Patients with severe mental illness (SMI), including schizophrenia and bipolar disorder, are at elevated risk of ST-elevation myocardial infarction (STEMI) but have previously been reported as less likely to receive revascularization. To study the persistence of these findings over time, we examined trends in STEMI incidence, revascularization, and in-hospital mortality for patients with and without SMI in the National Inpatient Sample from 2003 to 2012. We further used multivariate logistic regression analysis to assess the odds of revascularization and in-hospital mortality. SMI was present in 29,503 of 3,058,697 (1%) of the STEMI population. Patients with SMI were younger (median age 58 vs 67 years), more likely to be women (44% vs 38%), and more likely to have several co-morbidities, including diabetes, chronic pulmonary disease, substance abuse, and obesity (p <0.001 for all). Over time, STEMI incidence significantly decreased in non-SMI (p for trend <0.001) but not in SMI (p for trend 0.14). Revascularization increased in all subgroups (p for trend <0.001) but remained less common in SMI. In-hospital mortality decreased in non-SMI (p for trend = 0.004) but not in SMI (p for trend 0.10). After adjustment, patients with SMI were less likely to undergo revascularization (odds ratio 0.59, 95% CI 0.52 to 0.61, p <0.001), but SMI was not associated with increased in-hospital mortality (odds ratio 0.97, 95% CI 0.93 to 1.01, p = 0.16). In conclusion, in contrast to the overall population, the incidence of STEMI is not decreasing in patients with SMI. Despite changes in the care of STEMI, patients with SMI remain less likely to receive revascularization therapies.
Cardiovascular disease and acute myocardial infarction (AMI) are highly prevalent in patients with severe mental illness (SMI). Previous research has shown that patients with SMI with AMI are less likely than patients without SMI to undergo cardiac catheterization and revascularization procedures. Although the effect of this particular treatment disparity on mortality is not consistently established, patients with schizophrenia particularly appear to be at elevated risk. Importantly, because this disparity was first observed, there have been broad changes in the medical treatment of AMI, especially ST-elevation MI (STEMI). These include the increased use of early angiography and primary percutaneous coronary intervention (PCI) and the decreasing use of thrombolytic therapy. Such treatment changes have been accelerated by national initiatives encouraging timely revascularization, which in turn have contributed to a reduction in short-term mortality. It remains unknown, however, whether these shifts have affected the disparate rate of revascularization in patients with SMI, and whether such patients have had an equivalent decrease in mortality. To address these questions, we performed an analysis of patients with STEMI over a 10-year period in a nationally representative US database.
Methods
Data were obtained from the Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project—National (Nationwide) Inpatient Sample (NIS) files from 2003 to 2012. From 2003 to 2011, the NIS represented a 20% stratified sample of all community nonfederal US hospitals. Starting in 2012, the NIS was redesigned to represent 20% of all discharges from nonfederal US hospitals, representing 94% of all discharges from US community hospitals. Discharges are weighted based on the sampling scheme to permit inferences for a nationally representative population. In the year 2012, the NIS contained deidentified information for 7,296,968 discharges from 4,378 hospitals in 46 states, representing 36,484,846 discharges. Each record in the NIS includes all procedure and diagnosis codes recorded for each patient’s hospital discharge.
From January 2003 to December 2012, hospitalizations for AMI were selected by searching for the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for initial AMI 410.x1 (n = 1,986,035 representing 9,754,267 patients). Patients with ICD9 codes 410.7x (subendocardial MI) were excluded from analysis. Patients with a concomitant diagnosis of cardiogenic shock were identified using ICD-9-CM code 785.51. We used ICD-9-CM procedure codes to identify patients who underwent PCI (00.66, 36.01, 36.02, 36.05, 36.06, and 36.07) or coronary artery bypass grafting (CABG; 36.1x).
Patient- and hospital-level variables were included as baseline characteristics. Co-morbidities were identified using standard Agency for Healthcare Research and Quality variables (based on Elixhauser methods). Co-morbid SMI was considered present based on secondary ICD-9-CM codes using a previously reported categorization as follows: (1) schizophrenia (295) and (2) bipolar disorder (296.00 to 296.06, 296.40 to 296.89). SMI was defined as present if a patient had codes indicating either schizophrenia, bipolar disorder, or both.
For descriptive analyses, we compared baseline characteristics and hospital characteristics between patients with SMI and without SMI. Continuous variables are presented as means or medians as appropriate; categorical variables are expressed as frequencies (percentages). To compare baseline characteristics and in-hospital care patterns with respect to SMI, either Mann–Whitney Wilcoxon nonparametric tests or the Student t test was used for continuous variables, and Pearson chi-square tests were used for categorical variables. We calculated STEMI incidence as the weighted number of STEMI divided by 20% of the US population during that time period. Estimates of the US adult population were obtained from the US Census Bureau. All trends for patients with and without SMI were evaluated using the autoregressive integrated moving average model for time series.
Unadjusted in-hospital outcome rates were calculated according to SMI status. Multivariate logistic regression analyses were used to assess the associations between SMI (and its individual components) and outcomes including likelihood of undergoing revascularization and in-hospital mortality. For all regression analyses, the Taylor linearization method “with replacement” design was used to compute variances. Covariates included demographics, hospital characteristics, pertinent Elixhauser co-morbidities (anemia, connective tissue disease, congestive heart failure [CHF], chronic pulmonary disease, coagulopathy, depression, diabetes, hypertension, liver disease, electrolyte abnormalities, metastatic cancer, neurologic disorders, obesity, pulmonary vascular diseases, pulmonary circulation disorders, renal failure, substance abuse, weight loss, and valvular disease), previous PCI and/or CABG, hemodialysis, and cardiogenic shock. The covariant retention threshold was set at a p value of <0.10. In addition, for the analysis of in-hospital mortality, we separately tested the model in samples stratified by revascularization.
All statistical tests were 2-sided, and a p value of <0.05 was set a priori to be statistically significant. All the analyses were conducted using SAS, version 9.2 (SAS Institute, Cary, North Carolina) and SPSS, version 22 (IBM Corporation, Armonk, New York).
Results
There were 9,754,267 patients with AMI, of which, 3,058,697 patients had STEMI and were included for analysis. Among the STEMI cohort, 29,503 patients (1%) had SMI. Of the patients with SMI, 12,590 patients (42.7%) had schizophrenia, 15,679 patients (53.1%) had bipolar disorder, and 1,234 (4.2%) had both disorders.
Patients with SMI were significantly younger than patients without SMI and had a younger age distribution ( Table 1 ). Notably, patients with SMI were more likely to be women, nonwhite, have a history of substance abuse, diabetes, depression, neurologic disorders, CHF, chronic pulmonary disease, and obesity. Patients without SMI had higher rates of previous revascularization with PCI or CABG, rheumatologic disease, renal failure, valvular heart disease, and peripheral vascular disease. Cardiogenic shock was similar between non-SMI and SMI. Length of stay was longer in patients with SMI, and they were less likely to be discharged to home.
| Variable | Non-SMI (n = 3,029,194) ∗ | SMI (n=29,503) | p-value † | Schizophrenia (n=13,824) | Bipolar (n=16,913) |
|---|---|---|---|---|---|
| Age, years (mean ± SD) | 66.5 ± 14.9 | 59.6 ± 14.0 | <0.001 | 61.9 ± 14.2 | 57.5 ± 13.6 |
| Age (median, IQR) | 67.0 | 58.0 | <0.001 | 61.0 | 56.0 |
| Age (distribution by IQR) | <0.001 | ||||
| 18-55 | 25.3% | 42.2% | 36.1% | 47.9% | |
| 56-66 | 24.5% | 27.4% | 27.3% | 27.8% | |
| 67-78 | 25.2% | 18.7% | 21.9% | 15.8% | |
| ≥79 | 25.0% | 11.6% | 14.7% | 8.5% | |
| Female Sex | 38.0% | 44.1% | <0.001 | 42.8% | 44.7% |
| Race/ethnicity | <0.001 | ||||
| White | 78.4% | 77.4% | 67.3% | 52.1% | |
| Black | 8.1% | 13.5% | 20.1% | 16.1% | |
| Hispanic | 7.1% | 5.0% | 6.8% | 21.0% | |
| Asian | 2.2% | 1.1% | 1.6% | 6.6% | |
| Native American | 0.5% | 0.4% | 0.6% | 0.6% | |
| Anemia (iron-deficiency) | 11.6% | 13.0% | <0.001 | 14.8% | 11.7% |
| Congestive heart failure | 6.4% | 7.0% | <0.001 | 9.4% | 5.0% |
| Coagulopathy | 4.5% | 4.4% | 0.25 | 4.2% | 4.5% |
| Connective Tissue Disease | 1.9% | 1.4% | <0.001 | 1.0% | 1.7% |
| Chronic Pulmonary Disease | 18.2% | 27.4% | <0.001 | 28.4% | 26.8% |
| Depression | 4.9% | 8.3% | <0.001 | 10.2% | 6.4% |
| Diabetes | |||||
| Without complication | 23.2% | 27.9% | <0.001 | 28.3% | 27.6% |
| With complication | 3.9% | 4.1% | 0.13 | 3.9% | 4.4% |
| Fluid/Electrolyte Disorders | 20.2% | 26.4% | <0.001 | 32.6% | 21.3% |
| Hypertension | 56.4% | 54.9% | <0.001 | 51.9% | 57.4% |
| Liver Disease | 1.0% | 2.4% | <0.001 | 1.9% | 3.0% |
| Metastatic Cancer | 1.1% | 0.7% | <0.001 | 0.9% | 0.6% |
| Neurologic Disorders | 5.5% | 12.6% | <0.001 | 15.0% | 10.8% |
| Obesity | 8.5% | 11.8% | <0.001 | 9.4% | 13.7% |
| Prior coronary bypass | 4.5% | 2.8% | <0.001 | 1.8% | 3.4% |
| Prior coronary stent | 7.9% | 6.8% | <0.001 | 4.3% | 8.9% |
| Pulmonary Circulation Disorder | 0.7% | 1.0% | <0.001 | 1.0% | 1.1% |
| Peripheral Vascular Disease | 8.0% | 6.1% | <0.001 | 6.0% | 6.3% |
| Renal Failure | 10.6% | 9.1% | <0.001 | 10.1% | 8.1% |
| Hemodialysis | 0.3% | 0.3% | 0.007 | 0.2% | 0.3% |
| Substance Abuse | 4.2% | 13.2% | <0.001 | 11.8% | 14.8% |
| Valvular Disease | 1.7% | 1.2% | <0.001 | 1.4% | 1.0% |
| Weight Loss | 2.7% | 3.5% | <0.001 | 4.3% | 2.8% |
| Hospital Characteristics | |||||
| Payer | <0.001 | ||||
| Medicare | 53.2% | 58.5% | 66.6% | 52.1% | |
| Medicaid | 5.6% | 17.3% | 19.4% | 16.1% | |
| Private | 31.1% | 15.2% | 7.6% | 21.0% | |
| Self-Pay | 6.5% | 5.2% | 3.3% | 6.6% | |
| Hospital Size (by bed number) | <0.001 | ||||
| Small | 10.9% | 11.2% | 13.0% | 9.6% | |
| Medium | 23.4% | 24.5% | 24.9% | 24.1% | |
| Large | 65.7% | 64.3% | 62.0% | 66.2% | |
| Income Quartile (based on Hospital Zip Code) | <0.001 | ||||
| 1st (lowest) | 28.0% | 34.4% | 40.1% | 30.1% | |
| 2nd | 27.5% | 27.5% | 27.6% | 26.9% | |
| 3rd | 24.1% | 21.7% | 19.1% | 24.0% | |
| 4th (highest) | 20.3% | 16.4% | 13.2% | 19.0% | |
| Hospital Location | 0.7 | ||||
| Rural | 13.4% | 13.3% | 15.4% | 11.3% | |
| Urban | 86.6% | 86.7% | 84.6% | 88.7% | |
| Hospital Region | <0.001 | ||||
| Northeast | 17.7% | 20.6% | 21.8% | 19.5% | |
| Midwest | 23.9% | 24.1% | 24.7% | 23.9% | |
| South | 39.5% | 37.6% | 36.4% | 38.7% | |
| West | 18.9% | 17.6% | 17.0% | 18.0% | |
| Teaching Status | <0.001 | ||||
| Nonteaching | 55.6% | 53.5% | 54.1% | 53.0% | |
| Teaching | 44.4% | 46.5% | 45.9% | 47.0% | |
| Hospitalization | |||||
| Mean length of stay (days) | 5.6 ± 7.5 | 6.2 ± 8.2 | <0.001 | 7.2 ± 9.9 | 5.3 ± 6.3 |
| Cardiogenic Shock | 8.3% | 8.3% | 0.9 | 9.3% | 7.5% |
| Discharge status | <0.001 | ||||
| Home | 54.3% | 45.0% | 34.1% | 53.9% | |
| Transfer to short-term hospital | 10.3% | 10.4% | 9.3% | 11.3% | |
| Transfer to facility | 12.5% | 20.9% | 28.5% | 14.8% | |
| Home healthcare | 8.0% | 7.2% | 7.6% | 6.9% | |
| Against medical advice | 0.7% | 2.2% | 2.1% | 2.3% | |
| Died | 14.1% | 14.0% | 0.9 | 18.4% | 10.6% |
When SMI was separated into schizophrenia and bipolar disorder, further differences were observed. Notably, compared to patients without SMI, patients with schizophrenia were more likely to be of black race, whereas patients with bipolar were more likely to be black, Hispanic, or Asian. Compared with each other, patients with bipolar disorder were younger and more likely to be women. Multiple differences in co-morbidity burden and hospital characteristics were observed ( Table 1 ). Patients with schizophrenia were more likely to have CHF, chronic pulmonary disease, neurologic disorders, and renal failure, whereas patients with bipolar disorder were more likely to have hypertension, obesity, previous revascularization procedures, and substance abuse. In addition, patients with schizophrenia had higher rates of cardiogenic shock and were the least likely to be discharged to home.
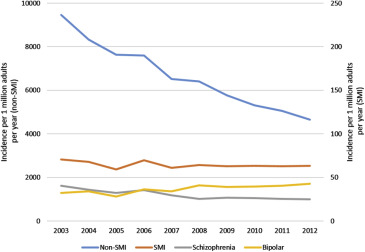
Over the study period of 2003 to 2012, the incidence of STEMI in the non-SMI population decreased 50%, from 9,455 to 4,652 per million adults per year (p for trend <0.001; Figure 1 ). In the SMI population, there was no statistically significant decrease in incidence of STEMI (from 71 to 64 per million adults per year, p for trend 0.14). Notably, although the incidence of STEMI decreased 39% in patients with schizophrenia (p for trend <0.001), it increased 33% in the bipolar disorder subgroup (p for trend = 0.002).
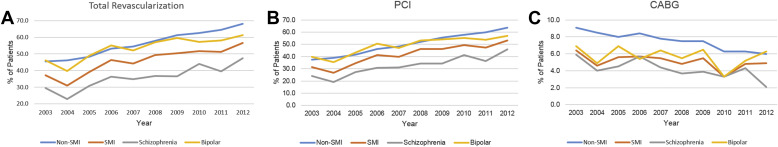
Revascularization procedures increased in all subgroups over the time period studied (p for trend <0.001). The crude rate of increase was lower in patients with SMI, especially in the schizophrenia subgroup ( Figure 2 ). When stratified by revascularization procedure, the rate of PCI increased in all subgroups (p for trend <0.001; Figure 2 ), although the crude rate was lower in SMI and schizophrenia. In contrast, CABG rates decreased in both the non-SMI cohort (p for trend <0.001) and the SMI cohort (p for trend 0.01; Figure 2 ). Within SMI, CABG rates did not significantly decrease in bipolar disorder (p for trend 0.37).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


