Heart rate variability (HRV) has been shown to be attenuated in patients with coronary artery disease (CAD) and may, therefore, be possibly used for the early detection of myocardial ischemia. We aimed to evaluate the diagnostic yield of a novel short-term HRV algorithm for the detection of myocardial ischemia in subjects without known CAD. We prospectively enrolled 450 subjects without known CAD who were referred to tertiary medical centers for exercise stress testing (EST) with single-photon emission computed tomography myocardial perfusion imaging (MPI). All subjects underwent 1-hour Holter testing with subsequent HRV analysis before EST with MPI. The diagnostic yield of HRV analysis was compared with EST, using MPI as the gold standard for the noninvasive detection of myocardial ischemia. All subjects had intermediate pretest probability for CAD. Mean age was 62 years, 38% were women, 51% had hypertension, and 25% diabetes mellitus. HRV analysis showed superior sensitivity (77%) compared with standard EST (27%). After multivariate adjustment, HRV was independently associated with an 8.4-fold (p <0.001) increased likelihood for the detection of myocardial ischemia by MPI, whereas EST did not show a statistically significant association with a positive MPI (odds ratio 2.1; p = 0.12). Of subjects who were referred for subsequent coronary angiography, the respective sensitivities of HRV and EST for the detection of significant CAD were 73% versus 26%. Our data suggest that HRV can be used as an important noninvasive technique for the detection of myocardial ischemia in subjects without known CAD, providing superior sensitivity to conventional EST in this population.
The diagnosis of coronary artery disease (CAD) resulting in myocardial ischemia often necessitates the use of either costly procedures that may expose the patient to ionizing radiation or of procedures limited by relatively low sensitivity and specificity. Heart rate variability (HRV) analysis is a noninvasive and relatively inexpensive test that does not expose the patient to ionizing radiation. It is based on the measurement of beat-to-beat variations and fluctuations, assessed by various statistical operations on normal R-R intervals. Previous studies have shown that HRV is correlated with the risk of all-cause mortality and cardiovascular and sudden cardiac death. Moreover, HRV was shown to be attenuated in patients with CAD, and it has been hypothesized that HRV analysis may be used to identify the existence of myocardial ischemia in subjects without known CAD. Few studies have assessed the use of HRV analysis for the detection of ischemia, with somewhat conflicting results. However, these studies were limited by heterogeneous populations and using long-term end points of cardiovascular events or death rather than the presence of myocardial ischemia at the time of HRV testing. We developed a new HRV algorithm that showed a high sensitivity for the detection of myocardial ischemia in a small pilot study. Here we report the results of a prospective, multicenter, clinical trial designed to validate the diagnostic yield of the HRV algorithm in subjects without known CAD.
Methods
The HeartTrends HRV Algorithm for the Detection of Myocardial Ischemia is a prospective clinical trial designed to evaluate the yield of HeartTrends, a novel HRV algorithm of a short-term Holter electrocardiogram, for the detection of myocardial ischemia in subjects without known CAD who were referred for exercise myocardial perfusion imaging (MPI). The study was conducted in 2 tertiary referral centers in Israel. Subjects enrolled were >21 years without known CAD who were referred by their physician for noninvasive assessment through MPI. Subjects were excluded if they had any of the following exclusion criteria: established CAD, atrial fibrillation or flutter, the diagnosis of an acute coronary syndrome, the presence of a cardiac pacemaker, clinical diagnosis of heart failure, moderate or severe pulmonary disease, acute myocarditis or any presence of cardiomyopathy, known drug or alcohol dependence, the presence of left bundle branch block, significant intraventricular conduction delay, or significant (>1 mm) ST deviations at baseline.
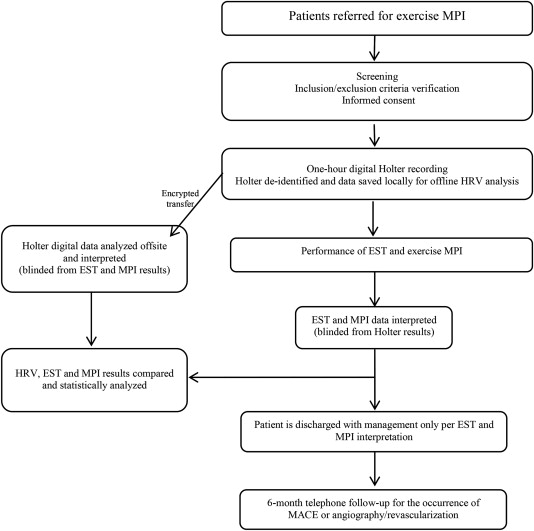
Subjects meeting inclusion criteria who provided informed consent to participate in the study underwent 1-hour digital electrocardiographic (ECG) Holter data acquisition before the planned nuclear stress test. After data acquisition, subjects underwent a standard exercise stress test and a nuclear scan according to accepted performance criteria (mean time interval between Holter and nuclear stress testing: 30 ± 15 minutes). Analysis of recorded ECG data for HRV was performed blinded to the exercise stress testing (EST) and MPI results, off-line at an ulterior date. All subjects were further followed for clinical events and interventions at 6 months. A summary of the study design is provided in Figure 1 .
The study was approved by the institutional review boards of the participating centers, and all subjects provided informed consent. Enrollment was initiated on July 1, 2012, and the study was terminated on March 1, 2014, with the final study population comprising 450 patients.
HRV acquisition is done by extracting R-R interval duration from a digital Holter electrocardiogram and further analyzing it by the Lev El Diagnostics of Heart Diseases novel patented and patent-pending algorithms. The ECG equipment used is simply an off-the-shelf Holter ECG device as HeartTrends algorithm is compatible with any device that includes the following standard characteristics. Once the Holter provides the “clean” RR time series, the HeartTrends runs its patented algorithm that results in the Dy/Dx indicator value. A detailed description of how to measure Dy/Dx has been published. Briefly, the Multipole analysis is a new way of investigating the Poincaré Plot from complex time series. The measures obtained from this kind of analyses bear intrinsic time dependence because of the very construction of the plot, as opposed to the SD of NN intervals, which does not include any time ordering. As a result Dy/Dx, as do other Poincaré plot indexes, derives information from both the time and frequency domains and reflecting increased randomness in the RR interval time series.
EST was defined as positive when there was a ≥1 mm of horizontal or downsloping ST-segment depression ≥80 milliseconds after the J-point (compared with the level of the PQ interval) for 3 consecutive beats or ST-segment elevation ≥1 mm in a non–Q wave lead other than V1 or AVR. All other EST results were considered to be negative for myocardial ischemia. HRV analysis was defined as positive when the Dy/Dx indicator value score generated by the HeartTrends device using a proprietary algorithm was <2.0, based on calibration analyses that were carried out in a pilot study. “MPI” was defined as positive when the amount of myocardial ischemia was >5% of the myocardium.
EST and MPI tests were adjudicated separately, each by 2 independent observers, blinded to the results of all other tests. Similarly, coronary angiograms performed during follow-up were reviewed and adjudicated by 2 independent observers, blinded to the results of all other tests.
We compared the diagnostic yield of the new HeartTrends HRV algorithm with the commonly used EST. MPI was used as the gold standard for the detection of a significant CAD. The sample size was calculated to show a 10% superiority of the new HRV algorithm compared with standard EST. The expected sensitivity of HeartTrends HRV testing for the gold standard exercise imaging tests is >70% compared with 60% using EST, with a corresponding 10% difference in the negative predictive value and specificity between the 2 screening techniques. Accordingly, a minimal required sample size of 450 total subjects (for a power of 0.9 and alpha of 0.05) was calculated, adjusting for an expected 5% rate of unusable Holter recordings.
Continuous variables were compared using t test and expressed as mean ± SD. Categorical variables were assessed using the chi-square test or Fisher’s exact test, when at least one of the cells in the table had an expected number <5. For diagnostic yield assessment, we calculated the test’s sensitivity, specificity, positive predictive value, and negative predictive value.
Multivariate logistic regression modeling was used to assess the likelihood for the identification of myocardial ischemia by HRV and EST. Prespecified covariates in the multivariate models included age, gender, hypertension, dyslipidemia, diabetes mellitus, body mass index, current smoking, and a family history of CAD. Analyses were performed using the SAS software (SAS Institute Inc. Cary, NC) (version 9.30).
Results
Of the 450 subjects enrolled in the study, 47 had uninterpretable Holter ECG recordings (<1 hour), 5 did not complete EST, and 4 were ultimately found to have 1 or more exclusion criteria, thus resulting in a final analysis sample of 394 subjects. The baseline clinical characteristics and medications of study subjects are presented in Table 1 . Notably, the characteristics of the subjects who were included in the final analysis were similar to those who were excluded. Mean age was 62 years (±10) and 62% were men. All subjects had an intermediate pretest probability for CAD, with a relatively high frequency of cardiovascular risk factors, including hypertension and diabetes mellitus ( Table 1 ).
| Characteristic | Included in the final analysis (N=394) | Excluded from the final analysis (N=56) |
|---|---|---|
| Age (years) | 62 ± 10 years | 63 ± 12 years |
| Men | 62 % | 63 % |
| Hypertension † | 51 % | 50 % |
| Dysplipidemia † | 66 % | 68 % |
| Diabetes Mellitus | 25 % | 23 % |
| Family history of coronary artery disease | 44 % | 46 % |
| Peripheral vascular disease | 2 % | 1 % |
| Prior cerebrovascular accident or transient ischemic attack | 2 % | 2 % |
| Smoker | ||
| Past | 18 % | 16 % |
| Present | 22 % | 24 % |
| Body mass index (kg/m 2 ) | 28 ± 5.4 | 29 ± 6 |
| Medications | ||
| Beta blockers ‡ | 14 % | 13 % |
| Calcium channel blockers | 11 % | 13 % |
| Antiarrhythmics | 0.3 % | 0 % |
∗ Data are as percentages or mean ± SD; all p-values for the comparison between the two groups are >0.10.
† Hypertension and dyslipidemia were defined if subjects were receiving antihypertensive and lipid lowering therapies, respectively.
‡ Treatment with beta blockers was withheld 48 hours prior to start of study procedures.
Myocardial ischemia was detected using MPI in 7% of the study cohort. Ischemia was detected in various territories (left anterior descending, diagonal branch, and left circumflex) and ranged in magnitude from mild (5% to 10% of myocardium), moderate (10% to 20% of myocardium), or severe (>20% of myocardium).
The diagnostic parameters of the new HRV algorithm and of conventional EST for the study population are presented in Table 2 . The HRV test showed a markedly higher sensitivity for the detection of myocardial ischemia compared with EST (77% vs 27%). In addition, the negative predictive value of the HRV test was very high (98% compared with 94% associated with conventional EST), whereas the specificities and positive predictive values of the 2 tests were similar ( Table 2 ). Notably, the diagnostic yield of the HRV test was independent of the daily hour in which it was obtained.



