Diameter (mm)
1–5
6–9
10–14
15–19
≥20
Number of nodules
103
38
9
6
6
Percentage (%)
63.6
23.5
5.6
3.7
3.7
3.1 Positive Results
Fifty nine individuals were classified as positive (nodule of 5 mm or larger in diameter). Based on the radiologic appearance after baseline screening, ten individuals were admitted to the hospital for diagnostic evaluation. Three of those patients underwent a bronchoscopy with biopsy, as a result of which two cases of NSCLC were diagnosed (Figs. 1 and 2). Nonetheless, no malignant cells were detected in the biopsy specimen of one of the patient, but because of the clinical and radiological changes he was referred to a PET CT in which a malignant tumor with metastases was confirmed. The patient was admitted to the surgical ward, where he underwent mediastinoscopy, with the histopathological result of adenocarcinoma. Another patient underwent lobectomy and Stage I NSCLC was diagnosed (squamous cell carcinoma) (Fig. 3). In another six patients, no sign of malignancy was found. A PET scan was performed in all of them, with negative results. These patients were referred for further evaluation (LD-CT in 6 months). Two of them most likely had post-tuberculotic changes in the lungs (Fig. 4).



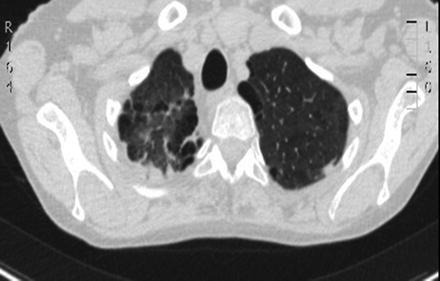

Fig. 1
Non-small cell cancer of right lung

Fig. 2
Pulmonary metastases of non-small cell lung cancer

Fig. 3
Squamous cell lung cancer, Stage I, right middle lobe
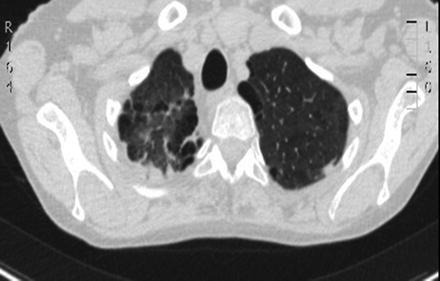
Fig. 4
Post-tuberculotic changes in upper lung lobes
Forty nine patients were referred for a repeat scan after 3 months. Thirteen of them were non-compliant and did not turn up for the test. No significant growth was observed in 27 of the remaining 36 cases; a repeat scan after 12 months was preplanned. Six of these patients were referred for a PET scan and all the results were negative. Three patients were submitted to a control examination within 3 months after completing a full course of antibiotics. A progression of the disease was noted in one of the patients, after receiving complete antibiotic therapy. This patient and two others with changes in the upper part of the lungs were admitted to the hospital. They underwent bronchoscopy during which the material for a cytologic examination was collected. The examination results were negative and the patients were referred for a PET scan.
3.2 Semi-positive result
A hundred and three patients with a semi-positive result from baseline screening were referred for annual screening. Only did 25 of them turn up for a repeat scan. Among all the annual screenings, no significant growth was reported. No further action was taken.
4 Discussion
Lung cancer is still the leading cause of death due to cancer. The prognosis in lung cancer is very poor with a 5-year survival rate of about 10–15 %. This has remained unchanged over the last two decades. In Poland every year approximately 3,000 out of 20,000 new cases of primary NSCLC are operated on, with a resection rate of 17 % (Chabowski et al. 2008). Trials evaluating chest X-rays and sputum cytology as screening modalities were conducted in the 1970s, but they did not show a reduction in lung cancer mortality (Kubik and Polak 1986). The major breakthrough was the National Lung Screening Trial (NLST) that demonstrated a 20 % reduction in mortality rates in a low-dose CT group compared to the X-ray group (National Lung Screening Trial Research Team 2011). In this trial the number of patients that had to be screened to prevent one death was 320.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


