FIGURE 12-1 Radial artery avulsion with 8F guiding catheter. (Courtesy of G. Barbeau.)
TABLE 12-1 Complete List of Published Vascular Complications with Radial/Ulnar Access
• Accelerated atherosclerosis
• Arteriovenous fistula
• Cardiovocal syndrome
• Compartment syndrome
• Distal finger ischemia/necrosis
• Pseudoaneurysm
• Radial/ulnar occlusion
• Reflex sympathetic dystrophy
• Retrograde perforation/dissection
• Retropleural hematoma
• Severe spasm
• Wrist, forehand, arm, pectoral hematoma
A recent meta-analysis of randomized studies reported an incidence of major vascular complications of 1.4% (49/3507 cases) with transradial approach (TRA) compared to 3.7% (131/3514 cases) with the femoral approach, a relative reduction of 63% (OR 0.37, 95% CI 0.27–0.52, P < 0.0001).37 Initial and more recent data have generally reported a frequency of radial access-site failure of less than 5%.38 Reasons associated with access-site failure include puncture failure, spasm and radial, brachio-cephalic trunk abnormalities, or excessive loops, and can be additionally related to lack of experience, small artery size, or transient or permanent reduction in vessel diameter. In a large series of all-comers undergoing transradial PCI in an experienced radial center, Abdelaal et al. reported a primary failure rate of 2.7% and a crossover rate to femoral approach of 1.8%. Independent predictors of radial failure included female sex, prior coronary artery bypass grafting (CABG), and cardiogenic shock.39 Importantly, patients who had radial access failure had more ischemic, bleeding, and vascular complications.
Access-site failure may also result from anatomical variations, severe tortuosities, or loops in radial or brachial arteries. The incidence of these variations in vessel anatomy is close to 5%.40,41 Most of the time, operators manage to negotiate them using hydrophilic wires, 0.014-inch angioplasty wires, or hydrophilic catheters (see Chapter 7). It is advised to perform an angiography of the arm in case of difficulty of wire or catheter advancement, as failure to identify the problem may lead to vessel perforation or dissection. Radial or brachial artery dissections can produce marked angiographic images, but it should be emphasized that they represent retrograde dissections. Therefore, it is worth attempting to carefully recross them with a soft 0.014-inch angioplasty wire. If this attempt is successful, the catheter will usually seal the dissection or perforation, and there will be no clinical consequence for the patient. In some cases, operators have proceeded with placement of long sheath, long balloon inflation, or even covered stent implantation for refractory bleeding. Failure to recognize these perforations might be dramatic as slow and delayed intramuscular bleeding may potentially lead to compartment syndrome.
The incidence of compartment syndrome after intramuscular bleeding or vascular damage is extremely low but should be promptly recognized, as it may lead to devastating consequences (Fig. 12-2). One series reported acute compartment syndrome in five cases out of 250 patients treated (2%), while a more recent study reported two cases in 51,296 procedures (<0.01%).42 Open surgical fasciotomy can be avoided if effective preventative measures are employed as soon as local bleeding is suspected. These include (1) stopping intravenous anticoagulant therapy, (2) controlling the pain and blood pressure, and (3) using transient external compression with a blood pressure cuff.43
TABLE 12-2 Comparison of Femoral and Radial Complications
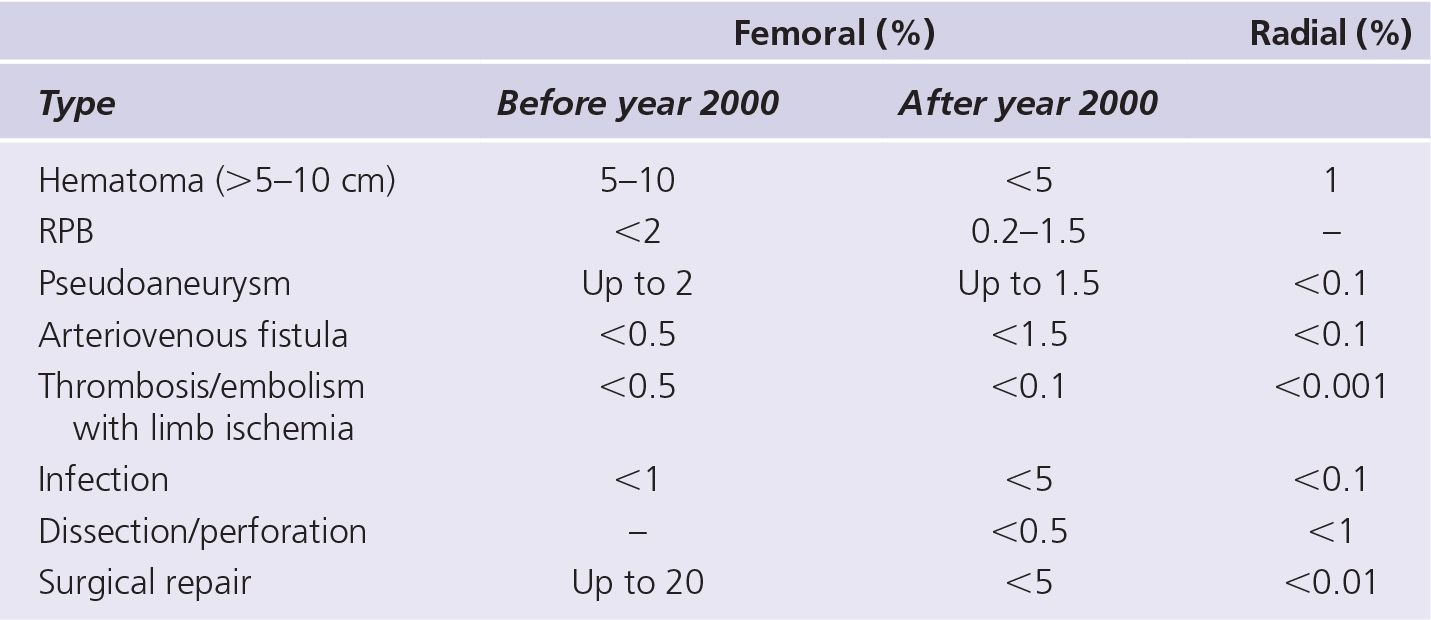
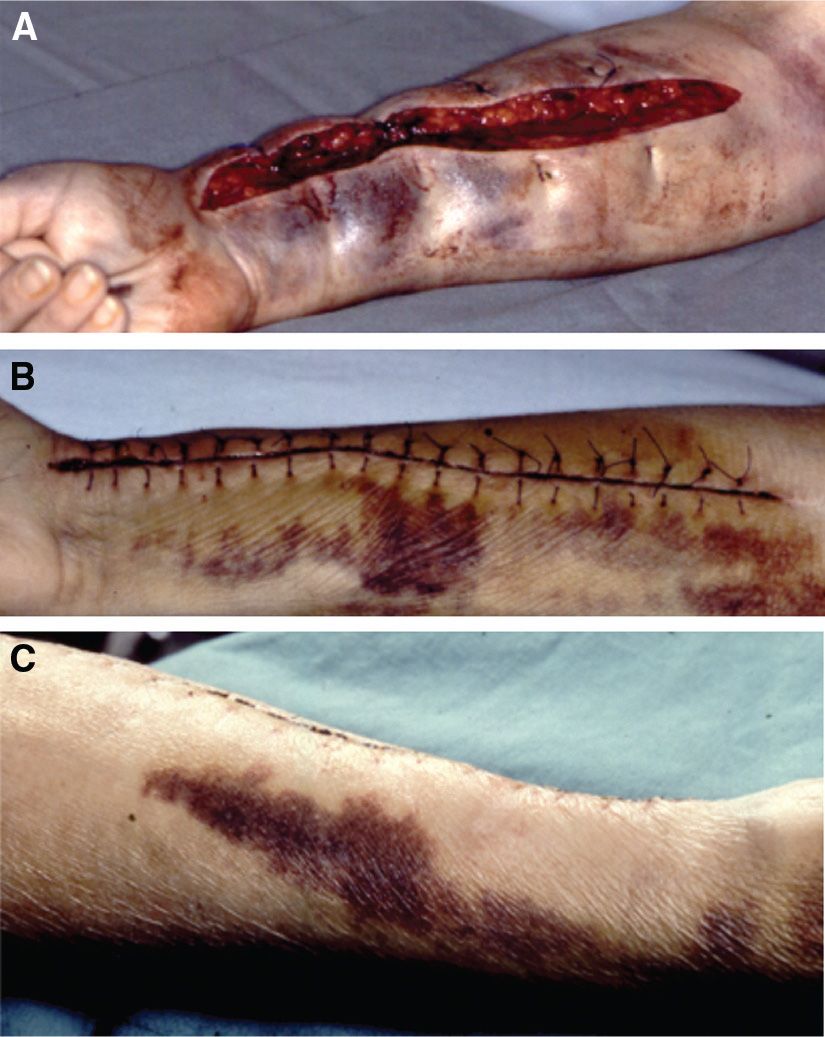
FIGURE 12-2 Compartment syndrome. A: Long surgical cut to relieve the pressure. B: The wound is closed during a second surgery. C: With prompt diagnosis and treatment, the outlook is excellent for recovery of the muscles and nerves inside the compartment. (Courtesy of G. Barbeau.)
Several large meta-analyses have found a relative reduction <75% of bleeding with TRA compared with the femoral approach.44–46 The benefit for TRA remains even if closure devices are used with femoral access.47,48 Access-site bleeding represents 60%–80% of bleeding episodes with the femoral approach, and the major benefit of TRA is the marked reduction of major bleeding related to access site (see Chapter 2). It should also be recognized that some blood loss has long been associated with femoral PCI. In the eighties, patients after percutaneous transluminal coronary angioplasty and heparin anticoagulation suffered hemoglobin (Hb) drops of 1–2 g/dL within 24 hours, with 6% of patients presenting with a fall in Hb of <3 g/dL.49,50 In contrast, in a recent study with transradial PCI and maximal antiplatelet therapy, the mean Hb fall was 0.6 ± 1.0 g/dL, with only 1.3% of patients presenting Hb drop < 3 g/dL within 24 hours.51
Most initial studies comparing bleeding with radial and femoral approaches did not use standardized bleeding classifications. Investigators in the EASY trial developed a hematoma classification adapted to TRA and this can be compared to recent hematoma scale proposed with femoral approach52,53 (Fig. 12-3). In this trial performed with maximal antiplatelet therapy, the incidence of hematoma <5 cm (grade I) was 5.3%, <10 cm (grade II) was 2.5%, distal to the elbow (grade III) was 1.6%, and proximal to elbow (grade IV) was 0.1%. Grade V is reserved for hematoma inducing compartment syndrome. It should be noted that while grade I and II hematomas are directly related to the puncture site, higher grades usually result from wire damages to vessels and small perforations. These may induce very unusual and rare hematomas such as hematoma of the pectoral muscle, of the neck, or even of the mediastinum.54 Ilhan et al.55 recently reported a first case of retropleural right hematoma which required transfusion and drainage with right radial diagnostic angiography complicated by difficult advancement of wire at the subclavian artery level. Following difficulty with wire advancement at the left subclavian artery, Parikh et al. described a patient who developed a large neck hematoma following post-PCI.56 A CT scan revealed diffuse hematoma infiltration with displacement of the trachea. Conservative management was performed without any sequelae. Following similar difficulty at the brachio-cephalic level, Arsanjani et al.57 reported bleeding following damage to a pericardio-phrenic artery, which required coil embolization to seal the perforation. Romagnoli et al.58 reported a transient cardiovocal syndrome in a patient where they had also faced difficulties with crossing the right subclavian artery but no clear hematoma was found with CT scan.
Complications resulting from vessel trauma such as pseudoaneurysm or arteriovenous fistula are rare (<0.1%), presumably due to the small caliber of these vessels. Pseudoaneurysms are easily diagnosed as they present with or without pain as a pulsating swelling. Most of the time there are signs of inflammation, which may let fear bacterial infection, but this is exceedingly rare.59,60 They are usually managed by repeat and prolonged compression after ultrasound confirmation, and extremely rarely require surgical interventions (ligation or patch).61 Several reports of successful thrombin injection have also been published62,63 (Fig. 12-4). Risks factors for pseudoaneurysm include female gender, hypertension, and chronic anticoagulation.
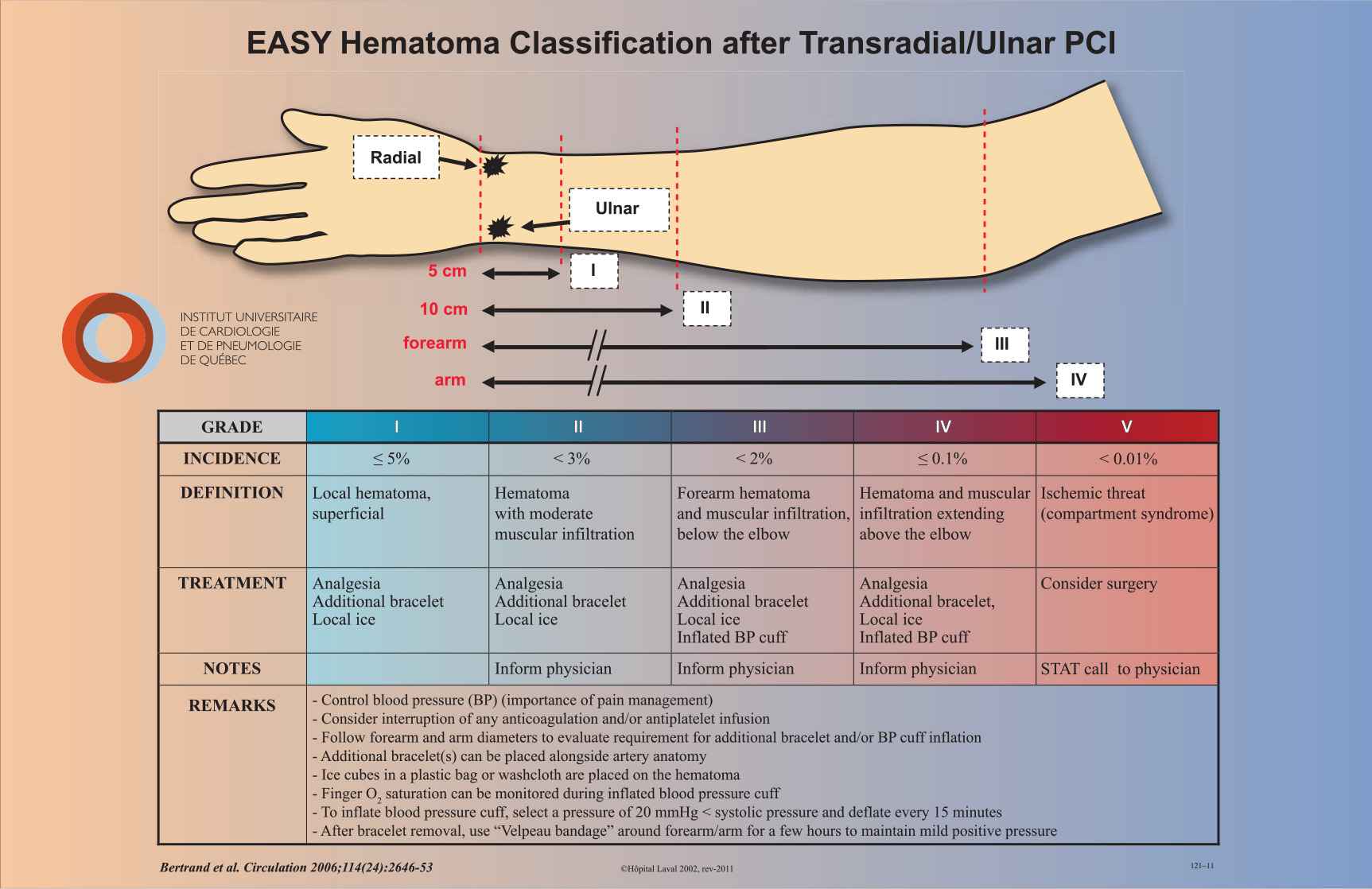
FIGURE 12-3 EASY hematoma classification after transradial/ulnar intervention. (From Bertrand OF. Acute forearm muscle swelling post transradial catheterization and compartment syndrome: prevention is better than treatment! Catheter Cardiovasc Interv. 2010; 75(3):366–368.)
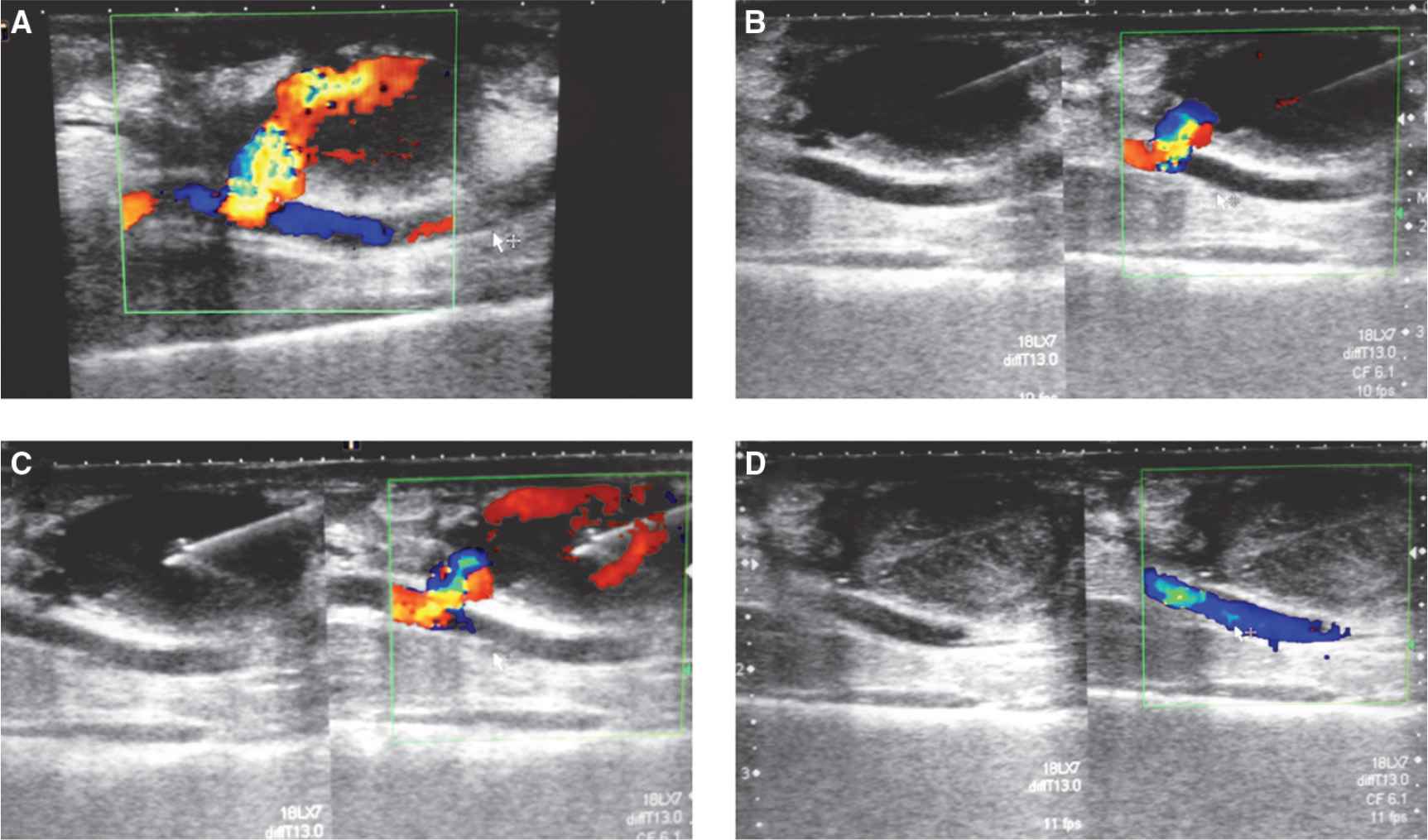
FIGURE 12-4 Ultrasound image of radial artery pseudoaneurysm. A: Color Doppler view showing pattern of turbulent blood flow between radial artery and pseudoaneurysm. B: Needle is positioned inside pseudoaneurysm. C: During thrombin injection. D: After thrombin injection, observe occlusion of pseudoaneurysm and closure of connection between radial artery and pseudoaneurysm.

FIGURE 12-5 Adverse local reaction to the use of hydrophilic sheaths (Cook) after radial artery cannulation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


