Although exercise treadmill testing (ETT) is a useful initial test for patients with suspected cardiovascular (CV) disease, there is concern regarding the use of downstream imaging tests especially in the setting of equivocal or positive ETTs. Patients with no history of coronary artery disease who underwent ETT between 2009 and 2010 were prospectively included. Referring physicians were categorized as cardiologists and noncardiologists. Downstream tests included nuclear perfusion imaging, coronary computed tomography angiography, stress echocardiography, stress magnetic resonance, and invasive coronary angiography performed up to 6 months after the ETT. Patients were followed for CV death, myocardial infarction, and coronary revascularization for a median of 2.7 years. Among 3,656 patients, the ETT were negative in 2,876 (79%), positive in 132 (3.6%), and inconclusive in 643 (18%). Cardiologists ordered less downstream tests than noncardiologists (9.5% vs 12.2%, p = 0.02), with less noninvasive tests (5.9% vs 10.4%, p <0.0001) and more invasive angiography (3.6% vs 1.8%, p <0.0001). After adjustment for confounding, patients evaluated by cardiologists were less likely to undergo additional testing after equivocal (odds ratio: 0.65, p = 0.02) or positive ETT results (odds ratio: 0.39, p = 0.02), whereas after negative ETT, the odds ratio was 1.7 (p = 0.06). There was no difference in the rate of adverse CV events between patients referred by cardiologists versus noncardiologists. In conclusion, patients referred for ETT by cardiologists are less likely to undergo additional testing, particularly noninvasive tests, than those referred by noncardiologists. The lower rate of tests is driven by a lower rate of tests after positive or inconclusive ETT.
Exercise treadmill testing (ETT) is commonly performed to evaluate patients with chest pain who are able to exercise and have a normal baseline electrocardiogram (ECG). Because of its widespread availability, ETT is routinely ordered by the cardiologists and noncardiologists for a wide range of clinical indications. However, appropriate interpretation of ETT results is not always simple, and previous experience and training may affect how the test results are integrated with other clinical information into a management plan. The expanded use of advanced noninvasive imaging tests has led to growing concerns about the increased use of cardiovascular (CV) testing. Although medical societies have developed appropriate use criteria to address these concerns, preliminary data show that they do not reduce the utilization of inappropriate tests. Recognizing the need for other methods to reduce overutilization of testing, some studies have evaluated the impact of patient characteristics on the use of CV imaging tests. However, there is limited data evaluating the contribution of physician specialty as a source of variability in the use of CV imaging tests. Therefore, we sought to evaluate the impact of physician specialty on the use of additional cardiac testing after ETT.
Methods
We prospectively collected data on all consecutive patients older than 18 years who underwent clinically indicated ETT between January 1, 2009 and December 31, 2010 at Brigham and Women’s Hospital, in Boston, Massachusetts. The study excluded patients with previous diagnoses of coronary artery disease (CAD) (defined as previous coronary artery bypass grafting, percutaneous coronary intervention, and myocardial infarction [MI]) and patients with nonclinical indications for testing such as exercise prescription, participation in a research protocol, and post–heart transplant evaluation. The Partners Healthcare Institutional Review Board approved this study.
Information on demographics, clinical history, risk factors, medications, and indications for testing was collected using a standardized patient interview and confirmed by review of each patient’s longitudinal electronic medical record. We estimated the pretest probability of CAD using the Morise score. Each physician initiating the referral for an ETT was then categorized as a cardiologist or noncardiologist. Noncardiologists included primary care/internal medicine physicians and other specialists.
ETTs were performed using a symptom-limiting Bruce protocol according to the established guidelines as part of routine clinical care. The target heart rate was determined as 85% of the maximum predicted heart rate, which equals 220 − age. All ST segment deviations were assessed 80 ms after the J point. The Duke treadmill score was calculated for each patient as: exercise time (minutes) – (5 × maximal ST segment depression in millimeter) – (4 × angina index; 0, no angina; 1, angina; 2, angina as reason for stopping test).
We categorized each test results as positive, negative, or inconclusive. Positive tests were defined as upsloping ST depressions ≥ 1.5 mm or downsloping or horizontal depressions ≥ 1.0 mm in at least 2 contiguous ECG leads. Inconclusive tests included any result that may be interpreted as indeterminate and comprised the following categories: (1) negative ECG with reduced sensitivity because of submaximal exercise (<85% maximum predicted heart rate and rate pressure product < 25,000); (2) positive ECG with reduced specificity because of baseline ECG abnormalities; (3) positive ECG with reduced specificity because of rapid recovery of ECG changes; (4) typical anginal symptoms or (5) inappropriate dyspnea despite a negative ECG findings, and (6) clinically significant rhythm disturbances (any sustained arrhythmia or >3 beats of ventricular tachycardia).
For each patient, we identified the use of all noninvasive imaging and invasive angiography tests performed within 6 months after ETT through review of the electronic medical record. We chose the 6-month cutoff to capture any downstream testing that was likely triggered by the ETT results.
We included all possible subsequent noninvasive imaging tests available at our institution: nuclear stress tests, stress echocardiograms, coronary computed tomography (CT) angiography, and stress magnetic resonance imaging. All tests were performed and reported according to institutional protocols. We categorized all nuclear stress test (positron emission tomography and single-photon emission CT) results as follows: negative, for normal test results; equivocal for “inconclusive” or “negative with reduced exercise capacity”; and positive for “abnormal” or “probably abnormal” results. We categorized the coronary CT angiography results as negative for reports of no plaque or stenosis ≤50% and positive for stenosis >70% (or >50% in the left main coronary). We defined as inconclusive for the evaluation of ischemia any studies that were uninterpretable or had moderate (51% to 70%) stenosis, given that such lesions may not be associated with ischemia and have uncertain hemodynamic significance. We categorized cardiac magnetic resonance results as negative if no ischemia was detected, equivocal if image quality precluded interpretation, and positive if ischemia was identified. We categorized the results of echocardiograms as positive, negative, or equivocal based on the presence or absence of stress-induced wall motion abnormalities. Equivocal tests were defined as ones in which reduced image quality limited the evaluation or if patients failed to achieve 85% of the maximum predicted heart rate.
We defined obstructive CAD as a stenosis ≥50% in the left main coronary artery or ≥70% in any other coronary vessel.
We reviewed all patient charts to identify incident nonfatal MI and coronary revascularizations, which comprised all percutaneous coronary interventions and coronary artery bypass graft procedures. MI was defined using universal criteria.
We determined patients’ vital status using the Social Security Death Index and the cause of death using chart review, autopsy findings, and hospice notes where available. If the chart lacked information to determine the cause of death, we used death certificates obtained from the Massachusetts Registry of Vital Records and Statistics. Two cardiologists blinded to all clinical information and test results adjudicated the cause of death for each patient. CV death was defined as acute MI, atherosclerotic coronary vascular disease, congestive heart failure, valvular heart disease, arrhythmic heart disease, or stroke. Major adverse CV events were the combined outcome of CV death, nonfatal MI, and coronary revascularization.
Continuous variables are expressed as the mean ± SD or median and interquartile range, as appropriate. Categorical variables are presented as frequencies. Differences between groups were tested using chi-square or Fisher’s exact tests for discrete variables and 1-way analysis of variance for continuous variables. The analysis of the rate of second testing was performed with the estimation of univariable and multivariable logistic regressions. To adjust for confounding on variables that may influence the use of downstream testing, we built multivariable logistic regression models including age, gender, number of risk factors, symptoms, and ETT results. Separate models were developed for (a) all downstream testing, (b) noninvasive testing, and (c) invasive testing. To evaluate for effect modification of ETT results between cardiologists and noncardiologists, interaction terms were included in the models and reported when significant. To compare CV outcomes, we calculated the annualized rate of CV death, MI, and coronary revascularization and the combined outcome that includes any of these 3 events. All tests were 2 sided, and p <0.05 was considered statistically significant. Statistical analysis was performed using Stata, version 12, Statacorp (College Station, Texas).
Results
Among 4,262 consecutive patients referred for ETT during the study period, we excluded 509 patients with previous CAD, 9 patients younger than 18 years, and 88 patients who underwent ETT for indications other than evaluation of CAD, such as a research protocol or post–heart transplantation. The final study population included 3,656 patients, all of which had complete follow-up for CV death. Follow-up data for incident MI or coronary revascularization were available for 3,345 (91.4%) patients. Patients with incomplete follow-up for incident MI or coronary revascularization achieved higher MET, had a higher Duke Treadmill score, and were less likely to have typical angina symptoms.
The baseline characteristics of the patient population (age 54 [13] years, 46% men) stratified by specialty of the physician initiating the referral to ETT are presented in Table 1 . Among all patients referred for ETT, 1,058 (29%) were referred by cardiologists, whereas 2,598 (71%) were referred by noncardiologists. Although patients referred by cardiologists were older and more likely to be men, they had a lower prevalence of diabetes and hypertension and lower BMI. Accordingly, patients referred by cardiologists had a lower probability of CAD by the Morise score (29.8% [22.0%] vs 36.5% [21.1%], p <0.0001).
| Variable | All n = 3656 | Cardiologists n = 1058 (29%) | Non-Cardiologist n = 2598 (71%) | p-Value |
|---|---|---|---|---|
| Men | 1681 (46%) | 552 (52%) | 1129 (43%) | <0.0001 |
| Age (years) | 53.6 ± 13.2 | 54.7 ± 11.9 | 51.1 ± 15.9 | <0.0001 |
| Hypertension ∗ | 1681 (46%) | 450 (43%) | 1231 (47%) | 0.008 |
| Diabetes mellitus | 470 (13%) | 96 (9%) | 374 (14%) | <0.0001 |
| Hyperlipidemia † | 1537 (42%) | 461 (44%) | 1076 (41%) | 0.23 |
| Smoker | 468 (13%) | 120 (11%) | 348 (13%) | 0.09 |
| Body mass index (kg/m 2 ) | 28.2 (6.5) | 26.9 (5.9) | 28.7 (6.6) | <0.0001 |
| Morise score | 10.4 (4.5) | 9.3 (4.8) | 10.9 (4.3) | <0.0001 |
| Symptoms | <0.0001 | |||
| Asymptomatic | 214 (6%) | 89 (8%) | 125 (5%) | |
| Non-anginal chest pain | 1676 (46%) | 275 (26%) | 1401 (54%) | |
| Atypical chest pain | 297 (8%) | 39 (4%) | 258 (10%) | |
| Typical chest pain | 241 (7%) | 53 (5%) | 188 (7%) | |
| Dyspnea or other symptoms | 1228 (34%) | 602 (56%) | 626 (24%) | |
| Medications at baseline | ||||
| Statins | 1045 (29%) | 314 (29%) | 731 (28%) | 0.34 |
| Aspirin | 1103 (30%) | 289 (27%) | 814 (31%) | 0.01 |
| β blocker | 746 (20%) | 285 (27%) | 461 (18%) | <0.0001 |
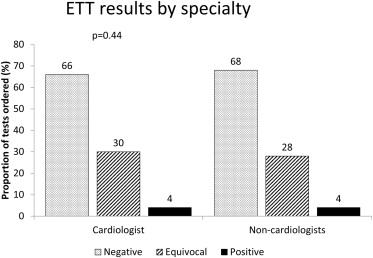
| Exercise test results | 0.44 | |||
| Negative | 2478 (68%) | 701 (66%) | 1777 (68%) | |
| Equivocal | 1043 (28%) | 317 (30%) | 726 (28%) | |
| Positive | 135 (4%) | 40 (4%) | 95 (4%) | |
| MET | 10.8 (4.3) | 11.8 (4.1) | 10.4 (4.3) | <0.0001 |
| Duke score | 8.6 (5.2) | 9.5 (4.9) | 8.3 (5.3) | <0.0001 |
| Symptoms during ETT | <0.0001 | |||
| None | 2420 (66%) | 757 (72%) | 1663 (64%) | |
| Typical angina pectoris | 150 (4%) | 38 (4%) | 112 (4%) | |
| Atypical angina pectoris | 184 (5%) | 26 (3%) | 158 (6%) | |
| Dyspnea | 459 (13%) | 108 (10%) | 351 (14%) | |
| Other symptoms | 443 (12%) | 129 (12%) | 314 (2%) | |
∗ Hypertension was defined as a systolic blood pressure > 140 mm Hg, diastolic blood pressure > 90 mm Hg, or diagnosis/treatment of hypertension.
† Hyperlipidemia was defined as total cholesterol > 240 mg/dl or high-density lipoprotein cholesterol < 40 mg/dl (men) or <50 mg/dl (women) or diagnosis/treatment of dyslipidemia.
There was no significant difference in ETT results when ordered by cardiologists vs noncardiologists ( Figure 1 ). However, patients referred by cardiologists achieved higher MET (11.8 [4.1] vs 10.4 [4.3], p <0.0001) and had a higher Duke Treadmill score (9.5 [4.9] vs 8.3 [5.3], p <0.0001) ( Table 1 ).
Patients who had the ETT ordered by a cardiologist underwent less downstream testing (9.5% vs 12.2%, p = 0.02) ( Figure 2 ). This difference was driven by a lower rate of noninvasive imaging (5.9% vs 10.4%, p <0.001). However, the rate of downstream invasive angiography was higher among patients initially evaluated by cardiologists (3.6% vs 1.8%, p = 0.001).
As expected, downstream utilization of all tests was lowest after a negative ETT and highest after a positive ETT irrespective of physician specialty ( Figure 2 ). However, the relative frequency of downstream testing was different between cardiologists and noncardiologists. In the setting of a negative ETT result, there was no significant difference in downstream testing between cardiologists and noncardiologists (3.0% vs 2.3%, respectively, p = 0.21; Figure 2 ). After an equivocal ETT, however, cardiologists ordered significantly less additional testing (18.0% vs 28.0%, p = 0.001; Figure 2 ). Similarly, the rate of downstream testing after a positive ETT was lower in patients referred by cardiologists (76.9% vs 52.5%, p = 0.005; Figure 2 ).
When specifically evaluating the rate of downstream noninvasive imaging tests, there was a lower rate for those initially evaluated by cardiologists when the ETT results were equivocal (10.7% vs 26.5%, p <0.0001) or positive (25.0% vs 45.3%, p = 0.004) but not significantly different when the ETT results were negative (2.6% vs 2.0%, p = 0.35) ( Table 2 ).
| All (n = 3656) | Downstream Testing | p-Value | ||
|---|---|---|---|---|
| No n = 3240 (89%) | Yes n = 416 (11%) | |||
| Men | 1681 (46%) | 1488 (46%) | 193 (46%) | 0.86 |
| Age (years) | 53.6 ± 13.0 | 53.0 ± 13.3 | 59.0 ± 11.6 | <0.0001 |
| Hypertension ∗ | 1681 (46%) | 1460 (45%) | 221 (53%) | 0.002 |
| Diabetes | 470 (13%) | 395 (12%) | 75 (18%) | 0.001 |
| Hyperlipidemia † | 1537 (42%) | 1330 (41%) | 207 (50%) | 0.001 |
| Smoker | 468 (13%) | 408 (13%) | 60 (14%) | 0.29 |
| Body mass index (kg/m 2 ) | 28.2 (6.5) | 28.2 (6.5) | 27.7 (6.8) | 0.14 |
| Morise score | 10.4 (4.5) | 10.2 (4.5) | 12.1 (4.3) | <0.0001 |
| Symptoms | <0.0001 | |||
| Asymptomatic | 214 (6%) | 196 (6%) | 18 (4%) | |
| Non-anginal pain | 1676 (46%) | 1505 (46%) | 171 (42%) | |
| Atypical chest pain | 297 (8%) | 259 (8%) | 38 (9%) | |
| Typical chest pain | 241 (7%) | 185 (6%) | 56 (13%) | |
| Dyspnea or other symptoms | 1228 (33%) | 1095 (34%) | 133 (32%) | |
| Medications at baseline | ||||
| Statins | 1045 (29%) | 887 (27%) | 158 (38%) | <0.0001 |
| Aspirin | 1103 (30%) | 939 (29%) | 164 (39%) | <0.0001 |
| β blocker | 746 (20%) | 648 (20%) | 98 (24%) | 0.09 |
| Exercise test results | <0.0001 | |||
| Negative | 2478 (68%) | 2416 (75%) | 62 (15%) | |
| Equivocal | 1043 (28%) | 785 (24%) | 258 (62%) | |
| Positive | 135 (4%) | 41 (1%) | 94 (23%) | |
| METs | 10.8 (4.3) | 11.0 (4.4) | 9.3 (3.3) | <0.0001 |
| Duke score | 8.6 (5.2) | 9.2 (4.3) | 3.7 (8.5) | <0.0001 |
| Symptoms during ETT | <0.0001 | |||
| None | 2420 (66%) | 2218 (68%) | 202 (48%) | |
| Typical angina | 150 (4%) | 69 (2%) | 81 (19%) | |
| Atypical angina | 184 (5%) | 171 (5%) | 13 (3%) | |
| Dyspnea | 459 (13%) | 366 (11%) | 93 (22%) | |
| Other symptoms | 443 (12%) | 416 (13%) | 27 (6%) | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


