Chapter 13
Complications of Central Venous Access
The use of central venous catheterization is becoming more widespread. The indications for its use are expanding every day. It is estimated that more than three million central catheters are placed in this county each year. The annual cost is estimated at 230 million dollars. Chronic central venous catheters account for 15%, ports 29%, hemodialysis catheters 13%, and short-term catheters 26%.1 Therefore, the demands for insertion of central venous catheters are increasing every day.
Most central venous catheters are placed by interventional radiologists in the interventional radiology suite or by surgeons in the operating room. Despite advances in methods and techniques and improvements in equipment, it is inevitable that complications related to central venous catheter placement increase as more procedures are being performed. Central venous catheters are being placed by some operators who are not familiar with the techniques and methods of placing them. This situation sometimes occurs when expert personnel are not available or when a busy department has too many patients needing central venous access at the same time so that not enough experienced operators are available to insert the catheters.
Central venous catheters are placed for therapeutic and diagnostic indications, such as long-term systemic chemotherapy, administration of blood products, hemodialysis, plasmapheresis, total parenteral nutrition (TPN), stem cell harvesting, intravenous (IV) fluid administration, administration of IV medications, repeated blood samplings for laboratory tests, and to monitor response to treatment.2 The indications for placement of central catheters are expanding continuously. It is natural that, despite the use of careful techniques and adequate equipment, complications related to the procedure can eventually develop.
Advances in radiologic equipment and the routine use of fluoroscopy and ultrasound guidance during placement of central venous catheters in the vascular interventional radiology suite have allowed interventional radiologists to perform the procedures with fewer complications and lower costs.3,4 In a recent study of the costs of radiologic versus surgical placement of central venous catheters, the cost of the former was half that of the latter.5,6 In many aspects, the rate of complications of procedures done in the operating room, without fluoroscopy or ultrasound, is much higher.3,4,7 On the other hand, the rate of some delayed complications is similar, regardless of who inserts the catheters or where they are inserted. In addition, the rate of complications is directly related to the expertise of the operators placing those devices, regardless of their subspecialty.
Interventional radiologists frequently are called to solve problems originating from central catheter placement by operators with no experience in catheterization techniques; therefore, the vascular interventional radiologist must be ready to solve most of these problems.
It is important that personnel who place and care for catheters know and be familiar with the types of complications, the mechanisms of occurrence, and the prevention and management of complications. Emphasis on preventing complications is an ideal goal. Although prevention of complications should be the primary goal, it is impractical to think we can change the course of some events that are likely to occur in patients with long-term central venous catheters, who are thereby maintained and kept alive for a long time. The longer a central venous catheter is in place, the greater the risk that complications will develop.
We can therefore expect complications to occur sooner or later and must be prepared to manage these problems. Health workers responsible for central venous catheter maintenance must be familiar with the topic so they can notify the vascular interventional radiologists or surgeons in a timely manner because these persons eventually will take care of the problems. A combined approach with different operators would be ideal, particularly to maintain the functionality of hemodialysis catheters.8
As we shall see, it is much better to tackle a problem early, as soon as it is suspected, because it is easier to correct it, and the success of maintaining the access is higher. As a general principle, the central access should be maintained as long as possible, with every effort made to keep the catheters functioning. This is particularly important in patients who will have central catheters, perhaps for the remainder of their lives, such as patients on chronic hemodialysis. We must consider that many of these patients, particularly those on hemodialysis, have depleted most of their venous accesses, and their central venous catheters could be one of the last resources for hemodialysis. Therefore, we must make every effort to keep the access functional. We emphasize here that many catheters sooner or later will require revision.9
Sometimes it is better to be overconcerned about central venous catheter function. Health care personnel should not hesitate to contact the vascular interventional radiologist as soon as suspicion of catheter malfunctioning is raised, even if the problem seems “trivial.” The interventional radiologist must be ready and available at all times for consultation and should not question the call. We must realize that the degree of knowledge and expertise of the health workers are variable and sometimes limited.
On the other hand, health care personnel can take numerous steps to avoid or prevent complications and to improve the longevity of the catheters. Some such ideas are mentioned during the discussion of the different complications.10 We foster a “team approach” to central venous catheter maintenance that involves numerous individuals.8,11 The interventional radiologist must be involved in the care of the patients through the entire “life” of the catheter and port.1 Patients also must be educated and participate in the care of their access. Better patient education will result in lower rates of complications and improved patency. The rate of complications, however, remains low (3% in some series).12
TYPES OF COMPLICATIONS
For the sake of discussion, most authorities classify the complications in two large, broad categories.
Acute, Immediate, Early, and Procedural
These complications occur within 30 days of the procedure2 and include failure of placement, pneumothorax, hemothorax, hemopneumothorax, hemorrhage, misplacement of catheters, arterial injury, air embolism, thoracic duct injury, spasm of veins, injury to veins, injury to cardiac chambers, arrhythmias, injury to neural structures, inferior vena cava (IVC) filter dislodgement or extrusion, among others. Concerning peripherally inserted central catheters (PICCs), early complications are those occurring within less than 3 days after insertion.13 Some of these complications are rare, and others may be very unusual indeed and are listed here for completeness only. It is obvious that the better the technique and experience of the operators and the equipment used, the less likely it is that complications will occur.
Chronic, Delayed, Late, and Postprocedural
These complications occur later (after 30 days of the procedure) as a consequence of the long-term presence of the central venous catheter.2 The longer the catheter is in place, the more likely a complication will develop. With advances in catheter care, patients can be maintained with their accesses for many years and therefore are likely to develop complications. Concerning PICCs, late complications are those occurring more than 3 days after insertion.13
This group of complications includes infection, thrombosis, venous stenosis or occlusion, injury to vessels, migration of the catheter, fracture of the catheter, peripheral or central embolization of catheter fragments, malposition of catheter tip, erosion of skin and subcutaneous tissues, fibrous sheath deposition, hemorrhage, and others. In separate sections, we briefly describe most complications, the radiologic findings, and ways to prevent them, and we present some information about their management and treatment. Most of the information is derived from our own experience of many years with thousands of central venous catheterizations and also from a review of the works of other authors.
Acute Complications
Failure to Place a Central Catheter
Although not a true complication, here we include failure to place a central catheter as a complication. In our experience, inability to gain access is rare and almost nonexistent. Success rates of almost 100% are reported in the radiologic literature.2,14–16 Failures of placement of PICCs are almost nonexistent as well.13
We preferentially place central venous catheters in the internal jugular veins. If these veins are not available, the next access sites are the subclavian veins, the external jugular veins, and then the common femoral veins. If all these veins are occluded, the IVC by translumbar approach is the next step; finally, the hepatic veins by percutaneous puncture of the liver are used. Other less conventional accesses will be mentioned here as well. Most failures of catheter placement are by physicians and health workers with limited experience in catheterization techniques. The clinical literature reports failure rates of 4 to 33% during central venous catheter placement, except during bedside PICC placement, where high rates of success have been obtained.17–19
Vascular interventional radiologists have a very low or negligible failure rate because they access the veins with ultrasound or venographic “road mapping” guidance.20 With real-time ultrasound, the success rate of catheter placement approaches 100%, provided the central veins (internal jugular or subclavian) are patent. When the upper-body central veins are depleted, ultrasound and venography can be used to access the femoral veins, and when these veins are depleted, the IVC or the hepatic veins can be punctured with imaging guidance. Thereafter, other less common sites of access, such as azygous and hemiazygous, inter-costal, external jugular, or collateral veins can be used. Ultrasound and venography, in addition to facilitating puncture of the venous structures, prevent inadvertent puncture of adjacent arteries and other structures because the arteries usually course parallel to the veins.
Occasionally, computed tomography (CT) guidance can be used for IVC or hepatic vein access. We have placed catheters in the IVC under CT guidance. Thereafter, the patients were transported to the interventional radiology suite for final placement of the catheter. Many patients have completely depleted their veins for access. Sometimes, in some of these patients, the lumen of a chronically occluded vein can be recanalized, and a careful manipulation of wires and catheters may permit access into the superior vena cava (SVC) and right atrium (RA). The small lumen of the vein may not allow a large-bore catheter to be inserted into the RA, however. In some of these cases, fibrinolytic therapy with recombinant tissue plasminogen activator (tPA) alteplase (Activase), urokinase, or recombinant reteplase (Retavase) may be successful in recanalizing the vein and can be followed by angioplasty and stenting of the vein for central venous access. Angioplasty of venous stenoses to facilitate placement of central venous catheters must be encouraged and done as liberally as possible. There is no reason to struggle during catheterization of stenotic central veins, when the lesion can be dealt easily, quickly, and effectively with balloon dilatation and stenting, if needed.
In conclusion, vascular interventional radiologists know the central venous anatomy and have the materials and equipment needed for central venous catheterization. In experienced hands, the rates of failure of catheter placement are negligible: less than 1%. Vascular and interventional radiologists use creativity and intuition to place central venous catheters in patients with limited accesses, even after other less experienced operators may have failed. Furthermore, vascular interventional radiologists can perform various procedures, such as thrombolysis, percutaneous transluminal angioplasty (PTA), stenting, and stent-grafting of occluded or stenotic veins before placement of a central venous catheter, in situations when accesses are limited or almost completely depleted.20
Several options are available for catheter placement when conventional sites and placement are depleted. There are isolated reports of placement of catheters in unusual places, such as collateral veins, azygous system, external jugular veins, and others. Certainly, a close discussion between patients, referring physicians, and vascular interventional radiologists is necessary to determine the type of catheter and how long it will be needed. Sometimes, if a central catheter is needed for short-term therapy only, a peripheral IV insertion may be sufficient. So the message is that although central venous catheters are important and necessary, many times they are not needed if a simple IV access will do the job.
Inadvertent Removal of the Catheter
A problem that occurs occasionally is the inadvertent or accidental removal of a catheter. Sometimes the catheter falls out by itself, but this usually occurs because the patient removes the catheter for some reason; some uncooperative patients may do this. Although not a complication per se, it is mentioned here because it requires placement of a new catheter. Sometimes clinicians remove catheters, without consulting the interventional radiologist, when they think the catheter might be malfunctioning but in reality it is functioning well. Of course, this practice must be discouraged.9,21
Pneumothorax
Pneumothorax is now a rare complication of venous access caused by transgression of the pleural space, usually during the venous puncture.22 In a recent report, the incidence was 0.1% (one case in 880 procedures).14 In the past, this complication was more frequent because the subclavian veins were preferentially used for initial access. The subclavian veins are the preferred initial access for clinicians and other operators. Vascular interventional radiologists prefer the internal jugular veins for access, and therefore the rate of pneumothorax is low, reported to be between 0 and 1.7%.1,21 We try to spare or avoid the subclavian veins for central access, particularly in patients undergoing hemodialysis, for reasons that are described later.
Furthermore, even in the event that the subclavian veins are used for access, the puncture of the subclavian veins is done under digital venography “road mapping” or ultrasound guidance, and therefore the rate of pneumothorax has significantly decreased to almost nonexistent. Puncture of the subclavian veins should be performed under direct vision of the vein. We prefer to puncture the subclavian veins lateral to the intersection of the first rib and the clavicle to avoid pneumothorax and the “pinch-off” syndrome and catheter fracture and embolization (described in foregoing paragraphs). The likelihood of pneumothorax during an internal jugular puncture is almost nil or nonexistent.
The reported rate of pneumothorax during subclavian vein puncture approaches 1 to 6%, depending on the techniques used.17,23 The higher rate is likely during “blind” punctures by operators unfamiliar with the technique. In our experience, the rate of pneumothorax is less than 0.1%. It has been reported that pneumothorax may account for 30% of complications during “blind” punctures.17
On occasion, air is aspirated during venipuncture. If the patient complains of some tracheal irritation and cough during the puncture, it is likely that the trachea has been punctured. In this case, the contaminated needle should be discarded before a new puncture of the vein is attempted.
The diagnosis of pneumothorax can be made with fluoroscopy but more appropriately with “conventional” upright chest radiographs in frontal and lateral views on inspiration and expiration. CT has been used to depict small pneumothoraces not visualized with conventional radiographs. If a small pneumothorax is suspected, it is clinically not significant and follow-up chest radiographs are adequate (Fig. 13–1).
Treatment Management of a pneumothorax varies, depending on the specific circumstances and particularly on the degree of lung collapse. If there is a small pneumothorax (less than 15%) and the patient is asymptomatic, treatment is conservative and includes observation and serial chest radiographs. A repeat chest radiograph may be obtained in 6 to 8 hours before discharge.
If the pneumothorax is asymptomatic, but the amount is more than 15%, a chest catheter or tube needs to be placed. The chest tube can be inserted in the interventional radiology suite by interventional radiologists. A catheter with a Heimlich valve is used for small pneumothoraces. If the pneumothorax is large, the patient will need to have a chest tube placed by the surgeon or by the interventional radiologist (if he or she is knowledgeable about the technique). We prefer that a surgeon place the tube and manage the complications.
Hemothorax
Bleeding into the thoracic cavity is a serious complication and usually is a result of injury to a vessel (vein or artery) during puncture and transgression of the thoracic cavity. Another rare cause of hemothorax is injury to vessels during catheter removal in the unexpected situation in which the tip of the catheter is adherent to the vessel wall, causing a tear of the vessel wall during withdrawal.
The degree of bleeding varies. Minor bleeding usually causes no significant sequela; however, serious bleeding requires immediate treatment. Serious hemothorax is usually due to puncture and laceration of a large artery, such as the subclavian, internal mammary, or carotid, which are in close apposition to the veins being punctured. Tears to the central veins also can result in serious hemothoraces. Fortunately, this complication is rare, especially when the access is done under ultrasound or fluoroscopic venographic guidance. The subclavian venous approach may be more likely to result in major vessel injury. During subclavian vein punctures, lateral to the junction of the first rib with the clavicle, the risk of pneumothorax and hemothorax is very low.
Isolated reports of injuries to the aorta, brachiocephalic arteries, and even the pulmonary arteries during central venous catheter placement have resulted in serious hemothoraces requiring emergency intervention. Injuries to the arteries resulting in hemothorax are not uncommon when inexperienced house officers try to place central venous catheters in the emergency room or bedside without ultrasound or fluoroscopic guidance.
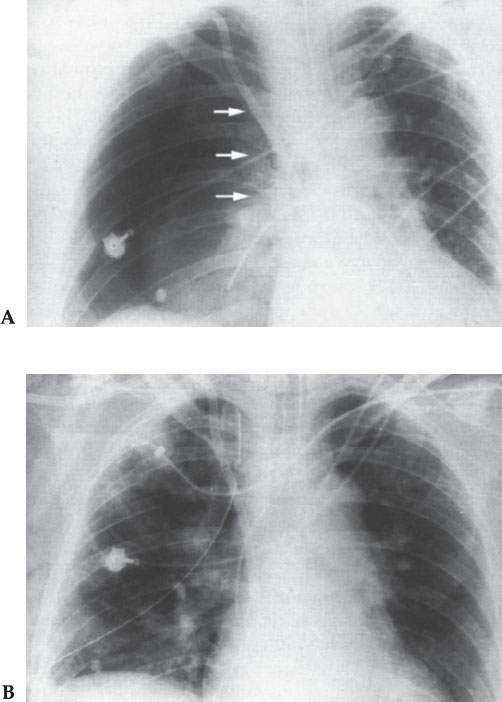
Figure 13–1 (A) Large pneumothorax (arrows) after central catheter placement by internal jugular vein puncture. (B) A chest tube was placed. The patient recovered uneventfully.
Prevention It is most important that the veins be punctured under ultrasound or fluoroscopic guidance. Also, personnel unfamiliar with imaging guidance should not try “blind” approaches in seriously ill, uncooperative, intoxicated patients, particularly in the emergency department.
Treatment Consists of maintaining the patient’s hemodynamic stability and insertion of a chest tube for drainage of the blood and, perhaps, repair of the injured vessel, if possible. With the advent of stent grafts, this complication can be managed in the interventional radiology suite. If an arteriovenous fistula (AVF) is present, transcatheter embolization is preferable to surgery. Fortunately, this event is rare.
Air Embolism
Air embolism is a serious and potentially fatal complication, but it is fortunately rare. An incidence of 1.4% was reported in a recent article.14 A mortality rate of 50% is associated with this complication. Air can be introduced (sucked in) into the veins through needles, catheters, sheaths, and peel-away sheaths during the procedure.22 Obviously, air can enter the veins during the many different steps of central venous catheter placement. The negative intrathoracic pressure, particularly during inspiration, will allow air to be sucked into the veins if there is an opening (communication) between the atmosphere and the bloodstream during insertion (or removal) of needles or catheters in the RA or central veins.1,17,24
It has been estimated that a large amount of air can enter the bloodstream rapidly via needles or catheters used for central venous access. One or two deep breaths may be enough to introduce sufficient air to result in a fatal embolism. Some uncooperative patients may cough, take deep inspirations, or perform a Mueller maneuver during catheter insertion, thereby decreasing the intrathoracic pressure, facilitating aspiration of air into the venous system. Some patients are deeply sedated during the procedure and may not be able to cooperate. It is important to cover open needles and catheters and to be as expeditious as possible during the steps of catheter insertion, including during wire insertion into the needle after the vein has been punctured or dilatation of the tract for catheter or peel-away sheath insertion.
One of the most dangerous steps for air embolism is during removal of the dilator from the peel-away sheath and insertion of a large-diameter [12–14 French (F)] tunneled catheter. It is important to ask the patients to take a deep breath, stop breathing, perform the Valsalva maneuver (if possible), or hum during final insertion of the catheter into the peel-away sheath.
These maneuvers are intended to increase the intrathoracic pressure, with resultant increasing bleeding from the sheath but decreasing the risk of air embolism. If the patient is under general anesthesia, we suspend the respiration, if possible. Pinching the peel-away sheath immediately after removal of the dilator is also recommended if the catheter cannot be inserted immediately into the peel-away sheath to obliterate the large lumen that is a direct communication between the atmosphere and the central venous system or RA. Obviously, if the peel-away sheath is crushed or pinched, it must be restored to normal shape quickly; otherwise, it may be difficult to insert the soft Silastic catheters through the sheath.
One important concept is the possibility of air embolism during removal of catheters. In many institutions, removal of catheters is delegated to nursing or ancillary personnel. If they are not aware of this potential problem or if they are not careful enough, a catastrophic air embolism could result. This is mentioned in another section.
Pressure changes in the intrathoracic cavity are responsible for air embolism during catheter insertion or removal. During inspiration, the intrathoracic pressure drops below atmospheric pressure. During expiration, the reverse is true. There are also changes in pressures in the central veins. The pressure decreases during inspiration and increases during expiration. During inspiration, therefore, air can easily be sucked into the veins in the same manner as air enters the lungs.24
Moreover, because a fibrin sheath usually develops around indwelling catheters, a fibrin tract may be formed from the skin entry site to the central vein. Therefore, as soon as a catheter is withdrawn, air could easily enter into the venous system if one is not careful to obliterate the entry site, tunnel, pathway, or tract into the vein. Air into the right heart gets trapped in the pulmonary outflow tract and right-sided heart failure, shock, and death may ensue.24
Prevention Increasing intrathoracic pressure during removal of the catheter to prevent air from entering the venous system can be done by stopping respiration, taking a deep breath, and bearing down (Valsalva) or humming. Placing the patient in Trendelenburg position during catheter insertion is also effective but not practical in most angiographic suites.1
Treatment
1. Observe the patient carefully. Monitor vital signs closely.
2. Give oxygen 100% by mask. A loud churning sound may be auscultated over the chest in the presence of serious air embolism.
3. Place the patient in the left lateral Trendelenburg position to trap air in the RA.
4. Aspirate air from the RA via the catheter just placed, or place another catheter in the RA to aspirate air. Some investigators advocate percutaneous puncture of the RA with a needle and aspiration of trapped air.17,24
Thoracic Duct Injury
This is a rare complication that may occur when the left internal jugular or left subclavian vein approach is used. The thoracic duct ascends in the left hemothorax and curves anteriorly to drain into the left subclavian vein. The thoracic duct may be enlarged in cirrhotic patients, making this complication more likely. Care must be taken during left subclavian vein puncture in cirrhotic persons and in patients with chronic lymphatic obstruction because enlargement of the thoracic duct may be present. This injury is suspected when the patient develops a left chylothorax after access.
Prevention A lateral puncture during left subclavian vein access lateral to the junction of the left clavicle and the left first rib should prevent thoracic duct injury. Imaging guidance should decrease the number of unsuccessful punctures and decrease the risk of this complication as well.
Treatment Treatment is to remove the catheter, apply pressure, and observe the patient. No other sequela is expected. Surgery is rarely indicated.
Catheter Misplacement
The ideal location for central venous catheters is at the junction of the SVC and RA.25 We prefer to place the catheter a little more into the RA, where the blood pool is more abundant, particularly for hemodialysis and pheresis catheters. The same can be said for PICCs and portacaths.
The incidence of catheter misplacement by vascular interventional radiologists is very low (less than 1%) because most, if not all, catheters are placed under ultrasound or venographic guidance for access and fluoroscopy for definitive placement of the tip of the catheter. We usually leave the catheter in its final location after a “survey” is taken by the vascular interventional radiology team, including technologists, nurses, and others. We look at the monitor and agree on the final position of the catheter. If any discrepancy or question exists concerning location of the tip of the catheter, an injection of contrast material is made and digital subtraction angiography (DSA) or “one-shot” pictures are taken. If the catheter is in an anomalous position, we immediately investigate and try to determine why the catheter is lodged there. On occasion, anomalies of the venous system, such as double SVC, left SVC, absence of jugular veins, and so on may be the cause.
We do not terminate the procedure until we are sure that the catheter is in the correct position and is working properly. Blood must be aspirated easily from all ports of all catheters. By rotating the C-arm in different obliquities, we make sure that a catheter taking an unusual course is not lodged in an unusual or anomalous vein (such as azygos, small veins, contralateral central veins). If any question exists, contrast material must be injected to ascertain the position of the tip of the catheter.
When dealing with obese patients, particularly women with large breasts, we tape the breasts down caudally, toward the lower chest and waist, and then make sure that a longer catheter (about 5 cm longer) is used.25 This is because of the migration of the catheters when the patients sit or stand and walk.26,27 Sometimes we obtain chest radiographs in the supine and upright positions to evaluate changes in catheter tip position; however, some do not obtain chest radiographs.28 If the catheter is too short in the SVC in the supine position, when the patient is supine or when the patient stands, the catheter can migrate cephalad and abut the vessel wall (either the SVC or central veins) and become nonfunctional. On occasion, we ask the patients to sit up and we check the position of the tip of the catheter with fluoroscopy for changes in position from supine to erect and correct any misplacement before the patient leaves the room.25
If the catheter is too low or too long into the RA, it may impair the functioning of the cardiac valves with resultant arrhythmias. On occasion, if the catheter is too long, it may prolapse across the tricuspid valve into the right ventricle with resultant arrhythmias as well. Furthermore, complications from a long or misplaced catheter are not uncommon. Endocardial damage, vegetations, thrombosis, damage to valves, inflammation, infection, endocarditis, and other problems have been described related to the abnormal position of the misplaced catheters.
Inadvertent malposition of catheters in an artery is possible but very unlikely when using ultrasound or fluoroscopic guidance. Furthermore, if one punctures an artery rather than a vein, a pulsatile flow of bright red blood will be obvious and unmistakable. Less-experienced operators doing “blind” punctures may experience this complication. In addition, because the arteries and veins are in close apposition to each other, and because large-bore catheters may need to be inserted, there is a possibility of creating an AVF. This could happen during puncture of the internal jugular vein (with the carotid arteries) or subclavian veins (with the subclavian arteries) and common femoral veins (with the common femoral arteries), among others. Arterial occlusion, thrombosis, embolism, pseudo-aneurysm, and arteriovenous fistula are rare but possible complications of placement of central catheters.
One common malposition during “blind” insertion of a subclavian catheter is when the tip of the catheter becomes lodged in the ipsilateral internal jugular vein as the catheter goes cephalad rather than caudad into the SVC. In addition, the catheter could be placed across the midline into the contralateral subclavian vein, internal jugular vein, azygous, hemiazygous, or accessory hemiazygous veins. Sometimes the catheters are lodged in small peripheral veins and small thoracic veins. In these cases, the catheters eventually will malfunction because of venous thrombosis causing persistent inability to withdraw blood. Malpositioned catheters frequently become malfunctional or nonfunctional, and thrombotic complications may ensue. Misplacement of catheters is one of the most common etiologic factors of catheter or venous thrombosis (Figs. 13–2 and 13–3).
Rare reports of perforation of the pleura and insertion of the catheter into the pleural cavity have been published. Extravascular insertion in other sites may occur, such as in the neck, mediastinum, chest, and so on.
Treatment The malpositioned catheter must be repositioned using a variety of maneuvers and techniques. If the problem is found immediately during or after placement and the patient is still on the angiographic table, the catheter can be repositioned by advancing one or two guide-wires (preferable hydrophilic) through one or both lumens of the catheter and trying to reposition the tip.
When a catheter is found malpositioned sometime after placement, it may be repositioned via a common femoral vein approach using the gooseneck loop snare technique. This procedure is rather simple and is described in another section. Briefly, a sheath is inserted into a common femoral vein. An Amplatz gooseneck loop snare or a Dotter basket is advanced into the RA or SVC. The catheter tip is snared with the loop or snare, the loop or snare is closed, and the catheter repositioned. This technique works if the tip of the catheter is free and not attached to the vessel wall. Otherwise, one can use a tip-deflecting wire to release the tip of the catheter from the wall of the vessel and once one end of the catheter is free, a gooseneck loop snare, a basket, or a Curry loop can be used to snare the catheter and reposition in the correct location. This procedure is simple and efficacious, it can be done in a few minutes, and it is used when other techniques fail, especially when dealing with a malpositioned portacath. Finally, if a catheter cannot be repositioned, it must be exchanged for a new one using conventional catheter exchange methods.
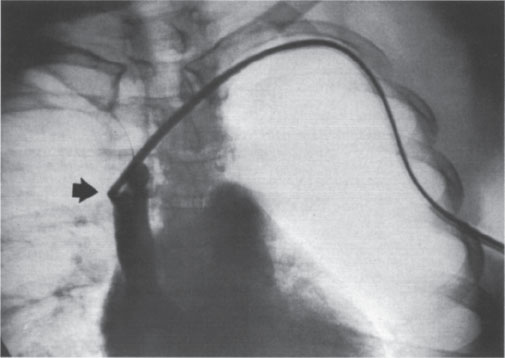
Figure 13–2 Malpositioned left subclavian catheter. The tip is in the superior vena cava (arrow). Fibrin deposits are noted.
Vascular Injuries
Arteries and veins (and lymphatics) can be injured during central venous catheter placement. Clinically significant arterial puncture occurred in 12 of 880 procedures (1.4%) in a recent study.14 Fortunately, these mishaps are uncommon. Some of these problems are described with the different complications, either acute (procedural) or chronic (postprocedural). Possible problems include the following:
• Injury to the carotid artery during internal jugular vein puncture. One carotid puncture occurred in 82 placements in a recent series.29 Pseudo-aneurysms resulting from inadvertent catheterization of the carotid artery with large-diameter catheters have been described. AVFs are possible but rare occurrences.
• Injury to the subclavian artery and branches may occur during subclavian vein access. The close apposition between the artery and the vein makes the artery vulnerable to injury during attempts at venous puncture (Fig. 13–4).
• Injuries to the abdominal aorta and branches are very unlikely but could occur during IVC catheter placement by a translumbar approach.
• Injuries to the femoral arteries are more common during arteriographic studies but also sometimes occur during venous catheterization.
• Trauma to the upper-extremity arteries (brachial artery) is rare but possible during PICC line placement.13
• Arteriovenous fistulas are rare complications but can be a major problem for management. Fortunately, these lesions are so rare that we have no experience in this specific problem. If a large AVF occurs during central venous catheterization, embolization or placement of stent grafts should solve the problem.
• The thoracic aorta and brachiocephalic arteries and branches may be injured during internal jugular vein or subclavian venous puncture if a low puncture is made or a needle that is too long is used. We therefore favor the use of “short” (4–5 cm long), small-gauge (22-gauge) needles and micropuncture sets for venous puncture. In cases of inadvertent arterial puncture, the needle is withdrawn and manual pressure is applied for a few minutes for hemostasis, which usually is sufficient.14



