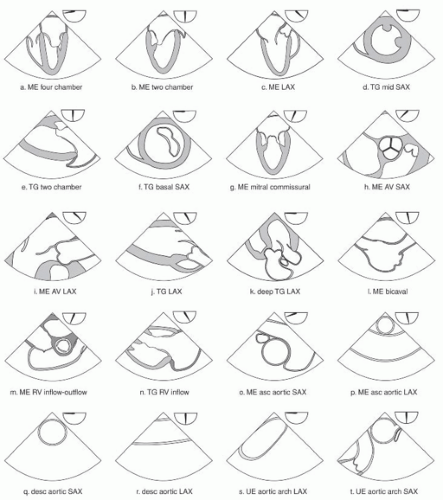
The comprehensive exam recommended by the SCA/ASE guidelines consists of 20 views.
Screen for esophageal disease BEFORE inserting the TEE probe.
NEVER apply excessive force when inserting or manipulating the TEE probe.
Examine each structure with multiple views.
An abbreviated eight view exam may achieve the basic applications of perioperative TEE.
Ultrasound images are obtained by the electronic sweeping of the ultrasound beam through an arc with a pie-shaped image created with the apex corresponding to the position of the transducer.
The heart is anterior to the esophagus so proximal to the esophagus appears as posterior structures (e.g., left atrium) and anterior structures (e.g., left ventricle apex) are at the bottom.
Intraoperative echo can be performed with transesophageal, epicardial, or epiaortic approaches.
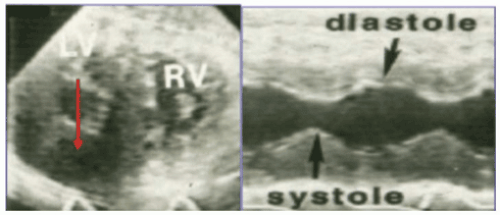
A one-dimensional view of structures along the path of a single beam
Useful for measuring and timing events within the heart throughout the cardiac cycle.
The density and position of the scan line is updated 1,000 times/s (red line in Fig. 5-1).
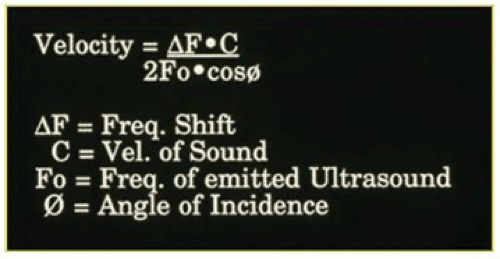
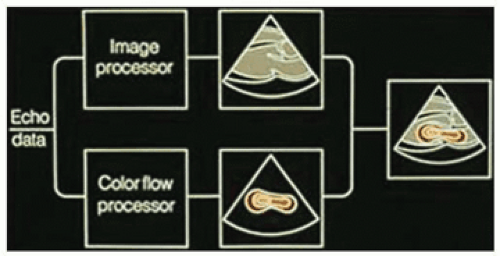
Used to assess the flow of blood by measurement of BF velocity and direction (Fig. 5-2).
When the beams are transmitted and strike a moving red blood cell they are reflected in different directions. The difference between the reflected signal and the transmitted signal creates a Doppler phase shift.
Assessment of valves (and their repairs), blood flow patterns, left ventricular function, myocardial ischemia, endocarditis (and its complications), septal closures and repairs of congenital heart disease, air removal after open heart surgery, endovascular stent deployment and dissection, evaluation for hypotension, evaluation of aorta for cannulation, detection of intracardiac masses, thrombus and vegetations, measurement of cardiac output
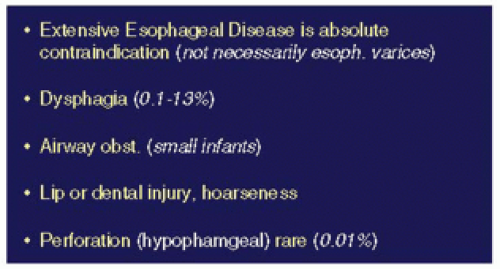
Absolute contraindications (TEE in an anesthetized patient)
Esophageal disease
Relative contraindications
TABLE 5.1 GUIDELINES FOR TEE | ||||||
|---|---|---|---|---|---|---|
|
Twenty views of the heart and great vessels (Fig. 5-6).
Individual anatomic variation must be considered, and adjustments made.
An OG tube should be inserted, suctioned, and withdrawn prior to inserting the probe.
All examinations should be as complete as possible to obtain the recommended images.
Superior means toward the head and inferior toward the feet.
Posterior means toward the spine and anterior toward the sternum.
Right and left denote the patient’s right and left sides.
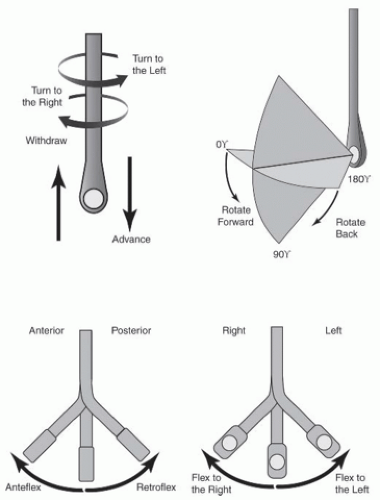
Pushing the probe is done to advance the transducer, and pulling the probe is withdrawing.
Moving the probe clockwise toward the patient’s right is called turning to the right.
Moving counterclockwise is called turning to the left.
Axial rotation from 0 degrees toward 180 degrees is called rotating forward.
Rotating in the opposite direction toward 0 degrees is called rotating back.
Flexing the probe tip anteriorly (the large control wheel) is called anteflexing (Fig. 5-7).
Flexing the tip posteriorly is called retroflexing.
Flexing the tip to the patient’s right is called flexing to the right, to the patient’s left is called flexing to the left (Fig. 5-7).
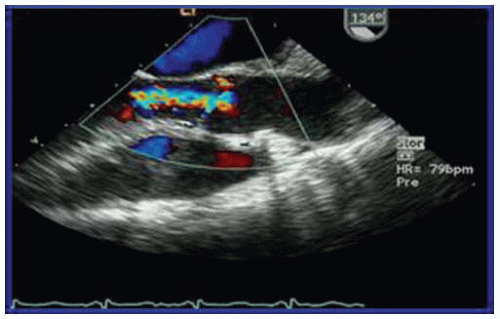
Begin by identifying the aortic valve short-axis view and exploring the anatomy of the aortic valve (2D echo) and flow (color Doppler and m-mode). This view is usually obtained at the mid- to upper esophageal level (insert the probe about 20 to 25 cm) and then apply approximately 20 to 40 degrees rotation of the multiplane transducer.
This image plane is useful for assessing AV anatomy, aortic alve area with
planimetry and aortic insufficiency with color M-mode (
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree