Various physical, emotional, and extrinsic triggers have been attributed to acute coronary syndrome. Whether a correlation can be drawn between identifiable ischemic triggers and the nature of coronary artery disease (CAD) still remains unclear. In the present study, we evaluated the correlation between triggered versus nontriggered ischemic symptoms and the extent of CAD in patients with ST-segment elevation myocardial infarction (STEMI). We conducted a retrospective, single-center observational study including 1,345 consecutive patients with STEMI, treated with primary percutaneous coronary intervention. Acute physical and emotional triggers were identified in patients’ historical data. Independent predictors of multivessel CAD were determined using a logistic regression model. A potential trigger was identified in 37% of patients. Physical exertion was found to be the most dominant trigger (65%) followed by psychological stress (16%) and acute illness (12%). Patients with nontriggered STEMI tended to be older and more likely to have co-morbidities. Patients with nontriggered STEMI showed a higher rate of multivessel CAD (73% vs 30%, p <0.001). In a multivariate regression model, nontriggered symptoms emerged as an independent predictor of multivessel CAD (odds ratio 8.33, 95% CI 5.74 to 12.5, p = 0.001). No specific trigger was found to predict independently the extent of CAD. In conclusion, symptoms onset without a recognizable trigger is associated with multivessel CAD in STEMI. Further studies will be required to elucidate the putative mechanisms underlying ischemic triggering.
Different behavioral, physical, and psychological factors have been shown to precipitate acute coronary syndromes (ACSs). Physical activity, emotional stress, and sexual intercourse are all sympathetic activators known to trigger myocardial infarction (MI) by sudden increase in heart rate, blood pressure, myocardial contractility, and oxygen demand. Increased autonomic vagal drive, as may occur after heavy meals or acute alcohol consumption, has also been related to acute MI by different mechanisms, including hemodynamic changes and coronary vasoconstriction. A recognizable trigger has been demonstrated in almost half of patients with acute MI, generally occurring during a hazard period of 1 to 2 hours before symptoms onset. Yet, the relation of such triggers before ischemic clinical symptoms to the nature and extent of the coronary artery disease (CAD) in these patients remains unclear. In fact, the investigation of the immediate circumstances under which MI occurs, also known as “acute risk factors” or “acute triggers”, have received relatively limited attention so far, compared with classical, chronic risk factors. In the present study, we assessed the possible correlation between the presence of an identifiable trigger before ischemic symptoms, based on the clinical history obtained during hospitalization, and the extent of coronary disease by angiography, in a large cohort of patients with ST-segment elevation MI (STEMI) undergoing primary percutaneous coronary intervention (PCI).
Methods
A retrospective, single-center observational study was performed at the Tel-Aviv Sourasky Medical Center, a tertiary referral hospital with a 24 of 7 primary PCI service. Included were all 1,436 consecutive patients admitted from January 2008 to December 2013 to the Cardiac Intensive Care Unit with the diagnosis of acute STEMI and treated with primary PCI. Excluded were patients treated either conservatively or by thrombolysis (n = 26), as were 65 patients whose final diagnosis on discharge was other than STEMI (e.g., myocarditis or takotsubo cardiomyopathy). The final study population included 1,345 patients whose baseline demographics, cardiovascular history, clinical risk factors, treatment characteristics, and laboratory results were all retrieved from the hospital electronic medical records. Diagnosis of STEMI was established in accordance to published guidelines including a typical chest pain history, diagnostic electrocardiographic changes, and serial elevation of cardiac biomarkers. Significant CAD was defined as 50% or greater coronary lumen stenosis. The study protocol was approved by the local institutional ethics committee. Acute triggers known by their potential to provoke myocardial ischemia were retrospectively identified in patients’ historical data gathered during hospitalization from patients and accompaniers when interviewed by the admitting physician. Recognized triggers included: physical exertion at an effort level equivalent to Borg ≥13 (defined by the patient as “somewhat hard” or harder), emotional stress (defined by patient), sexual intercourse, acute illness (i.e., fever/sepsis, invasive procedures), large meal (larger than usual), and alcohol/drugs (i.e., marijuana, cocaine, heroin)/coffee consumption. We assumed a causative correlation between potential triggers and symptoms, if the 2 appears within 2 hours.
All data were summarized and displayed as mean ± SD for continuous variables and as number (percentage) of patients in each group for categorical variables. The p values for the categorical variables were calculated with the chi-square test. Continuous variables were compared using the independent sample t test. Independent predictors of multivessel CAD (defined as >1 vessel CAD) were determined using a logistic regression model adjusted for age, gender, hypertension, diabetes mellitus, symptom duration, C-reactive protein (CRP) level and to the onset of symptoms while at rest. A 2-tailed p value of <0.05 was considered significant for all analyses. All analyses were performed with the SPSS software (SPSS Inc., Chicago, Illinois).
Results
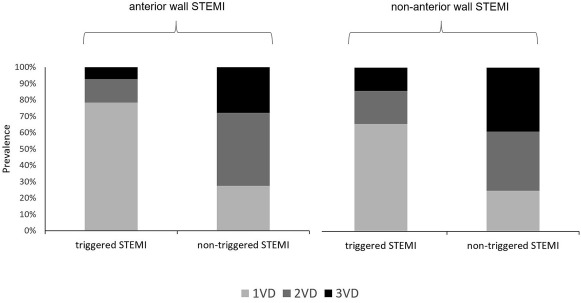
A total of 1,345 patients with STEMI (mean age 61 ± 13 years old, 81% men) treated by primary PCI were enrolled in the study. A potential trigger was identified in 497 patients (37%). Physical exertion was found to be the most dominant trigger (65%) followed by psychological stress (16%) and acute illness (12%; Figure 1 ). Baseline clinical characteristics of patients according the presence/absence of an ischemic trigger before symptoms are listed in Table 1 . Compared to patients with an identifiable ischemic trigger before symptoms onset, patients without a clear trigger on a medical history were more likely to be older, diabetic, and hypertensive. Patients developing symptoms without a clear trigger were more likely to have multivessel CAD vessel disease (73% vs 30%, p <0.001; Figure 2 ). Similar results were found while focusing separately on anterior and nonanterior well patients with STEMI ( Figure 3 ). Using a multivariate regression model designed to elucidate the risk factors predicting multivessel CAD nontriggered symptoms emerged as an independent predictor of multivessel CAD (odds ratio 8.33, 95% CI 5.74 to 12.5, p = 0.001). Additional risk factors included older age, female gender, and diabetes mellitus ( Table 2 ). No specific trigger was found to predict independently multivessel CAD.

| Variable | Onset of Symptoms | p Value | |
|---|---|---|---|
| Non-Triggered (n=847) | Triggered (n=498) | ||
| Age (years) | 63 ± 13 | 59 ± 13 | <0.001 |
| Men | 670 (79%) | 409 (82%) | 0.202 |
| Diabetes mellitus | 198 (23%) | 86(17%) | 0.009 |
| Dyslipidemia | 395 (47%) | 241 (48%) | 0.535 |
| Hypertension | 399(47%) | 184(36%) | <0.001 |
| Smoking history | 438 (51%) | 237 (48%) | 0.158 |
| Family history of coronary artery disease | 135(16%) | 83 (17%) | 0.759 |
| Prior myocardial infarction | 89 (10%) | 44 (9%) | 0.345 |
| Time to first medical contact (minutes) | 354 ±442 | 337 ± 465 | 0.003 |
| Admission C- reactive protein (mg/L) | 14 ± 28 | 11± 27 | 0.001 |
| Admission glucose (mg/dL) | 161.5 ± 72 | 147.6 ± 60 | 0.0003 |
| Admission serum creatinine (mg/dl) | 1.17 ± 0.27 | 1.14 ± 0.25 | 0.01 |
| Left ventricular ejection fraction (%) | 47 ± 8 | 48 ± 8 | 0.453 |
| Peak creatine phosphkinase (Units/L) | 1152± 1263 | 1230± 1499 | 0.667 |

| Correlates | OR | 95 CI | p Value |
|---|---|---|---|
| Age | 1.02 | 1.05-1.04 | 0.01 |
| Gender | 0.42 | 0.26-0.69 | 0.001 |
| Diabetes mellitus | 1.70 | 1.08-2.69 | 0.02 |
| Hypertension | 1.16 | 0.78-1.72 | 0.46 |
| Non-triggered symptoms | 8.33 | 5.74-12.5 | 0.001 |
Results
A total of 1,345 patients with STEMI (mean age 61 ± 13 years old, 81% men) treated by primary PCI were enrolled in the study. A potential trigger was identified in 497 patients (37%). Physical exertion was found to be the most dominant trigger (65%) followed by psychological stress (16%) and acute illness (12%; Figure 1 ). Baseline clinical characteristics of patients according the presence/absence of an ischemic trigger before symptoms are listed in Table 1 . Compared to patients with an identifiable ischemic trigger before symptoms onset, patients without a clear trigger on a medical history were more likely to be older, diabetic, and hypertensive. Patients developing symptoms without a clear trigger were more likely to have multivessel CAD vessel disease (73% vs 30%, p <0.001; Figure 2 ). Similar results were found while focusing separately on anterior and nonanterior well patients with STEMI ( Figure 3 ). Using a multivariate regression model designed to elucidate the risk factors predicting multivessel CAD nontriggered symptoms emerged as an independent predictor of multivessel CAD (odds ratio 8.33, 95% CI 5.74 to 12.5, p = 0.001). Additional risk factors included older age, female gender, and diabetes mellitus ( Table 2 ). No specific trigger was found to predict independently multivessel CAD.




