shortly after birth. A holosystolic murmur is heard and PGE-1 is started. An echocardiogram is performed (Fig 2.5.):
Color flow Doppler fails to show antegrade flow in the MPA. The ventricular septum is intact. Which of the following is true regarding neonates with this form of congenital heart disease?
A. Coronary artery perfusion is wholly RV dependent in about 45% of cases
B. Pulmonary blood flow most often is supplied by aortopulmonary collaterals
C. This form of congenital heart disease is more common in males
D. By definition, the right ventricle is always bipartite
E. A main pulmonary trunk almost always is present
56. A 3-year-old boy has pulmonary atresia with VSD. He has a history of hypoplastic central pulmonary arteries and multiple major aortopulmonary collateral arteries (MAPCAs), with multiple surgeries including a central shunt as well as right and left unifocalization surgeries. He is admitted for complete repair. Following reconstruction of the central confluence, placement of an RV-PA conduit, takedown of two MAPCAs, and VSD closure, he does not tolerate coming off bypass. His blood pressure is 84/60 mm Hg on multiple pressors. His saturations are 87% on 100% oxygen. His RV pressure is 69/15 mm Hg. TEE demonstrates patency of the conduit. What is the best course of action?
A. Placement of ECMO until hemodynamics improve
B. Reinstitution of bypass, takedown of RV-PA conduit and placement of a central shunt
C. Replacement of the RV-PA conduit with a larger conduit
D. Treatment with nitric oxide to improve PVR
E. Re-opening the VSD
57. An 11-year-old male with history of PA-VSD is status post a BT shunt on day of 10 and is also status post multiple unifocalization procedures. He is in the operating room for a complete repair. The surgeon has completed the operation. You are performing an echocardiogram. You note that the VSD is now closed and the RV-to-PA conduit has laminar flow by color Doppler. The estimated RV systolic pressure is 80 mm Hg. Biventricular function appears reasonable. You see that the radial arterial pressure tracing is 100/50 mm Hg. You advise the surgeon to:
A. Do nothing further
B. Replace the conduit with a smaller one
C. Replace the conduit with a larger one
D. Re-open the VSD
E. Place a BT shunt in addition to what has been done already
58. A 4-month-old infant with pulmonary atresia and VSD undergoes complete repair, including unifocalization, RV-PA conduit and closure of the VSD. Before sternal closure in the operating room she becomes hypotensive. Systemic arterial pressure is 65/45 mm Hg. She is edematous with hepatomegaly. TEE reveals RV hypertrophy and moderately decreased biventricular systolic function. She has mild/moderate tricuspid regurgitation with a velocity of 3.5 m/s. Which of the following interventions is most urgent at this time?
A. Milrinone
B. Leave the chest open and return to the ICU
C. Re-open the VSD
D. Placement of a bidirectional Glenn
E. ECMO
59. A neonate with pulmonary atresia-VSD undergoes heart catheterization. The angiogram in Figure 2.6. is obtained.

What is the primary source of pulmonary blood flow in this patient?
A. Ascending aorta
B. Descending aorta
C. Patent ductus arteriosus
D. BT shunt
E. Right subclavian artery
60. In a patient with pulmonary atresia and VSD, where does the proximal His bundle run relative to the VSD?
A. Along the posteroinferior rim of the VSD on the left ventricular side
B. Along the posterosuperior rim of the VSD on the right ventricular side
C. Along the anterolateral rim of the VSD on the left ventricular side
D. Along the anteromedial rim of the VSD on the right ventricular side
E. Not enough information provided
61. A 12-year-old patient with unrepaired TOF presents to clinic for pre-operative evaluation before a planned complete surgical repair. Physical examination reveals severe cyanosis with marked clubbing of the fingers. Cardiac examination reveals normal S1, single S2, with a grade 2/6 systolic ejection murmur at the left upper sternal border. There is also a soft continuous murmur over interscapular area. Echocardiography demonstrates severe right ventricular hypertrophy, anterocephalad malalignment of the conal septum, and a large perimembranous VSD with an overriding aorta. Owing to difficult visualization of the pulmonary artery anatomy, a cardiac catheterization is planned for the next morning at 8:30 am. Which of the following should be done to decrease the chance of a hypercyanotic spell in the morning?
A. Make the patient NPO after midnight and start an IV at 7:00 am
B. Use a general anesthesia inducing agent that decreases systemic vascular resistance more than PVR
C. Make the patient NPO after midnight, perform phlebotomy to decrease Hgb to < 14 before starting the IV
D. Start an esmolol drip as soon as the procedure starts
E. Make the patient NPO after midnight, start IV fluid when NPO starts, and use a topical anesthetic such as EMLA before attempting vascular access
62. A 17-year-old female with a history of TOF with left aortic arch presents with progressive dyspnea on exertion. She describes a history of multiple operations including an RV-PA conduit revision 2 years ago. As part of her evaluation, cardiac catheterization is performed, from whence the data in Table 2.2 are obtained.
Table 2.2 Cardiac Catheterization Data
On the basis of the information, which of the following is most likely to be true?
A. She would benefit from sildenafil
B. She would benefit from closure of her left to right shunt
C. She should have a conduit revision
D. Her symptoms are primarily related to diastolic dysfunction
E. She has a history of a Waterston shunt
63. A 6-day-old male infant presents with cyanosis and tachypnea. An echocardiogram confirms the diagnosis of TOF with absent pulmonary valve. He is in moderate respiratory distress. His heart rate is 190 bpm, respiratory rate is 55/minute, and his ABG shows PaO2=67, PaCO2=38, pH=7.41, Bicarb=20, and an oxygen saturation of 84%. What should be done next in an attempt to alleviate his respiratory distress?
A. Inhaled albuterol
B. Intubation and mechanical ventilation
C. IV solumedrol
D. Emergent surgical repair of his congenital heart disease
E. Placement in prone position
64. A 3-day-old male infant presents to the emergency department with cyanosis. He was diagnosed prenatally with TOF. He was born at home at 35 and 4/7 weeks of gestation. Over the first 48 hours of life, his color was good and he was nursing effectively. However, over the past 2 to 4 hours, he appeared progressively blue. At the time of presentation, his saturations are 60% to 65%, and he appears dusky. He is becoming more dusky. On examination, he has no appreciable murmur. A UVC has been placed. What is the best next step in management?
A. Echocardiogram to ascertain whether his prenatal echo had the correct diagnosis.
B. Hyperoxia test to try and ascertain if he has a pulmonary component of his cyanosis.
C. Emergent surgical repair
D. IV prostaglandin
E. IV morphine to encourage left-to-right shunting across his VSD
65. A 6-day-old male infant presents with a murmur and cyanosis. His saturation is 69% and his cuff blood pressure is 65/37. An echocardiogram reveals the following: TOF; severe infundibular obstruction (narrowest diameter 2 to 3 mm), a bicuspid pulmonary valve measuring ~5 mm at the annulus; almost entirely right-to-left shunting at the VSD with a peak Doppler VSD velocity of 2.5 m/s; accessory tricuspid valve tissue prolapsing into the VSD during systole; and a tricuspid regurgitation velocity of 4.5 m/s. He has an enlarged coronary sinus draining a left SVC. He has a large conal branch from his right coronary artery. Among the findings below, which feature is the most unusual in patients with TOF?
A. Large conal branch
B. Left SVC
C. Restrictive VSD
D. Pulmonary hypertension
E. Predominant right-to-left shunting through the VSD
66. A 3-week-old infant presents with tachypnea and poor oral feeding. Her prenatal screening ultrasound was suggestive of truncus arteriosus, but she never underwent a formal fetal echocardiogram. Today, vital signs are as follows: P = 140, BP = 80/35 mm Hg, RR = 60, O2 saturation = 93% (room air). Cardiac examination reveals an active precordium, normal S1, single S2 with systolic ejection click, and grade 2/6 systolic murmur at left-mid sternal border. When the baby is quiet, a soft continuous murmur becomes apparent in the back. Which of the following statements is correct regarding this scenario?
A. The continuous murmur strongly suggests a diagnosis of truncus arteriosus
B. The continuous murmur is the result of truncal valve stenosis and regurgitation
C. Physical examination findings suggest a diagnosis of pulmonary atresia with VSD more than truncus arteriosus
D. Physical examination findings suggest a diagnosis of pulmonary atresia with intact ventricular septum more than truncus arteriosus
E. The presence of an apical diastolic murmur in this patient suggests anatomical mitral valve stenosis
67. Which of the following statements is correct regarding coronary artery anatomy in truncus arteriosus?
A. The posterior descending coronary artery arises from the left circumflex artery (left coronary dominance) in <3% of patients
B. The left anterior descending artery is relatively large and displaced rightward
C. The conus branch of the right coronary artery is usually small
D. The left coronary artery arises from the pulmonary trunk in ~40% of patients
E. Left coronary usually arises from the left posterolateral truncal surface
68. An 8-year-old female from Mongolia presents for surgical consideration of her cyanotic congenital heart disease. Echocardiogram reveals type I truncus arteriosus with a large VSD. The atrial septum is intact and there is trivial TR. Heart catheterization is performed, whereupon the data in Table 2.3 are obtained:
Table 2.3 Heart Catheterization Data
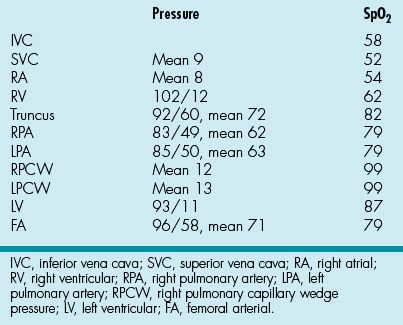
Her systemic cardiac index = 4.0 L/min/m2. Which of the following is true regarding this patient?
A. No corrective intervention is indicated (palliation only)
B. She should undergo closure of her VSD and placement of an RV-PA conduit
C. Decision about whether or not to repair her lesions should be deferred until her hemodynamics are reassessed while she receives 100% oxygen
D. She should be listed for cardiac transplantation
E. She may benefit from balloon angioplasty of her pulmonary arteries
69. A neonate presents with cyanosis. He is found to have type II truncus arteriosus with a bicuspid truncal valve and right aortic arch. He has a large secundum ASD and a left SVC draining into the coronary sinus. There is moderate RVH with normal biventricular function. Among the findings in this patient, which is most common among patients with truncus arteriosus?
A. Type II truncus
B. Bicuspid truncal valve
C. Interrupted aortic arch (IAA)
D. ASD
E. Left SVC
70. You are performing an echocardiogram on a cyanotic neonate. You note a large, thickened semilunar valve that is mildly incompetent and appears to originate from both RV and LV with a large outlet VSD. The pulmonary arteries originate separately from the ascending aorta. You also note interruption of the aortic arch. Which of the following is this baby most likely to have?
A. Bicuspid truncal valve
B. Right aortic arch
C. Absent ductus arteriosus
D. Absent left or right pulmonary artery
E. Chromosome 22q11 deletion
71. A cardiac catheterization is performed on an 18-month-old male with unrepaired truncus arteriosus. He has a moderate ASD with no ductus arteriosus. The data in Table 2.4 are obtained.
Table 2.4 Cardiac Catheterization Data
If pulmonary blood flow is 5.0 on room air and 6.8 on 100% FiO2, what course of treatment is recommended for this patient?
A. Home oxygen therapy with repair in 1 to 2 years
B. Pulmonary artery banding
C. Surgical repair now
D. Listing for heart-lung transplant
E. Home oxygen (palliation only)
72. You are seeing a new patient in clinic with a history of truncus arteriosus. On auscultation, you hear a split second heart sound at the left sternal border. What is the most likely cause of the splitting of S2?
A. Referred tricuspid valve closure sound
B. Ejection click after truncal valve opening
C. Delayed closure of some of the cusps of the abnormal truncal valve
D. Increased flow across the mitral valve
E. Pulmonary artery ostial stenosis
73. You diagnose truncus arteriosus in the fetal period. After delivery at 38 weeks through spontaneous vaginal delivery with no complications, you perform confirmatory echocardiography. You are able to visualize the pulmonary arteries. The PAs are widely patent with laminar, increased flow. The PAs arise from a common trunk. The aortic arch is right-sided. The truncal valve is quadricuspid and has moderate-to-severe regurgitation. There are no other complicating factors. You are confident that your imaging windows were sufficient. What is the best treatment plan for this newborn infant?
A. Perform bilateral BT shunts in first week of life, then a bidirectional Glenn at 4 to 6 months, with Fontan completion at 2 years of life
B. Diuretics, digoxin, and afterload reduction for first 2 to 4 months if tolerated. Plan complete repair at 6 months (divide MPA from aorta, aortic valve repair, homograft conduit from RV to MPA)
C. Band the LPA in first 2 weeks of life, then manage medically until 4 to 6 months, when complete surgical repair can be more safely performed
D. Complete repair by 1 month (divide MPA from aorta, aortic valve repair, homograft conduit from RV to MPA)
E. Complete repair within the first 72 hours of life using aortic valve tissue prosthesis (divide MPA from aorta, aortic valve tissue prosthesis, homograft RV-MPA conduit)
74. In the setting of parachute mitral valve, which of the following papillary muscle arrangements is the most common?
A. Absence of both papillary muscles
B. Absence of the anterolateral papillary muscle
C. Absence of the posteromedial papillary muscle
D. Presence of two separate papillary muscles
E. Presence of two fused papillary muscles
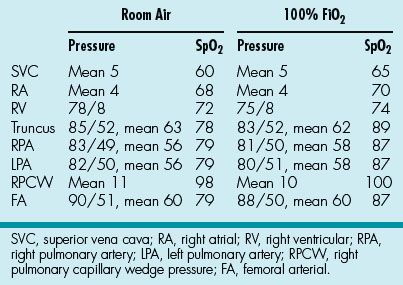
75. A 1-month-old infant presents with tachypnea and poor feeding. A cardiac murmur is heard and an echocardiogram is performed (Fig. 2.7).
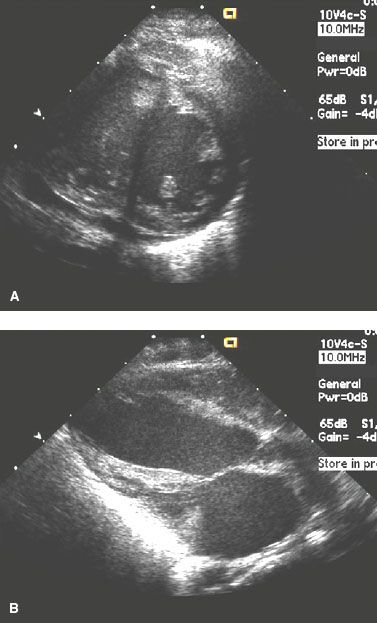
The echo also suggests moderate mitral inflow obstruction (mean gradient = 8 mm Hg), severe MR, and LA and LV enlargement. Which of the following is the most likely diagnosis?
A. Double orifice mitral valve
B. Mitral arcade
C. Supramitral ring
D. Parachute mitral valve
E. Cor triatriatum
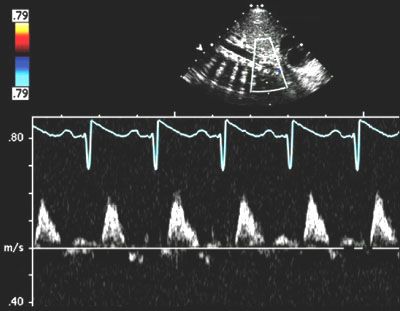
76. A 4-year-old female presents with tachypnea and heart failure and is found to have mitral stenosis. She undergoes a trans-atrial repair of her mitral valve. Attempts to extubate on post op day 2 are unsuccessful. Her examination is significant for a soft holosystolic murmur at the apex, a loud P2 and a liver edge palpable 3 cm below the costal margin. An echocardiogram documents a mitral inflow mean gradient of 5 mm Hg and the pulmonary vein Doppler flow pattern in Figure 2.8.
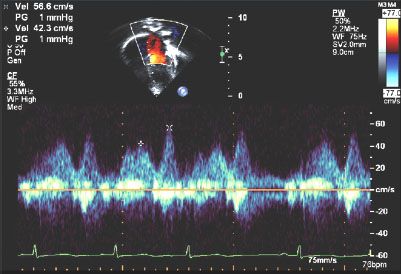
The RV is moderately dilated with moderately decreased systolic function, which is not significantly changed from her pre-operative echo. Which of the following is the most likely cause for the patient’s symptoms?
A. Pulmonary hypertension
B. Residual mitral stenosis
C. Unrecognized supramitral ring
D. Pulmonary vein stenosis
E. Right coronary infarction
77. Unlike the cleft in atrioVSDs, which of the following is true about the isolated cleft of the mitral valve?
A. Is more truly a commissure as there is typically a papillary muscle associated with it
B. Causes more severe regurgitation
C. Is associated with both mitral stenosis and regurgitation
D. Is directed anteriorly towards the LVOT
E. Is not associated with atrial or VSDs
78. A 4-month-old infant is found to have congenital mitral insufficiency without stenosis due to a cleft in the anterior leaflet. By echocardiography, the valve appears repairable. The LVEDD is at the upper limit of normal. The LA has mild-moderate enlargement. LV EF = 60%. CXR reveals a somewhat enlarged cardiac silhouette. ECG is normal for age. Vital signs are normal. What is the best next step in management?
A. Furosemide and captopril
B. Propranolol and verapamil
C. Propranolol and captopril
D. Surgical referral
E. No therapy for now
79. A 16-year-old female presents for clearance to participate in competitive volleyball. She has a history of vasodepressor-vasovagal syncope following a stressful event at school 2 years prior. Evaluation at that time revealed a normal physical examination and normal ECG. Now, physical examination while supine reveals a systolic click shortly after S1 at the apex. With sitting, you note that the click moves toward S1 and is followed by a I/VI systolic murmur at the apex that ends before systole concludes. These findings prompt an echocardiogram which reveals bileaflet mitral valve prolapse (MVP) with moderate mitral regurgitation, with a left ventricular EF of 52%. She then has a 24-hour ambulatory ECG monitor that shows frequent sustained SVT. Her height-to-weight ratio is 0.44 kg/cm. Along with her MVP, which of her findings would be indication to restrict her from competitive volleyball?
A. Degree of mitral regurgitation
B. Left ventricle ejection fraction
C. History of syncope
D. Ambulatory ECG results
E. Her height-to-weight ratio
80. An infant is diagnosed with critical aortic stenosis and resultant LV hypoplasia. According to the “Rhodes criteria” and other literature, which of the following echocardiographic criteria would indicate that the patient would benefit more from a Norwood-type palliation as opposed to a two-ventricle repair?
A. LV long axis to heart long axis ratio of 0.9
B.Aortic root diameter of 8 mm (4 cm/m2)
C.Indexed mitral valve area of 8 mm (4 cm/m2)
D.LV mass index of 10 g (50 g/m2)
E. Antegrade flow in the ascending aorta
81. A 17-year-old female immigrant presents with a 3-month history of progressive dyspnea on exertion. She had a childhood history of rheumatic fever, but she cannot remember the details of her underlying cardiac status except the painful IM antibiotic every month. On examination, she appears comfortable. Palpation on her chest reveals no thrill. Her S1 and S2 appear normal. There is a grade 3/6 harsh systolic murmur audible along the mid-left sternal border down to the apex. There is no diastolic murmur or click. During auscultation, she has a few premature ventricular contractions. The systolic murmur becomes much louder in intensity following the extra beat. What is the most likely etiology of these physical examination findings?
A. Tricuspid valve regurgitation
B. Mitral regurgitation
C. Pulmonary valve stenosis
D. Subaortic stenosis
E. Innocent murmur
82. Interventional aortic balloon valvuloplasty is indicated in which of the following patients? All patients have bicuspid aortic valves except where indicated, and all have undergone cardiac catheterization.
A. Asymptomatic 2-year-old male with normal growth who has a peak-to-peak gradient of 50 mm Hg
B. Asymptomatic 20-year-old female who is planning to become pregnant and whose peak-to-peak gradient is 40 mm Hg
C. Asymptomatic 18-year-old boy who wants to play American football with a peak-to-peak gradient of 45 mm Hg
D. A 1-day-old newborn with a unicommissural aortic valve who has an LV EF of 45% and a peak-to-peak gradient of 30 mm Hg
E. Asymptomatic 20-year-old male with a normal ECG whose peak-to-peak gradient is 55 mm Hg
83. Which of the following statements is true regarding diastolic function in children with aortic valve stenosis?
A. The echocardiographically derived ratio of early mitral inflow velocity (E) to early diastolic mitral annular velocity (E’) correlates with LVEDP
B. Measurement of mitral annular systolic velocity (S’) by tissue Doppler imaging (TDI) demonstrates systolic short-axis dysfunction
C. Longitudinally oriented fibers are present primarily in the subepicardial region
D. The subendocardium is remarkably resilient to ischemia
E. Transverse axis dysfunction typically precedes long-axis dysfunction
84. A 15-year-old male with congenital aortic valve stenosis presents for interval follow-up. He underwent successful balloon dilatation at age 4 years with a reduction in Doppler peak instantaneous gradient from 87 mm Hg to 22 mm Hg. He has been followed annually for the past 10 years without further intervention. BP is normal. By echo, his peak gradient today is 42 mm Hg (mean 26 mm Hg). There is mild LV hypertrophy without mid-cavitary obstruction. He is interested in playing hockey for his high school team. Try-outs start in 8 weeks. His is asymptomatic. What is the best recommendation?
A. Start low-dose lisinopril, then allow participation if BP remains acceptable
B. Balloon dilate the valve, then allow to play after 6 weeks
C. Replace the valve with a homograft, then allow to play
D. Replace the valve with a mechanical valve and prohibit participation
E. Perform an exercise ECG and reassess
85. You are asked to consult on a term neonate with a murmur. He has a harsh 2–3/6 systolic ejection murmur. He has good distal pulses and perfusion with no increased work of breathing. Echo reveals a thickened bicuspid aortic valve with a velocity across the valve of 3.0 m/s and a PDA. Which of the following is true?
A. Mild congenital subaortic stenosis, as a rule, rapidly progresses in the first few months of life
B. The amount of endomyocardial fibroelastosis (EFE) is independent of the degree of stenosis
C. Significant retrograde diastolic flow in the distal arch from the PDA is consistent with severe stenosis
D. Echo-derived pressure gradient is independent of other hemodynamic variables, such as pre-load and afterload
E. Relative to balloon valvuloplasty, open surgical valvotomy results in a greater degree of aortic regurgitation
86. A 10-day-old male infant presents to the emergency room with vomiting and respiratory distress. Pregnancy history was uncomplicated, and the infant was delivered vaginally at term. The patient was dismissed from the hospital at day 2 of life. At day 4 of life, the patient began to have some difficulty with feeds. He was slow to feed due to fast breathing. No color changes were noted with feeds. His PO intake and urine output had been decreased over 24 hours before presentation.
Vital signs at the time of presentation are: HR = 169, respiratory rate = 70, BP (right arm) = 90/60 mm Hg, right leg = 70/30. On physical examination, there are no facial dysmorphic features. The skin is mottled and pale. There is a hyperactive RV impulse, normal S1, single S2 with S3 gallop, and a soft systolic murmur at apex. Brachial pulses are normal, but femoral pulses are absent bilaterally. There are bilateral subcostal retraction. The liver is palpated 4 cm below restrictive cardiomyopathy (RCM). Extremities are cool.
ECG and CXR are obtained (Fig. 2.9).
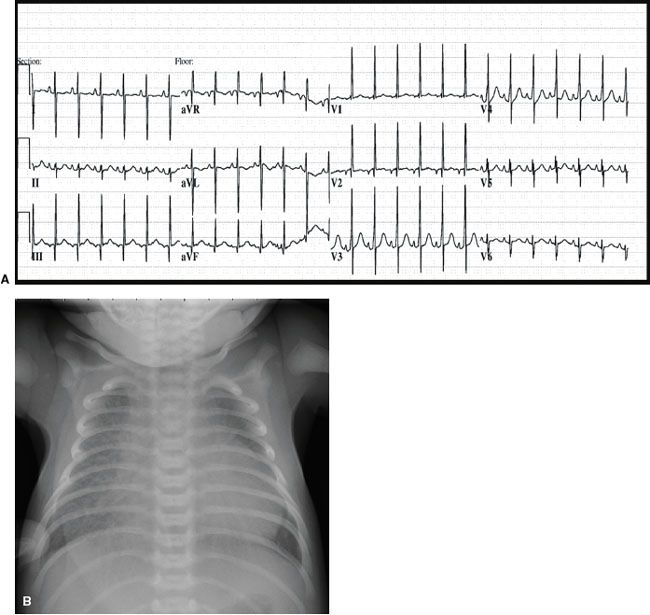
What would be the appropriate next step in management?
A. Perform an echocardiogram to get definite diagnosis
B. IV access and give Lasix
C. IV access and start dobutamine
D. IV access and start PGE1
E. IV access and give sodium bicarbonate
87. While IV access is being obtained, emergent echocardiography is performed on the baby. Pulsed wave Doppler interrogation of the abdominal aorta is performed (Fig. 2.10).
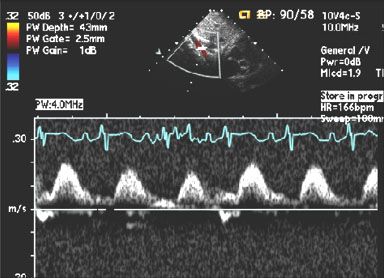
Which of the following statement is true?
A. The Doppler profile suggests that surgical correction is unlikely to be necessary before 12 months of age
B. A bicuspid aortic valve is unlikely to be associated with this defect
C. Severe aortic regurgitation is likely to be present
D. VSD is commonly associated with this defect
E. Secundum atrial septal defect is the defect responsible for this clinical presentation
88. A 1-year-old child is referred for a murmur. She is asymptomatic. Her BP in the left arm = 104/56, left leg = 84/50. Echocardiogram confirms isolated coarctation of the aorta. When do you recommend the patient have surgical repair?
A. Age 2 to 3 years
B. Age 6 to 8 years
C. Age 12 to 14 years
D. Only operate if systolic pressure gradient >50 mm Hg
E. Only operate if symptoms develop, such as lower extremity claudication
The following clinical stem is used to answer the next three questions (questions 89 to 91).
A 9-day-old female presents to the ED with respiratory distress. She is pale, irritable, and diaphoretic. RR 80; HR 210; 4-extremity BP: right arm 48/32, left arm 68/34, right leg 47/31, left leg 48/31. Auscultation reveals a gallop rhythm. A grade 2–3/6 murmur is heard at the upper left sternal border, at the base, and in the left interscapular area posteriorly. The murmur is heard throughout systole and disappears in early diastole. Moderate hepatomegaly is noted. She has widely spaced nipples and a webbed neck. She undergoes an echocardiogram.
89. What is the echocardiogram most likely to reveal?
A. Mitral valve stenosis with moderate MR
B. ALCAPA
C. Isolated large outlet VSD with severe pulmonary valve stenosis
D. Isolated severe coarctation of the aorta
E. Coarctation of the aorta with anomalous aortic arch branching pattern
90. The above patient undergoes an echocardiogram following initiation of PGE1. The pulsed wave Doppler profile in Figure 2.11. is obtained. What is the most likely explanation for the tracing?
A. Aortic arch is normal
B. Ductus arteriosus is open
C. Cardiac output is extremely low
D. Pulmonary hypertension is present
E. Thrombus is present in the descending aorta
91. The above patient undergoes genetic testing. What is the most likely result?
A. 45, XO genotype
B.JAG1 gene mutation
C.PTPN11 gene mutation
D.46, XY/47, XYY mosaicism
E.TBX5 gene mutation
92. A 12-year-old female with who is status post repair (end-end anastomosis) of coarctation of the aorta as a young child now complains of headaches with exercise. A neurological work up including an MRI/MRA of her neck and head are negative. She is noted to have exercise hypertension on a bicycle exercise test. Further cardiology evaluation with an echocardiogram reveals no significant anatomical obstruction of the aorta. Which intervention or next step in evaluation would be beneficial to help relieve her exercise hypertension?
A. Nothing, wait and watch
B. Heart catheterization with possible stent placement as needed
C. CT angiography to further evaluate aorta
D.β-Blocker pharmacotherapy
E. Nephrology consult
93. A 5-day-old term infant is 2 days status post a Norwood procedure with an RV-PA shunt (Sano) for hypoplastic left heart syndrome. His chest is closed and he is mechanically ventilated. Over the past 6 hours, you have noticed worsening acidosis and increasing hepatic enzymes. Creatinine has increased from 0.4 to 0.8. Urine output has been adequate. His vital signs are: HR 145 BP 60/38 RR 24 (all ventilator-initiated). His Sp02 is 77% on 30% FiO2; hemoglobin is 12 g/dL. Echocardiogram shows patent surgical connections with normal RV function. Which of the following interventions is most likely to improve this patient’s clinical status?
A. Start milrinone
B. Increase inspired oxygen to 50%
C. Start nitric oxide
D. Transfuse 15 mL/kg packed RBCs
E. Increase ventilator rate to 30/min
94. A neonate is diagnosed with d-TGA with an anterior malalignment VSD and subaortic stenosis. Which of the following is most likely to be concurrently found in this patient?
A. Coarctation of the aorta
B. Peripheral pulmonary stenosis
C. Pulmonary atresia
D. Mitral arcade
E. Ebstein’s anomaly
95. Which of the following statements is correct regarding pathologic anatomy of complete d-TGA with an intact ventricular septum?
A. There is complete resorption of subaortic conus
B. Ventricular septum is relatively sigmoid in shape rather than straight
C. Functional (dynamic) subpulmonic obstruction from bulging of ventricular septum into LVOT usually occurs immediately after birth
D. Sinus node and AV nodes are typically in their normal locations
E. LV mass usually regresses much faster in d-TGA with IVS compared with d-TGA with VSD
96. A neonate is found to have d-TGA with VSD and ASD. The VSD is nonrestrictive, but there is severe LVOT obstruction. The patient’s oxygen saturation is 68% on room air. What is the most appropriate initial surgery/procedure for this patient?
A. Jatene arterial switch with Lecompte maneuver
B. Mustard operation
C. BT shunt
D. LVOT balloon arterioplasty
E. PDA stent
97.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


