Left atrial (LA) volume is an important prognostic factor in cardiovascular disease. Multidetector computed tomography (MDCT) is an emerging cardiac imaging modality; however, its accuracy in measuring the LA volume has not been well studied. The aim of our study was to determine the accuracy of MDCT in quantifying the LA volume. A total of 48 patients underwent MDCT and 2-dimensional (2D) echocardiography (2DE) on the same day. The area–length and Simpson’s methods were used to obtain the 2D echocardiographic LA volume. The LA volume assessment by MDCT was obtained using the modified Simpson’s method. Four artificial phantoms were created, and their true volume was assessed by an independent observer using both imaging modalities. The correlation between the LA volume by MDCT and 2DE was significant (r = 0.68). The mean 2D echocardiographic LA volume was lower than the LA volume obtained with MDCT (2DE 79 ± 37 vs MDCT 103 ± 32, p <0.05). In the phantom experiment, the volume obtained using MDCT and 2DE correlated significantly with the true volume (r = 0.97, p <0.05 vs r = 0.96, p <0.05, respectively). However, the mean 2D echocardiographic phantom volume was 16% lower than the true volume (2DE, Simpson’s method 53 ± 24 vs the true volume 61 ± 24, p <0.05). The mean volume calculated using MDCT did not differ from the true volume (MDCT 60 ± 21 vs true volume 61 ± 24, p = NS). 2DE appeared to systematically underestimate the LA volume compared to phantom and cardiac MDCT, suggesting that different normal cutoff values should be used for each modality. In conclusion, LA volume quantification using MDCT is an accurate and feasible method.
Calculations of left atrial (LA) volume using 2-dimensional (2D) echocardiography (2DE) have relied on geometric assumptions implicit in formulas such as Simpson’s rule and area–length models, often leading to inaccurate LA volume quantification. Although computed tomography uses the Simpson’s method, similar assumptions that might be made are somewhat corrected by using a 3-dimensional (3D) data set. Cardiac multidetector computed tomography (MDCT) is an emerging cardiac imaging tool, with the capability for full volumetric image acquisition. Previous studies have shown an excellent correlation between MDCT and echocardiography regarding left ventricular volume quantification. Differences in chamber volume assessment by MDCT and 2DE have been postulated to result from either underestimation by 2DE or overestimation by MDCT. The aim of our study was to correlate the 2D echocardiographic and multidetector computed tomographic measurement of the LA volume and to determine the accuracy of both imaging modalities compared to the true volume derived from artificial phantoms.
Methods
Patients aged ≥18 years who had been referred for clinically indicated echocardiography and MDCT were eligible for inclusion. Patients with renal insufficiency (serum creatinine value >1.4 mg/dl), dyspnea precluding a 10- to 15-second breath hold, implanted defibrillators or pacemakers, or a history of allergy to iodinated contrast were excluded.
Both imaging techniques were performed within 24 hours. The institutional review board waived the requirement for written informed consent. The local ethics board of the Massachusetts General Hospital approved the study. A total of 48 patients (age 55 ± 19 years, 58% men) underwent MDCT and 2DE. The area–length method and Simpson’s method were used to obtain the 2D echocardiographic LA volumes by 2 independent readers ( Figure 1 ).
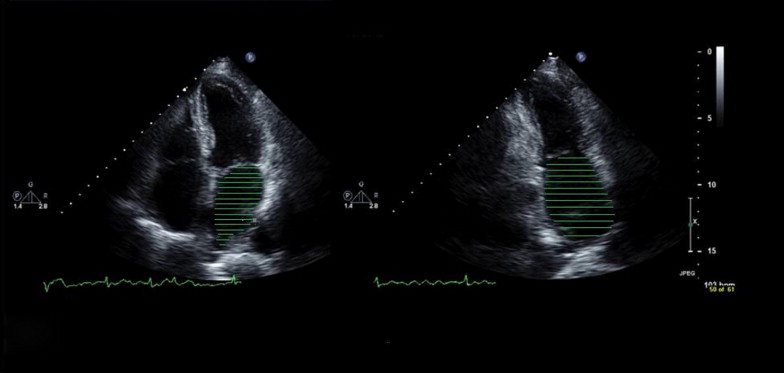
All patients underwent 2DE using a standard institutional protocol with a 3.5-MHz array transducer to obtain the parasternal long-axis, apical 2-chamber, and apical 4-chamber views of the left atrium (performed using Philips IE33, Andover, Massachusetts). The images were stored in digital format for off-line analysis. A single reader, unaware of the results of the multidetector computed tomographic study, measured the LA volumes using the American Society of Echocardiography recommendations for chamber quantification. The average heart rate during 2DE was 75 ± 10 beats/min. Simpson’s method (areas obtained in both apical 2-chamber and apical 4-chamber views) and the area–length method were used for LA quantification by 2DE. It has been shown that LA volumes are best estimated using either Simpson’s method or the biplane area–length formula.
All subjects underwent MDCT with a 64-slice multidetector row scanner (Sensation 64, Siemens Medical Solutions, Forchheim, Germany). An intravenous β blocker was administered 5 minutes before the scan in patients with a baseline heart rate >65 beats/min. The average heart rate during computed tomographic measurement was 65 ± 8 beats/min. After an initial scout image and a timing bolus scan, a volume data set was acquired (64 × 0.6 mm collimation, gantry rotation time 330 ms, table feed 3.8 mm/rotation, tube voltage 120 kV, tube current 300 to 950 mA, depending on patient size), covering the distance from the carina to the diaphragm. The contrast agent iopamidol (Isovue, Bracco Diagnostics, Princeton, New Jersey; 300 mg I/ml, mean volume 83 ± 10 ml) was administered at 5 ml/s, with a delay calculated according to a timing bolus scan. The contrast injection was immediately followed by 50 ml of saline at a rate of 5 ml/s. Dose modulation was used to minimize radiation without interfering with the end-systolic and end-diastolic frames to obtain the maximum LA sizes.
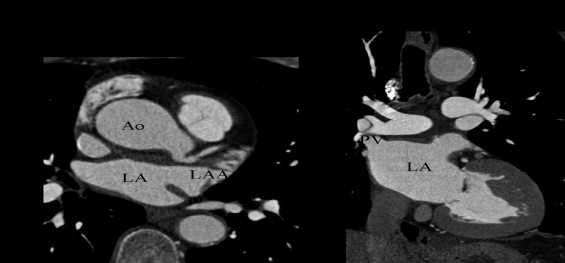
Axial images were analyzed on a dedicated workstation (Leonardo, Siemens Medical Solution) for assessment of the LA volumes. Images were reconstructed with a slice thickness of 0.75 mm (reconstruction kernel B25f) using a retrospective electrocardiogram-gated half-scan algorithm. With this approach, a temporal resolution of 165 ms in the center of the gantry rotation could be achieved. A data set consisting of axial images reconstructed at 10% of the R-R interval, corresponding to the left ventricular end-systolic phase, was loaded into volume calculation software. The LA volumes by MDCT were calculated at left ventricular end-systole using a stack of consecutive, nonoverlapping, 10-mm-thick, multiplanar, reformatted images reconstructed from true 3D pixel-based data in the short axis of the left atrium. This was performed using modified Simpson’s method by 2 independent observers. The endocardial border of the left atrium was manually traced, while excluding the LA appendage and pulmonary veins at the ostia. One axial view was used as a reference image, where we could visualize the left atrial appendage and 8 to 12 axial images were traced from the pulmonary veins to the mitral annulus. The full analysis took approximately 6 ± 2 minutes ( Figure 2 ).
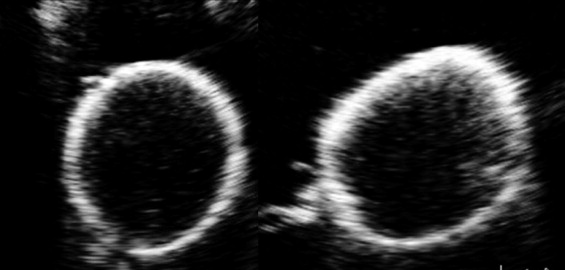
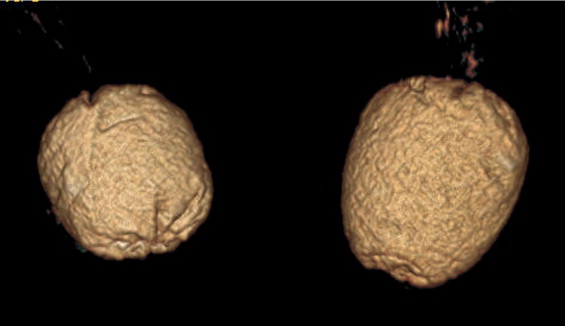
Artificial phantoms were created from a double-layer of latex rubber sheaths, and 4 balloons of varying sizes were created. Known volumes of degassed water mixed with iodinated x-ray contrast (Ultravist, 320 mg/dl, 1:50 volume dilution for imaging under cardiac computed tomography; Bayer Healthcare, Leverkusen, Germany) were measured with a graduated cylinder and poured into the inner latex sheath to form each LA cavity. LA cavity volumes ranging from 34 to 92 ml were created in 4 separate phantoms. Two blinded readers analyzed the phantom volume using 2DE and MDCT on the same day ( Figures 3 and 4 ). A third reader quantified the true volume.
The intertechnique agreement between the multidetector computed tomographic and 2D echocardiographic-derived LA volumes were evaluated using linear regression analysis with Pearson’s correlation coefficient and Bland-Altman analysis. The reproducibility of LA volume quantification by both imaging modalities was evaluated by calculating the interobserver variability of each technique. The Statistical Package for Social Sciences statistical software (SPSS, Chicago, Illinois) was used. The Program for Epidemiologists (PEPI) analysis was used to compare Pearson’s correlation values between the 2 imaging modalities.
Results
The main indications for cardiac imaging in our study were angina pectoris, followed by coronary artery disease ( Table 1 ). The LA volume assessment by MDCT and 2DE correlated significantly in the 48 patients was significant (r = 0.68, p <0.05); however, the mean 2D echocardiographic LA volume was 29% lower than that measured using MDCT: (2DE, area–length method, 82 ± 36 vs MDCT, 103 ± 32, p <0.05) and (2DE, Simpson’s method, 79 ± 37 vs MDCT, 103 ± 32, p <0.05). The Bland-Altman plot showed systematic underestimation of LA volume by 2DE ( Figure 5 ).



